Introduction: Premature cardiovascular events have been observed in systemic lupus erythematosus (SLE) patients, but the reason for this accelerated process is still debatable; although traditional risk factors are more prevalent in such patients than in the general population, they do not seem to fully explain that enhanced risk. One of the most important conditions is a proatherogenic lipid profile. There is not enough data about it in Mexican SLE patients.
Objective: To establish the differences in the lipid profiles between Mexican patients with SLE and the general population.
Material and methods: Observational, transversal, descriptive and comparative study, between SLE patients and age-sex-matched healthy volunteers. We performed a full lipid profile (by spectrophotometry) 14 hours of fast. The results obtained were analyzed by the statistical program SPSS® Statistics version 17.
Results: We studied the full lipid profiles of 138 subjects, 69 with a diagnosis of SLE and 69 agesex-matched healthy volunteers; 95.7% were females and 4.3% males. Average age was 30 years; average body mass index (BMI) 25.96 ± 5.96 kg/m2 in SLE patients and 26.72 ± 4.36 kg/m2 in the control group (p = 0.396). Average of total cholesterol 156 mg/dl in the SLE patients and 169.4 mg/dl in the control group (p = 0.028); average of low density lipoprotein (LDL) cholesterol 85.27 mg/dl in the SLE patients and 97.57 mg/dl in the control group (p = 0.023).
Conclusions: We did not find statistical differences in the lipid profiles among patients and healthy volunteers, which could explain increased cardiovascular morbidity and mortality observed in SLE patients.
Introduction
Premature cardiovascular events have been observed in systemic lupus erythematosus (SLE) patients, but the reason for this accelerated process is still debatable.1
In addition to traditional cardiovascular risk factors in SLE patients, there are factors inherent to the disease such as: immune complex-induced endothelial damage, vasculitis, thrombosis associated with antiphospholipid antibodies, Libman Sacks´ endocarditis, renovascular hypertension, glomerulonephritis and corticosteroid therapy used as part of the disease treatment.1
A greater prevalence of dyslipidemia has been reported in these patients, finding a marked pro-atherogenic lipid profile, i.e., elevation low density lipoprotein (LDL), lipoprotein (a), triglycerides and free fatty acids, as well as reduction of high density lipoproteins (HDL).2 Amongst traditional cardiovascular risk factors, dyslipidemia is considered to represent a greater impact on the development of cardiovascular disease, in addition to being related to a higher renal morbidity and a higher mortality in SLE patients.3
Chronic use of glucocorticoids, as part of the treatment of this pathology, also favours the development of a pro-atherogenic lipid profile in this population. Additionally, frequently used immunosuppressants for SLE treatment positively correlate with the antioxidant and antiinflammatory ability, reporting an oxidized LDL reduction (LDLox) in patients who receive them.4
About 75% of SLE patients develop hypercholesterolemia 3 years after diagnosis; these patients report the highest rates of cardiovascular events.5 In patients with more than 5-year of diagnosis progression, the risk of acute myocardial infarction has been reported to increase up to 52 times.6
For the above mentioned reasons, we decided to analyze and establish the differences in the lipid profiles between Mexican patients with SLE and the general population, matched by age and gender.
Material and methods
We performed an observational, transversal, descriptive and comparative study. We included 69 patients diagnosed with SLE by a rheumatologist, meeting at least 4 classification criteria of the American College of rheumatology, modified in 1997.7 The patients were 18 years of age or older, had no known cardiovascular history (myocardial infarction, angina, stroke, transient ischemic attack), attended by a rheumatologist in "Dr. José Eleuterio González" University Hospital and agreed to participate through a signed informed consent. This study was approved by our local Ethics Committee (MI09-007).
Subsequently, the patients were matched with 69 healthy volunteers by age and gender; subjects without any autoimmune diseases and no known cardiovascular pathologies at the randomization. All subjects (138) were required to comply with a 14-hour fast, following which a venipuncture was performed to obtain a full lipid profile, using the spectrophotometry technique. In addition, the following tests were done: erythrocyte sedimentation rate using the Wintrobe method, ultra-sensitive C-reactive protein (CRP), Complete Blood Count in the same lab.
We compared the total cholesterol value, LDL, HDL and triglycerides; then, we identified pro-atherogenic characteristics in the lipid profile, establishing as a cut-off point in accordance with that described in the literature as a cardiovascular risk factor: total cholesterol > 200 mg/dl, triglycerides > 150 mg/dl, HDL < 45 mg/dl, LDL > 100 mg/dl. We obtained the BMI of all patients.
Results were analyzed using the statistical program SPSS v17, performing a descriptive analysis for demographic and clinical variables.
For the binominal variable contrast, we used chi-square test or Fisher's exact test, with 2 x 2 contingency tables; for non-parametric variables we used the Mann-Whitney U test. p ≤ 0.05 was taken as a significant value.
Results
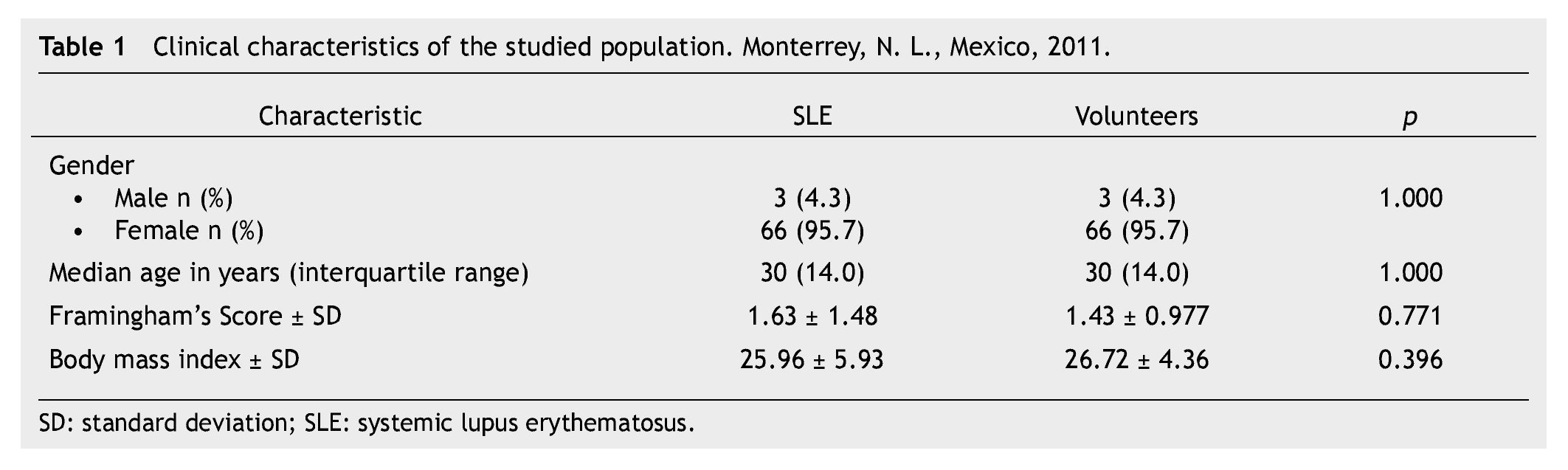
We analyzed 69 SLE patients and 69 healthy patients, 66 women (95.7%) and 3 men (4.7%) in each group matched by sex and age, with a median age of 30 years, and an interquartile range of 14 (Table 1).
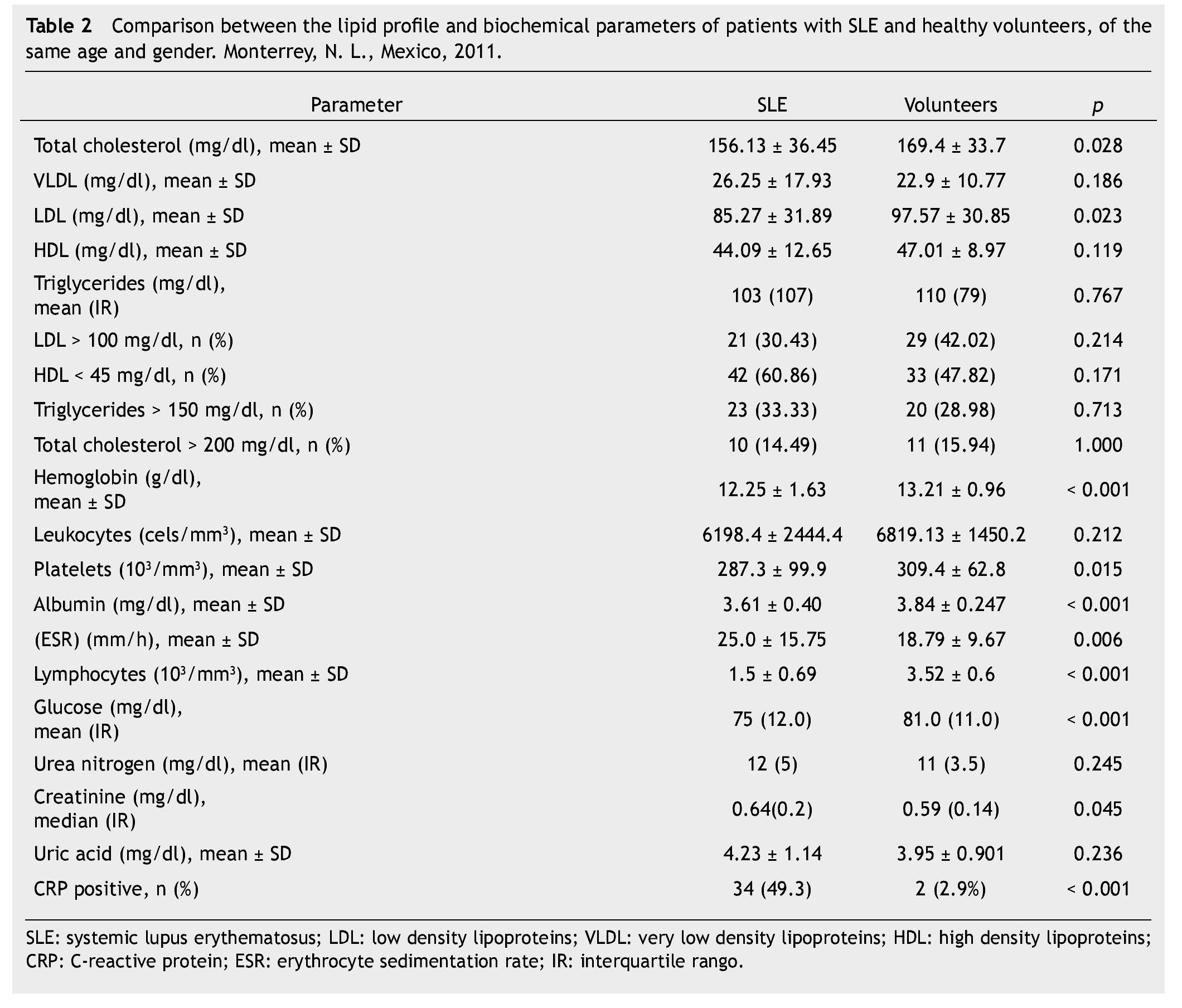
In the lipid profile, we found a total cholesterol average of 156 mg/dl in the group of SLE patients compared to 169.4 mg/dl in the control group (p = 0.028). The higher mean is in the group of healthy individuals, with a statistically significant difference. As far as LDL cholesterol levels, we found an average of 85.27 mg/dl in the group of SLE patients while in the group of healthy subjects the mean was 97.57 mg/dl (p = 0.023), also with a statistically significant difference. Despite finding statistically significant differences for absolute figures of total cholesterol and LDL cholesterol; when we performed the analysis for pro-atherogenic characteristics we did not find any statistically significant differences between both groups (Table 2).
In addition, we analyzed other clinical and biochemical parameters (BMI, erythrocyte sedimentation rate, albumin, CRP, uric acid, glucose and hemoglobin), finding that data in the group of patients regarding the erythrocyte sedimentation rate, CRP and serum creatinine were higher with statistical significance. On the other hand, the healthy volunteers group had higher hemoglobin, lymphocytes, platelets, albumin and glucose, also with statistical significance (Table 2).
In the 69 SLE patients, we also analyzed the disease's characteristics; finding that the average number of years of SLE diagnosis at the time of entering the study was 5 years; with an interquartile range of 8, this population had an average diagnostic age of 25.8 ± 7.41 years. The disease activity index used was the MEX-SLEDAI, finding an average of 1.69 ± 2.71, which places the average of the population in the low activity group.
Concerning medication use, we found that 68 patients (97.1%) used antimalarials at the time of the study; 20 patients (29.4%) were taking chloroquine at an average dosage of 150 mg/day, while 48 patients (70.5%) were taking hydro-xychloroquine at an average dosage of 200 mg/day. Sixty patients (88.2%) had been taking antimalarials routinely for over a year.
Discussion
We found the difference in total cholesterol and LDL averages to be statistically significant; however, it was significantly greater in the healthy group, which may be explained by the genetics that our Mexican population carries for dyslipidemia. Thus, we compared BMI between both groups and lipid profiles, finding no statistically significant differences.
When we analyzed atherogenic lipid levels, thus identifying cardiovascular risk, we found no differences between the lipid profiles from the SLE patients and the healthy volunteers. This suggests that there may be qualitative differences rather than quantitative ones in lipids of SLE patients.
In SLE patients, an increase in hydroperoxidized lipids associated with endothelial dysfunction has been reported, as well as a decrease in antioxidizing ability.8 High oxidized HDL levels (HDLox), not only eliminate the protecting effect of HDL, but also are associated with pro-inflammatory action and accelerated atherogenesis.2 IgG-type antibodies against LDLox are also linked with the early development of atherosclerosis observed in SLE patients.8
One of the weaknesses in our work is the fact that we did not measure LDLox levels. Increased cardiovascular risk, which in recent years has been found in SLE patients, in this studied population is not consistent with a pro-atherogenic lipid profile; however, further studies including larger number of patients are required to determine the causes that lead to an increase in cardiovascular morbimortality in this specific population.
In our Mexican population with SLE, we were not able to find a marked atherogenic profile, contrary with the recent published.3 However, in this last publication they studied Caucasian, Black and Asian races but did not include the Latin American population. Additionally, in this group characteristics associated with total cholesterol increase were age over 30 years and use of prednisone, with dosages greater than 10 mg/day. In the population studied by Petri et al., 35% of the patients used hydroxichloroquine on a regular basis, unlike our population in which 97.1% were taking anti-malarials. This is relevant because the use of hydro-xychloroquine has been linked to an improvement in lipid profiles of SLE patients.9
In a study performed in India including 30 SLE patients paired by sex and age with 30 control subjects, dyslipidemia was found in 63% of SLE patients; however, a statistically significant difference was only found in triglycerides, which turned out to be greater in the SLE group.10 In the same study, 63% of SLE patients had been diagnosed with lupus nephropathy, which could have altered lipid characteristics in that population in contrast with our population, in which they found only 12% of lupus nephropathy (none with proteinuria in nephrotic range nor undergoing renal replacement therapy, when subjects were included in the study).
In a trial including Mexican subjects, in which 16 SLE patients were studied, no difference was found in the lipid profile of SLE patients, compared to a healthy control group, paired by age, sex and BMI. However, one advantage of our study was that did include a larger number of patients and controls.11
The few studies performed in a Mexican population regarding the lipid profile in SLE patients, make it indispensable to conduct further studies on the issue. The differences found about hemoglobin, erythrocite sedimentation rate, albumin, CRP, albumin, creatinine, platelets and lymphocytes, may be explained as expected changes in SLE patients.
Another important consideration is that the SLE patient sample had a low MEX-SLEDAI (under 2, on average), which places them in the subgroup of low-activity patients, the disease activity being another variable frequently associated with accelerated atherosclerosis; however, in our population did not keep a relationship with the disease activity.12
As for other traditional cardiovascular risk factors (obesity, hypertension, hyperglycemia after fasting),12 no link with lipid profile alterations was found. However, this could be related to our patients' age at the time of inclusion in the study (mean 30 years); at this age, cardiovascular comorbidities are less prevalent.
Conclusions
We did not find statistical differences in the lipid profiles among patients and healthy volunteers to explain the increased cardiovascular morbimortality observed in SLE patients.
Conflicts of interest
The authors have no conflicts of interest to declare.
Funding
No financial support was provided.
Received: October 2013;
Accepted: January 2014
* Corresponding author:
"Dr. José Eleuterio González" University Hospital, Universidad Autónoma de Nuevo León.
Gonzalitos 235 North Avenue, Mitras Centro, Z.P.
64020, Monterrey, N. L., Mexico.
Telephone: (+52) (81) 8348 2015. Fax: (+52) (81) 8348 2065.
E-mail address: iriscolunga@hotmail.com (I. J. Colunga-Pedraza).