To establish the prevalence of sensorineural hearing loss (SNHL), as well as the predisposing risk factors, in children and adolescents with type 1 diabetes mellitus (T1DM) attending the Service of Endocrino-Pediatrics and Otolaryngology Department of the “Dr. José Eleuterio González” University Hospital and the Materno-Infantil Hospital, from January 2011 to December 2012.
Material and methodsA total of 84 children with T1DM, with ages between 6 and 18 years old, were studied. Values of glycated hemoglobin (HbA1c) were assessed and Tonal audiometry and Speech audiometry tests were performed.
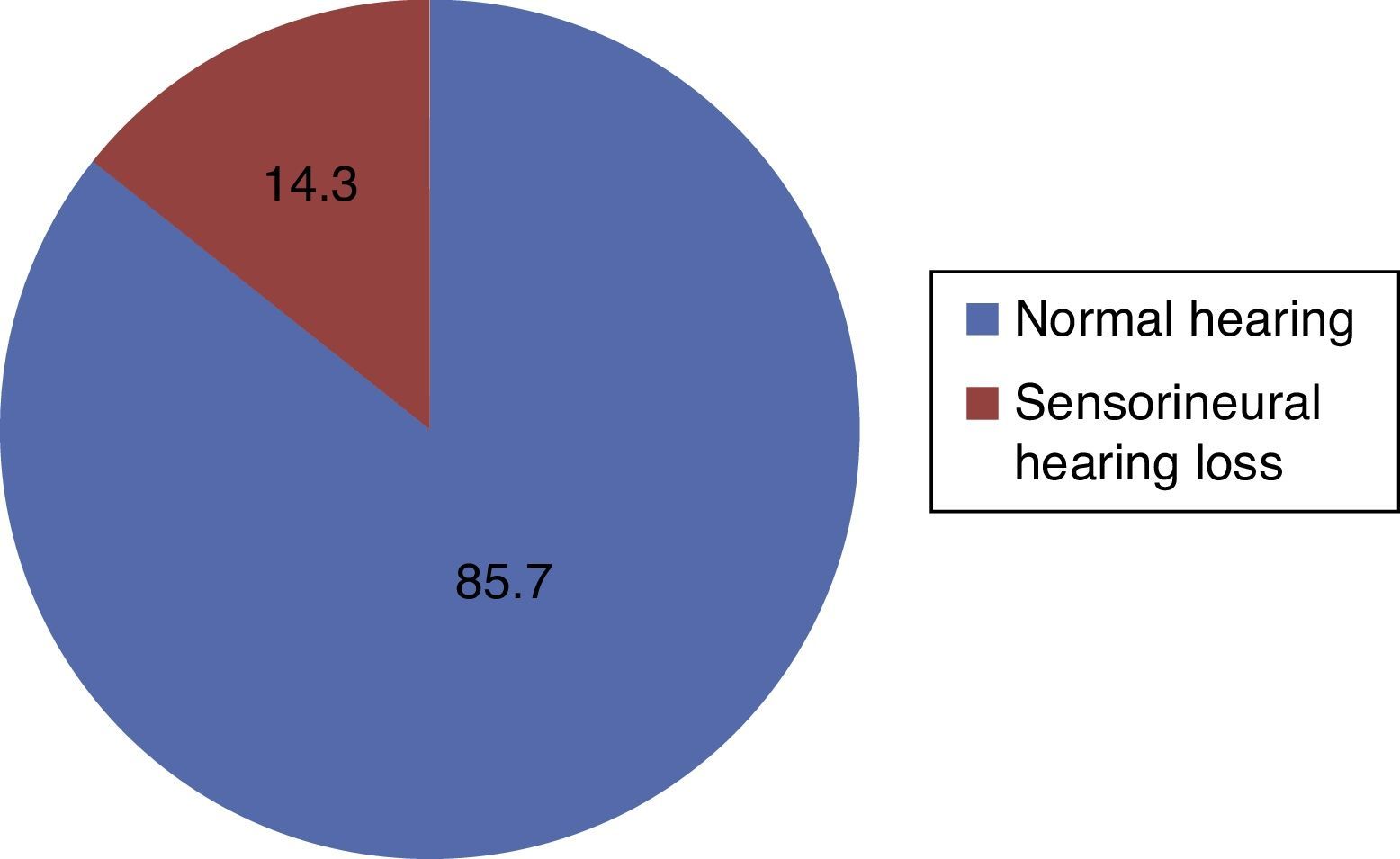
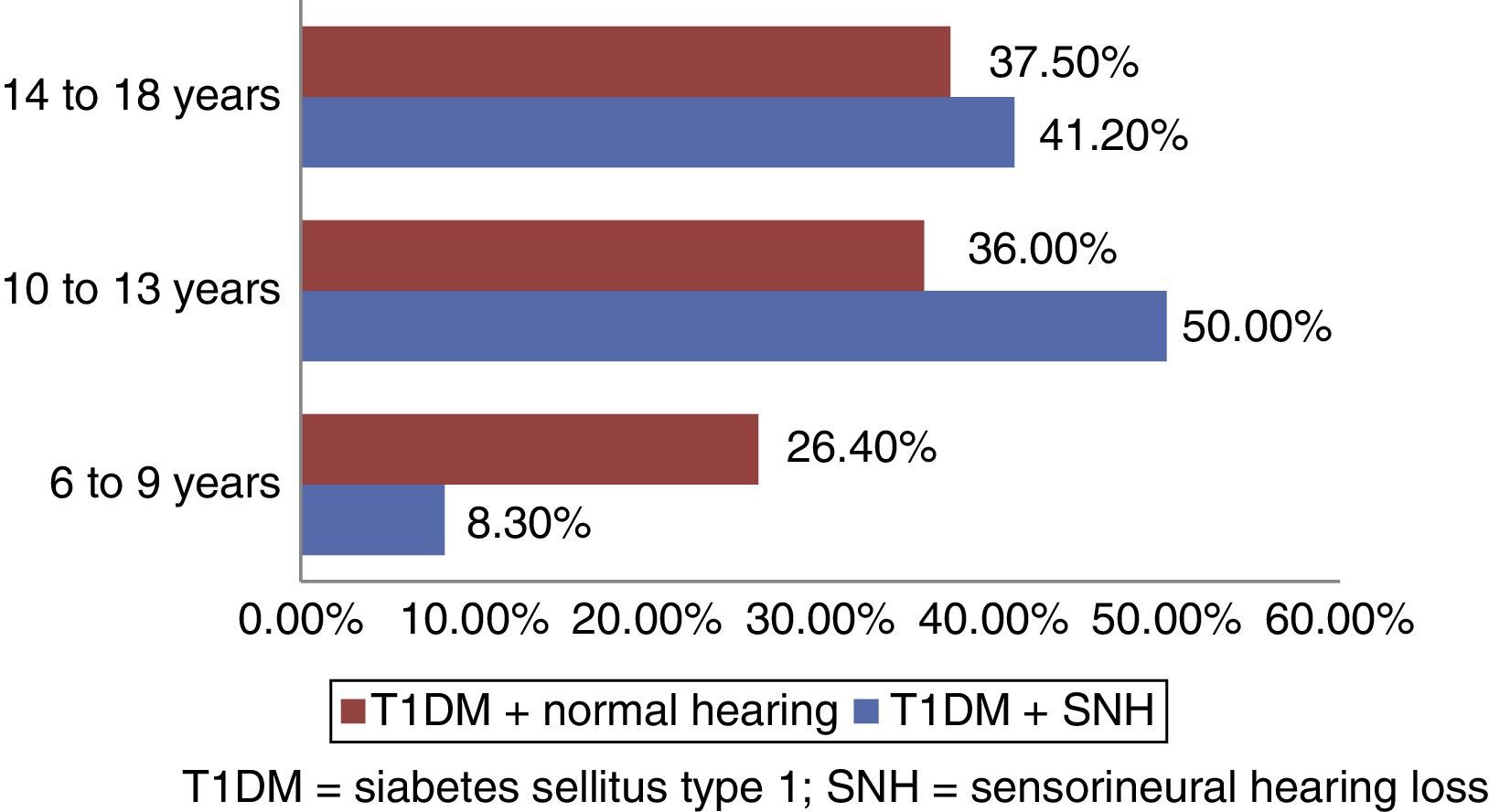
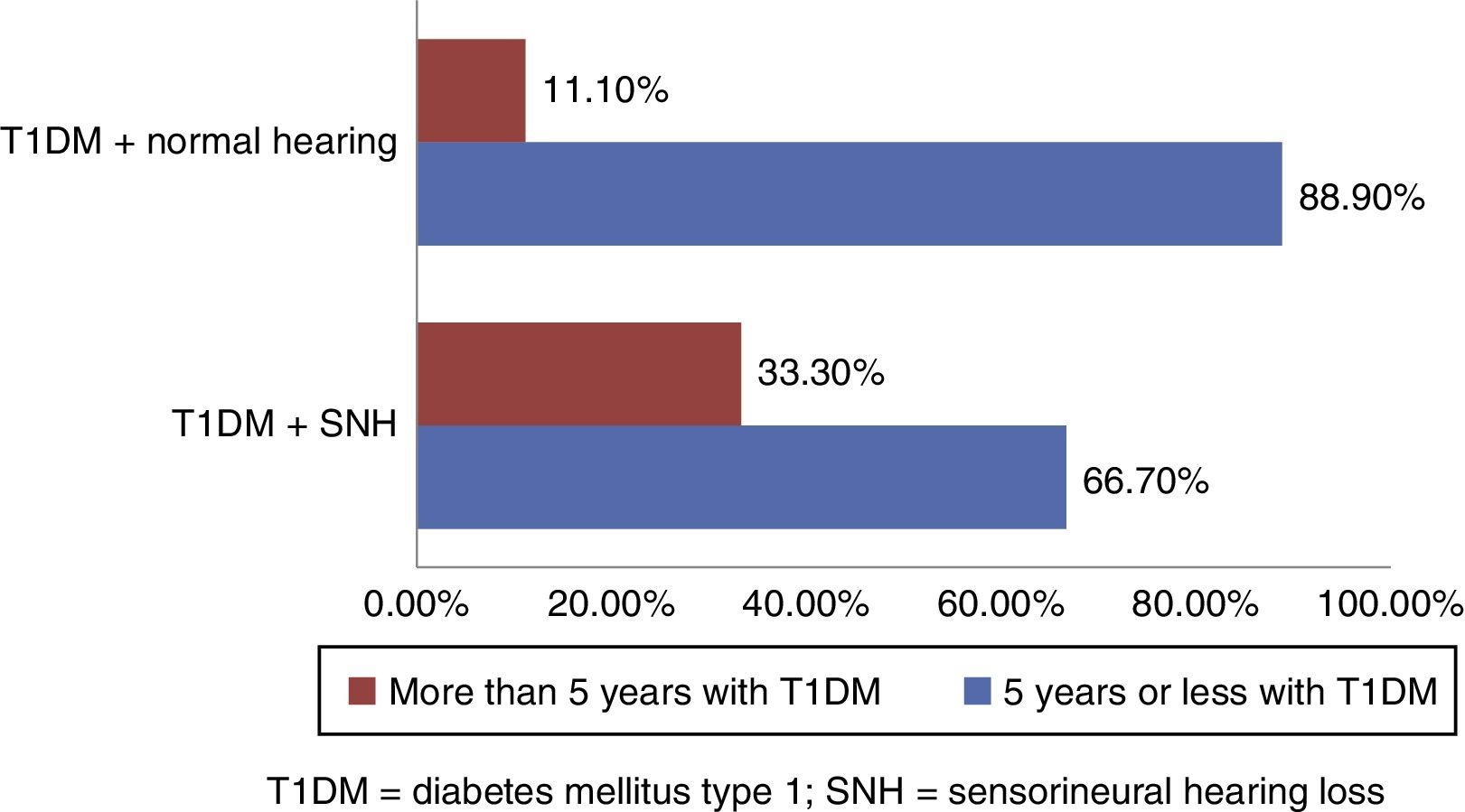
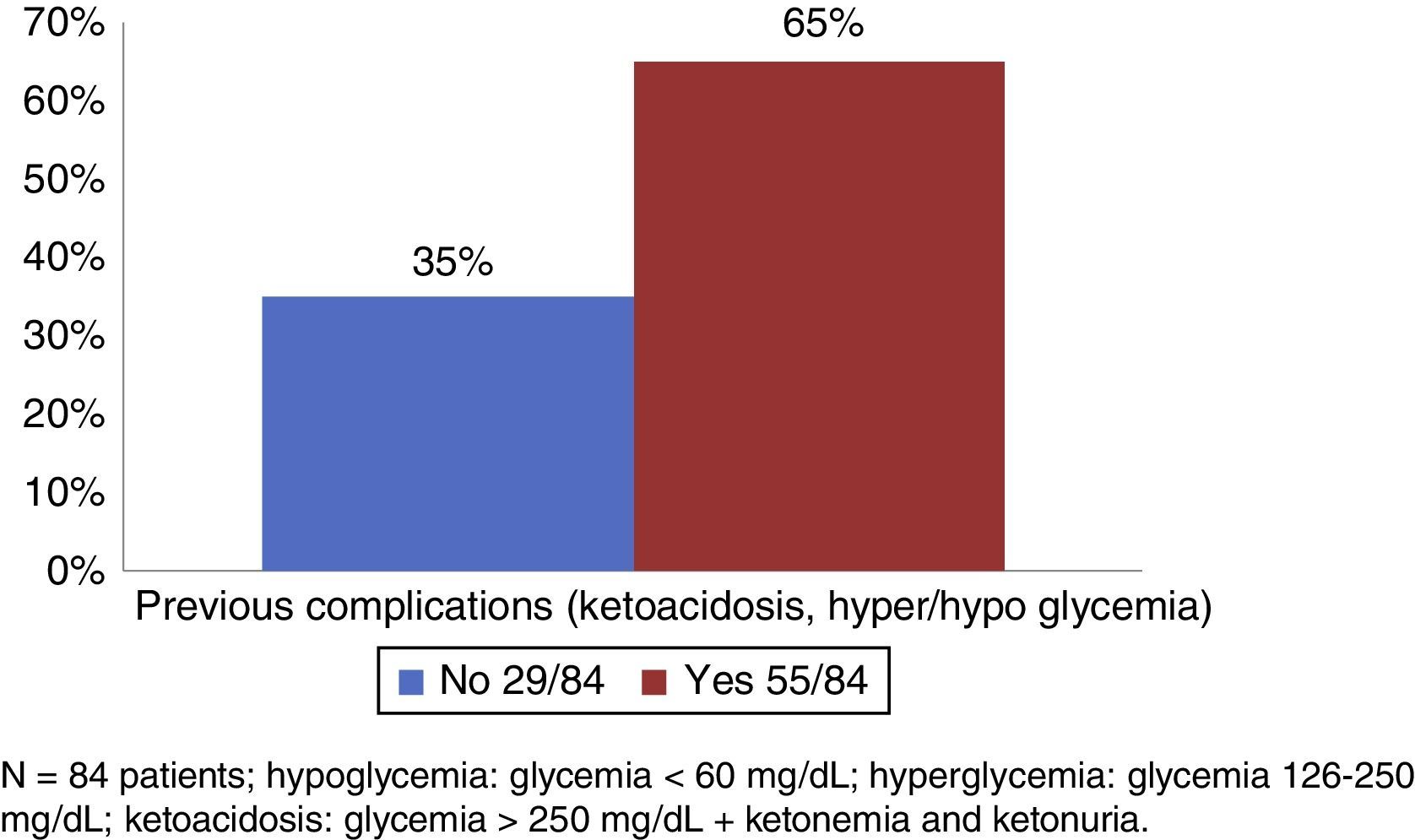
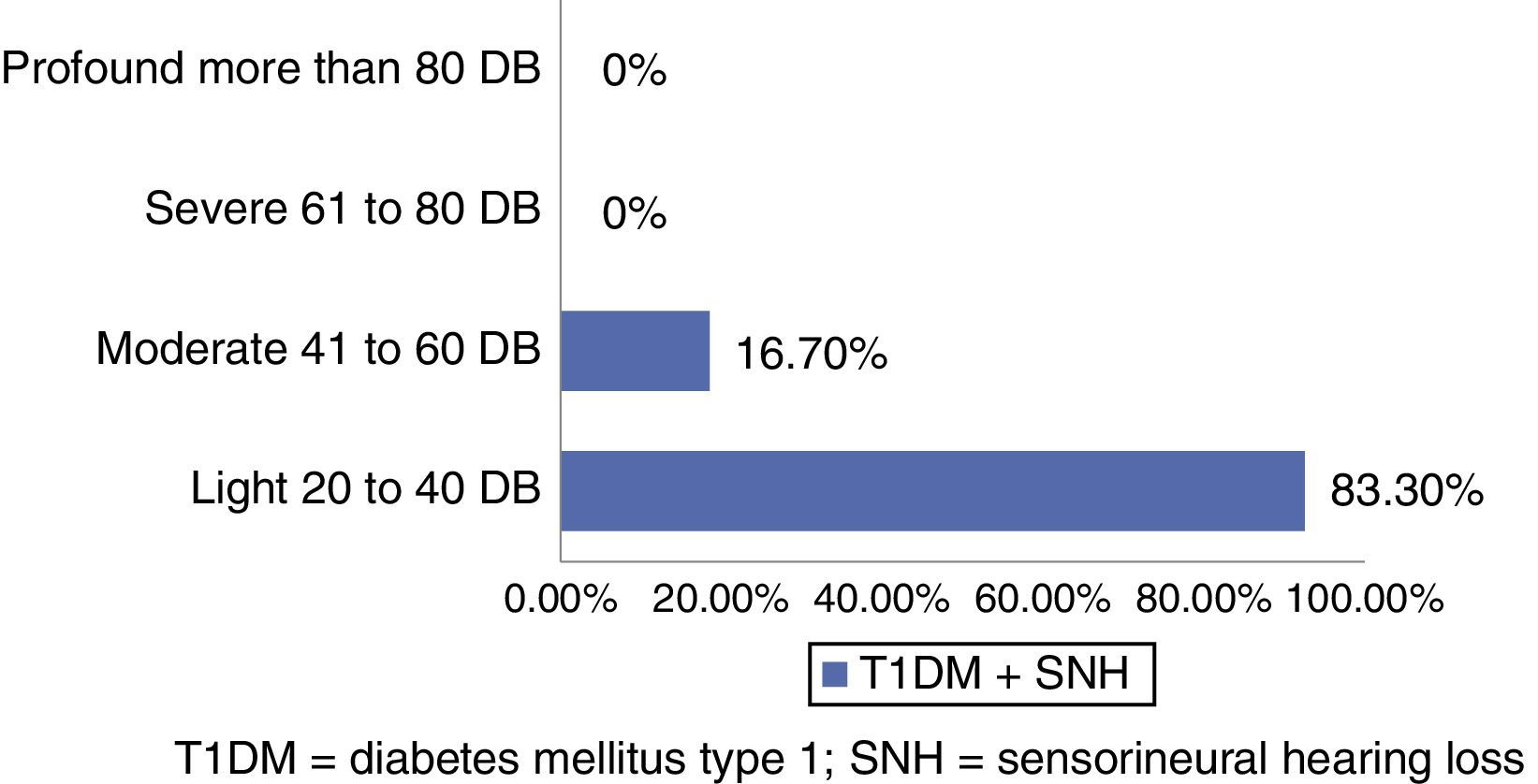
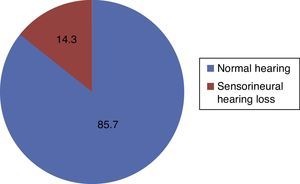
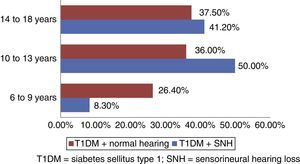
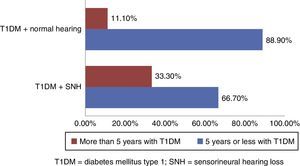
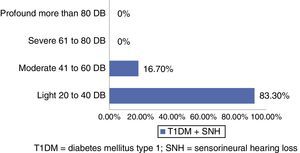
ResultsA total of 84 patients with a diagnosis of T1DM were studied, out of which 12 (14.3%) presented SNHL. Fifty percent of patients with hearing loss were in the age range of 10–13 years old. Regarding time of evolution with the disease (T1DM), 33% of patients with more than 5 years with T1DM presented SNHL, and nearly 88.9% of the patients with less than 5 years with T1DM presented normal hearing (p=0.011). Moreover, 65.47% of the patients presented complications due to poor glycemic control at some point in the evolution of their disease. All (100%) diabetic patients with SNHL and 91% of the patients without SNHL had HbA1c values greater than 6%. In patients with hearing impairments, 83.3% suffered mild and 16.4% suffered moderate hearing loss. Most presented bilateral hearing loss, with the right ear dominating. Acute frequencies, mainly 8000kHz, were the most affected.
ConclusionSNHL prevalence among our diabetic population was 14.3%, which indicates that a sixth of our diabetic type 1 population will develop SNHL. According to the results obtained, SNHL is more frequent among patients who have had T1DM for more than 5 years. Nevertheless, more studies are required to confirm that there is a relation between time spent with the disease and SNHL.
The World Health Organization (WHO) defines diabetes mellitus (DM) as a multiple-etiology metabolic disorder, characterized by chronic hyperglycemia and other metabolic abnormalities, which result in absolute or relative insulin deficiency. It is the most frequent endocrine-metabolic disorder in children and adolescents, and has remained the main type of diabetes in children.1–4
Type 1 diabetes mellitus (T1DM) is a disease with an etiology of intervening environmental factors which interact with a genetic-predisposition component; it is considered a chronic autoimmune disease which causes the destruction of the pancreatic β cells which produce insulin.5
The average age of the onset of the disease is between 7 and 15 years of age; however, it may occur at any age.6 Values of the HbA1c>6% higher than the normal range (5–6%) have been considered a risk of developing micro- and macroangiopatic complications. The affection of the blood vessels which supply the inner ear and the vascular stria have been reported by different authors as a physiopathological cause of SNHL in T1DM patients.3,7 Treatment with insulin, maintaining on average HbA1c of 7.2%, reduces the onset and progression of microangiopatic complications, atrophy, and demyelination of the spiral ganglion by up to 76%.8,9,13
Sensorineural hearing loss (SNHL) is a loss of hearing at any frequency more than 25dB, with conductive and sensorineural gaps lower that 20dB, and affecting the patient's ability to communicate, his or her education, job prospects and social relationships, and also causes stigmatization.11,12
The reported prevalence of SNHL is up to 33% in children with T1DM versus 0.3–0.5% in healthy children. In Mexico there is a lack of sufficient epidemiologic information which defines the hearing condition prevailing in our population.12
Materials and methodsA prospective longitudinal, analytic, comparative study was conducted on a total of 87 patients of both sexes, ages 6–18, with a T1DM diagnosis, from the Service of Endocrino-Pediatrics and Otolaryngology Department of the “Dr. José Eleuterio González” University Hospital and the Materno-Infantil Hospital, from January 2011 to December 2012.
We included patients who agreed to participate in the protocol through a signed informed consent, signed by their parents and/or guardians and/or the patient. We excluded patients with noise exposure, a family history of deafness, use of ototoxic medications, otitis media, a history of previous ear surgery (except ventilation tube insertion) and DM type 2.
All subjects in this study were given a questionnaire, which included family, prenatal, natal and personal pathological and non-pathological history. Patients underwent basic otorhinolaryngological exploration, tone audiometry and oral audiometry using an audiometer AUDIOTEST 259b, manufactured for Interacustics, Type 2 Tone Audiometer, Type B-E-T speech audiometer in a soundproof cabin Acoustics Systems, Model RE-142, Serial #21413ª, made in USA. The study was approved by the Ethics and Research Committee of the School of Medicine of the Universidad Autónoma de Nuevo León (UANL by its Spanish acronym) with the registration key OT12-002.
The information obtained was gathered in a database using Excel, performing statistical analysis using SPSS 20.0. We obtained the traditional statistics in the quantitative and qualitative variables, looking to establish differences between both groups through hypothesis tests for means and proportions, to establish the absence or presence of association and correlation using chi square, Pearson or Spearman, with a confidence and reliability of 95%.
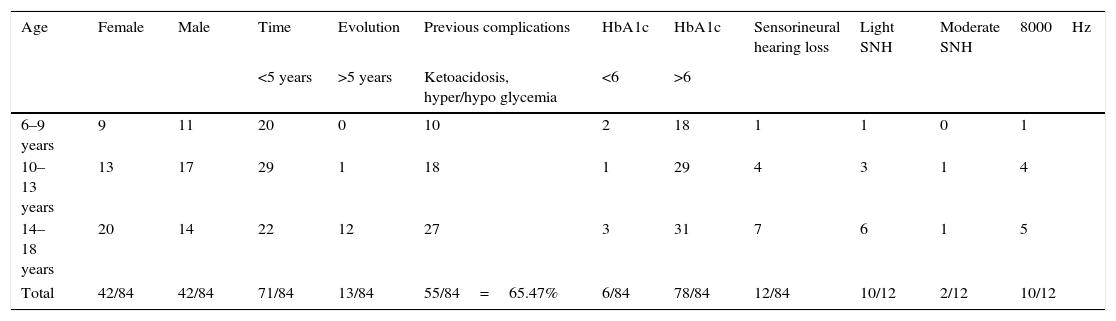
ResultsOut of the 87 recruited patients with a T1DM diagnosis, we excluded a patient with a history of chronic otitis media of the right ear, one with otitis media with bilateral effusion and a patient with a final diagnosis of T2DM. The remaining 84 patients were divided into 3 groups based on age: 6–9, 10–13, and 14–18 years old. We observed that 72 patients with a T1DM diagnosis showed normal hearing while 12 T1DM patients showed sensorineural hearing loss (Fig. 1).
The 6–9 group included 20 patients (9 girls and 11 boys) with diabetes with an evolution time of less than 5 years; 10 (50%) subjects presented a history of previous complications like ketoacidosis, hyperglycemia or hypoglycemia, 2 (10%) patients had HbA1c<6 and 18 HbA1c>6, and 1 (5%) subject presented mild SNHL for 8000kHz thresholds. The 10–13 group included a total of 30 patients (13 girls and 17 boys); 29 (34.5%) had had diabetes mellitus for less than 5 years and 1 (1.21%) for over 5 years, 18 (21.4%) patients presented a history of ketoacidosis, hypo- or hyperglycemia, 29 (34.52%) presented HbA1c>6 and 1 (1.19%) HbA1c<6; mild SNHL was displayed in 3 (3.57%) subjects and 1 (1.19%) patient displayed moderate SNHL, and all 4 patients were in hearing thresholds of 8000kHz. The 14–18 group consisted of 34 patients (40.47%) (20 girls and 14 boys), 22 (64.70%) with an evolution time of less than 5 years and 12 (35.29%) for more than 5 years; complications like ketoacidosis, hypo- or hyperglycemia were reported by 27 of them; 3 (8.82%) subjects showed an HbA1c<6 and 31 (91.17%) an HbA1c>6; SNHL occurred within this group in 7 individuals (mild in 6 and moderate in 1). In all patients, SNHL was observed in thresholds of 8000kHz (See Table 1).
Result of variables studied, by age group.
| Age | Female | Male | Time | Evolution | Previous complications | HbA1c | HbA1c | Sensorineural hearing loss | Light SNH | Moderate SNH | 8000Hz |
|---|---|---|---|---|---|---|---|---|---|---|---|
| <5 years | >5 years | Ketoacidosis, hyper/hypo glycemia | <6 | >6 | |||||||
| 6–9 years | 9 | 11 | 20 | 0 | 10 | 2 | 18 | 1 | 1 | 0 | 1 |
| 10–13 years | 13 | 17 | 29 | 1 | 18 | 1 | 29 | 4 | 3 | 1 | 4 |
| 14–18 years | 20 | 14 | 22 | 12 | 27 | 3 | 31 | 7 | 6 | 1 | 5 |
| Total | 42/84 | 42/84 | 71/84 | 13/84 | 55/84=65.47% | 6/84 | 78/84 | 12/84 | 10/12 | 2/12 | 10/12 |
In our study, we were able to observe a percentage prevalence of SNHL of 14.3% (12 out of 84 patients). Also, 64 patients (76.19%) with T1DM were older than 10 years of age, as opposed to a small group of 20 patients (23.80%) between the ages of 6 and 9 (Fig. 2). There were no differences in gender, each representing 50%. In regard to time of evolution of T1DM, 15.47% (13 patients) with over 5 years with T1DM presented SNHL, and 84.52% (71 patients) with less than 5 years with T1DM presented normal hearing, this being a statistically significant value (p=0.011) (Fig. 3).
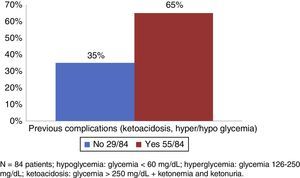
Out of the 84 patients, 55 (64.47%) presented complications at some point during the evolution of their disease due to glycemic irregularities; the most frequent complication was ketoacidosis and the least prevalent was hypoglycemia (Fig. 4).
In the present study, 100% of diabetic patients with SNHL (12 patients) and 91% of patients with normal hearing presented HbA1c values greater than 6%, showing an average value of 7.5% in the general population studied. According to age groups, the group consisting of children between 6 and 12 years presented, on average, an HbA1c value of 7.24%, while the group consisting of children between 13 and 19 years of age presented, on average, an HbA1c value of 7.67%.
Of all the SNHL patients, 83.30% (10 patients) presented mild hearing loss and 16.70% (2 patients) moderate hearing loss (Fig. 5). Most patients presented bilateral hearing loss, predominately on the right ear. The 8000kHz thresholds were the most affected. (Table 1)
DiscussionAn SNHL prevalence of up to 33% in children with T1DM has been considered, versus 0.3–0.5% in healthy children. In Mexico, there is a lack of epidemiologic information that can define the hearing condition which prevails among our population.12
The observed prevalence in our studied group was 14.3%, contrary to the rate reported in different publications. However, we must keep in mind that most of the studied population is American or European. It is important to stress the fact that there are still many T1DM cases that have not been diagnosed, but with the obtained results at this point, we are able to infer that up to a sixth of the diabetic population in our society will develop SNHL.
Regarding age, the obtained information matches the one found in the bibliography. Most children are in the mentioned peak ranges, especially above 10 years of age, beginning with hormone changes that are a normal part of puberty and adolescence. Nevertheless, based on the obtained results we are able to see that the patient's age does not represent a risk factor for the presence of SNHL.
According to the American Diabetes Association (ADA) and the Diabetes medical attention standards of 2014, the goal for HbA1c in type 1 diabetic patients varies depending on age. Concerning values <8% in the 6–12 years-of-age range, because it is not possible to have more strict goals due to the risk of developing hypoglycemia, even in this age range we can demand goals of <7.5% in specific cases where patients do not present severe hypoglycemia. In the 13–19 years-of-age range, values of <7.5% are considered and in specific cases even <7%. In children under 6 years of age, goals of <8% are too strict, so up to <8.5% is acceptable, because these children have a greater vulnerability for hypoglycemia, a greater sensitivity to insulin, and are unpredictable in their intake and physical activity.10
The average population showed HbA1c values of 7.5% and taking the results by age group into account, we are able to say that our patients, under 13 years of age with an HbA1c average of 7.24%, are within an adequate glycemic control, because they are inside the accepted range by the ADA 2014 (6–12 years=<8%); and patients older than 13 years of age with an average of 7.67% show a control barely above that expected for their age group (13–19 years=<7.5%).
It is important to maintain HbA1c values as close to normal as possible, thus reducing by almost 80% the risk of presenting microangiopatic complications; however, we must not be very strict with our population, especially with children under 13 years of age, because of the risks of presenting severe or belated hypoglycemia cases, and hence the importance of following the standards established by the ADA 2014.
Regarding time of evolution with T1DM, it was the only statistically significant risk factor (p=0.011) for a period greater than 5 years and the presence of hearing loss. However, when we looked for the correlation between both factors, we did not find it. The present study showed a greater prevalence of hearing loss in patients with more than 5 years of evolution of T1DM, without it being associated or related. This could be due to the lack of potency in the studied population who presented T1DM and SNHL, requiring a greater number of patients and further research. Nevertheless, it is important that 5 years after a T1DM diagnosis, as there is an already established protocol in search of microangiopatic complications like retinopathy, we establish the application of hearing studies which allow us to detect hearing problems in a timely manner.
Out of all of our patients with SNHL, 83.3% presented a mild hearing loss, bilaterally, in acute frequencies, predominately 8000Hz, which agrees with the rate obtained in previous studies. The type of hearing loss presented in these patients is similar to the one that patients with presbycusis would present, but at an earlier age compared to the population without T1DM.
This research provided valuable data to lead the way for new researches in these types of patients, and establish a timely and protocol-led assessment for their glycemic control as well as their hearing, thus avoiding hearing complications which patients with a T1DM of long duration present, like SNHL and sudden hearing loss. Also, later studies are recommended where a long-term follow-up is given to these patients in order to determine the causation degree of the studied risk factors on the base pathology.
Conflicts of interestThe authors have no conflicts of interest to declare.
FundingNo financial support was provided.