Whipple's disease (WD) is a multisystem infection caused by Tropheryma whipplei (T. whipplei). Associated neurological symptoms are common, although they rarely appear as the initial manifestation of the disease. They are often related to disease limited to the CNS.1
We present a case of a 30-year-old woman who presented at the emergency department with neck pain accompanied by frontal headache and tingling and clumsiness in the left arm and left side of the face. The patient attributed symptoms to a motor vehicle accident with no head trauma that had taken place 2 weeks before. Additionally, she reported some drowsiness and difficulty speaking. The patient's medical history was not relevant except for her residence in a rural area. Physical examination revealed dysarthria, minimal claudication in the upper left limb, and paraesthesia of the left hand without loss of sensitivity. Complete blood count, biochemical analysis, and other conventional laboratory tests yielded normal results.
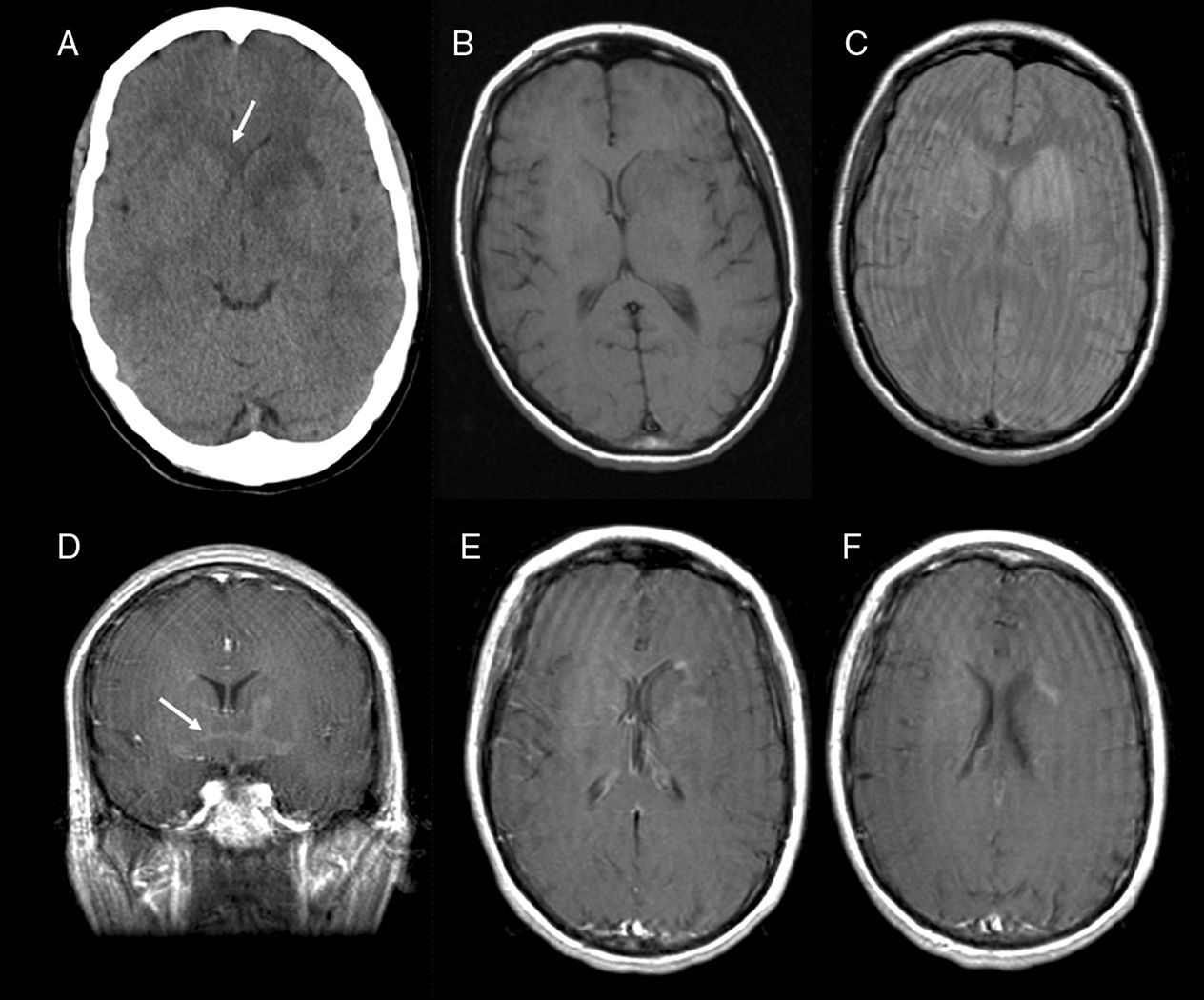
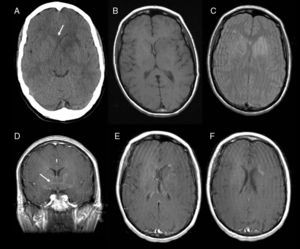
Doctors performed an emergency cranial computed tomography without contrast that showed a hypodense area affecting the caudate nucleus and globus pallidus, the anterior limb of the left internal capsule, and the anterior part of the left external capsule (Fig. 1).
CT without contrast (A) performed upon arrival of the patient shows a hypodense area affecting the left caudate and lentiform nuclei and the internal capsule. Note the hypodense area extending contralaterally along the edge of the corpus callosum. MR images taken 18hours later revealed hypointensities in the same regions described by the CT scan in T1-weighted sequences and hyperintensity in DP-weighted sequences. Administration of paramagnetic contrast (D–F) yielded distinct, heterogeneous and mainly peripheral areas of enhancement clearly showing the lesion's contralateral extension through the anterior commissure (arrow in D).
Cranial MRI scans performed with and without contrast 12hours after the patient was admitted showed signal alterations in both caudate nuclei, left lentiform nucleus, genu of the corpus callosum, and anterior commissure; changes were more pronounced on the left side. Lesions showed expansile tendencies and faint, irregular enhancement after administration of contrast (Fig. 1).
During the hospital stay, the patient was studied using thoracic, abdominal, and pelvic CT with both oral and intravenous contrast. Scans did not reveal any relevant findings. Lumbar puncture was used to extract cerebrospinal fluid for analysis, and all results from both cytology studies and serology studies (for the most common pathogens) were normal.
Given the patient's progressively worsening condition (abulia, hypersomnia, urinary incontinence, Babinski sign, and claudication of the lower limbs), doctors decided to perform a stereotaxic brain biopsy of the lesion adjacent to the right caudate nucleus. The anatomical pathology study of the sample showed areas of gliosis and hypercellularity caused by numerous macrophages with clear cytoplasm and granular PAS-positive structures that suggested CNS impairment due to WD. Tissue and serum samples were analysed using the polymerase chain reaction method; serum was negative for T. whipplei.
In light of these results, doctors performed a lower gastrointestinal series and digestive tract endoscopy with a duodenal biopsy. Tests revealed no signs of extracranial Whipple disease.
The patient was treated with 2g IV ceftriaxone every 12hours; treatment was tolerated well and the patient's status improved. The patient continued to be treated with 800/160mg co-trimoxazole every 12hours for 1 year.
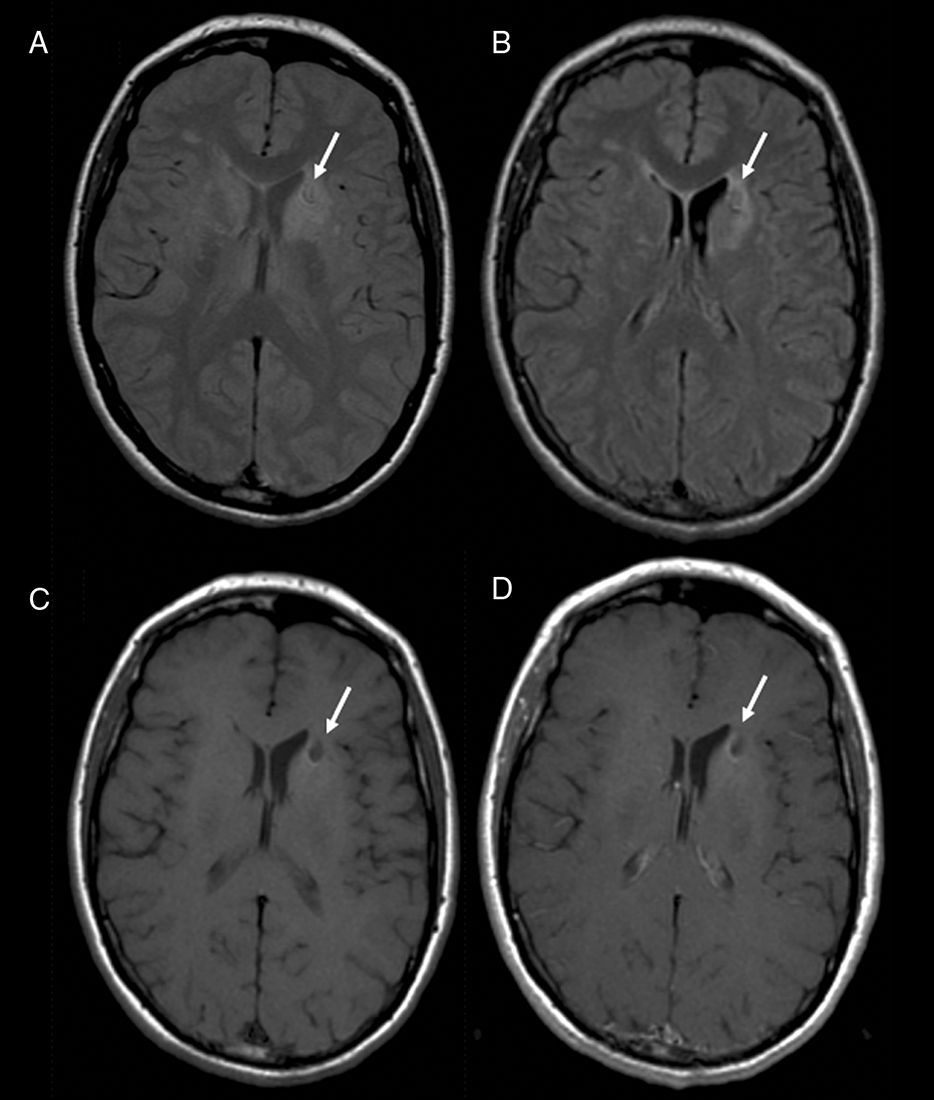
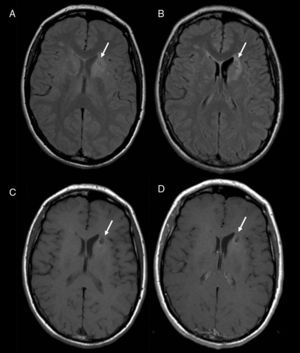
A routine MRI scan 2 months later clearly showed a reduction in the size of the lesions described by previous images. No expansile effect or contrast uptake was detected in the lesions. The patient remained asymptomatic, without abulia, and with normal plantar reflexes and sphincter control; claudication in lower limbs also improved (Fig. 2).
Routine MRI study completed at the 1-month mark shows the change in residual signal that causes retraction of the anterior horn of the lateral ventricle in DP-weighted (A), FLAIR (B) and T1-weighted sequences without contrast (C). No areas showing pathological enhancement were seen after administering contrast (D). All sequences show a nodular hypointense/isointense feature corresponding to the biopsy lesion (arrow).
Since WD is rare, it is frequently diagnosed late, especially in cases presenting with neurological signs and none of the digestive symptoms characteristic of that condition. Conventional laboratory studies reveal non-specific changes. PCR is regarded as the diagnostic technique of choice because it has higher sensitivity and specificity than other techniques. Nevertheless, negative PCR findings do not rule out the diagnosis of WD, as seen in this case.
Although findings from CT and MRI scans are non-specific, these techniques provide the most information. Cranial CT shows cerebral atrophy and single or multiple focal hypodense lesions that predominantly affect the white matter, cortex, and hypothalamus. Lesions present contrast enhancement.2 The most common MRI finding is that the lesions described above are hyperintense in T2-weighted and hypointense in T1-weighted sequences.3 Additionally, expansile lesions showing enhancement after administration of paramagnetic contrast may appear. Perfusion/diffusion-weighted MRI and spectroscopy may be useful, but few studies have been performed to date and typical patterns have not yet been described.2 Reports indicate that these techniques are valuable in cases of recurrent cerebral WD in which lesions may be smaller, even though restricted diffusion may be indicative of areas of active infection.3 Acute ischaemic lesions may produce similar imaging findings, but it is possible to distinguish between them based on their continuity and presence of absence of a fully evolved infarct.
PET studies with 11C-methionine may be used in differential diagnosis to rule out tumours; in WD, hypermetabolic regions may be present in cortical and subcortical areas including the brainstem.4 However, other studies employing 99mTc-HMPAO SPECT have described decreased cerebral blood flow in affected areas.
Please cite this article as: Lombardo Galera S, et al. Enfermedad de Whipple: presentación de un caso infrecuente de afectación cerebral aislada. Neurología. 2013;28:317–9.