The correlation between epilepsy and psychiatric complications is recognized by medical literature. However, there are reports that establish doubt about this. Therefore, the main intention of this project is to determine the prevalence of associated psychiatric disorders through the application of the MINI- PLUS International Structured Interview in patients with a diagnosis of epilepsy who were being treated in an outpatient setting at the Neurology Outpatient Clinic of a tertiary level care hospital in Northeastern Mexico, during the months of April and May of 2016.
Materials and methodsWe performed a descriptive, cross-sectional study in which patients with a diagnosis of epilepsy, regardless of type or etiology, older than 18 years of age, were included. We excluded those who underwent prior surgery without a known psychiatric diagnosis and without clinical evidence or with a diagnosis of mental retardation, dementia or an established language disorder.
ResultsWe were able to record general socio-demographic data, number of currently used antiepileptic drugs, and the type of epileptic seizures, according to the classification of the International League against Epilepsy of 1981.
A total of 33 patients was included, since of the 42 detected, two did not agree to participate in the study, four had a diagnosis of mental retardation and three were already under psychiatric treatment for major depressive disorder. The MINI PLUS was fully applied to all of the remaining selected patients.
ConclusionThrough the application of the MINI PLUS Interview, we found that 12 patients, 36.36% of the sample, presented a psychiatric disorder comorbid to epilepsy.
Despite the extensive literature indicating that depression is a frequent psychiatric complication of epilepsy,1,2 different reports show that this and other mood disorders continue to be little-known and under-treated amongst these patients,3–5 causing a negative impact on the quality of life in this population.6
The link between epilepsy and psychiatric comorbidity has consistently been analyzed, and diverse studies show that it ranges between 20% and 50%, reaching up to 80% in selected populations (i.e. in patients with temporal lobe epilepsy), and it is clear that these indexes are superior to those found amongst the general population, which are between 10 and 20%.7
Today, there are several clinimetric tools for the detection and assessment of mental disorders; nevertheless, the M.I.N.I. (Mini International Neuropsychiatric Interview) is a short, highly-structured interview of the main psychiatric disorders of the CIE-10 and DSM-IV, which may be administered by psychiatrists and non-psychiatric physicians after a short training period. The interview was initially developed by Y. Lecrubier, et al. of the Pitié-Salpêtrière Hospital of Paris and D. Scheehan, et al. of the University of Florida in Tampa in the years 1992, 1994 and 1998. There are several versions, and it has been translated into 33 different languages.7
The version of the administered test for this paper specifically was the M.I.N.I. PLUS (Mini International Neuropsychiatric Interview PLUS version), which includes mainly Axis I mental disorders, showing a “wide” version, since it includes 23 disorders instead of 17 in comparison to the original version. It includes modules for somatization disorder, hypochondria, body dysmorphic disorder, pain disorder, attention deficit disorder with hyperactivity, adaptive disorders, premenstrual dysphoric disorder, mixed anxiety disorder and depression, and yet is similar in practicality and reliability to the original test.8
With an administration time of approximately 45 to 60minutes, the test was designed to satisfy the need of a structured psychiatric interview, be short but accurate for multi-centered clinical trials and epidemiological studies, and be used as the first step in the monitoring of the results in everyday clinical practice. 8
ObjectiveTo determine the prevalence of associated psychiatric disorders through the application of the Mini-international structured interview PLUS in patients with a diagnosis of epilepsy who were being treated in an outpatient setting at the Neurology Outpatient Clinic of a tertiary level care hospital in Northeastern Mexico, during the months of April and May 2016.
Materials and methodsThe present study was descriptive and transversal, including patients with a diagnosis of epilepsy regardless of type or etiology, patients who were 18 years old or older, excluding those who had previously undergone surgery, patients without a known psychiatric diagnosis, and without clinical evidence or an established diagnosis of mental retardation, dementia or language disorder.
General socio-demographic data were consigned, along with the number of anti-epilepsy medications used daily and the type of seizure, according to the classification of the International League Against Epilepsy (ILAE) of 1981.9
Out of the 42 detected patients, we were able to include 33 patients, since 2 patients did not agree to participate in the study, 4 were diagnosed with mental retardation and 3 were already under psychiatric treatment due to a major depressive disorder.
The MINI PLUS interview was applied to the selected patients. Additionally, general information was obtained through the completion of a form with the following socio-demographic information: age, gender, marital status, level of education, years of evolution of the epilepsy, number of pharmaceuticals prescribed and type of seizures. Prior to the completion of the interview, the purpose and objectives of the research were explained to the patients, and all signed an informed consent.
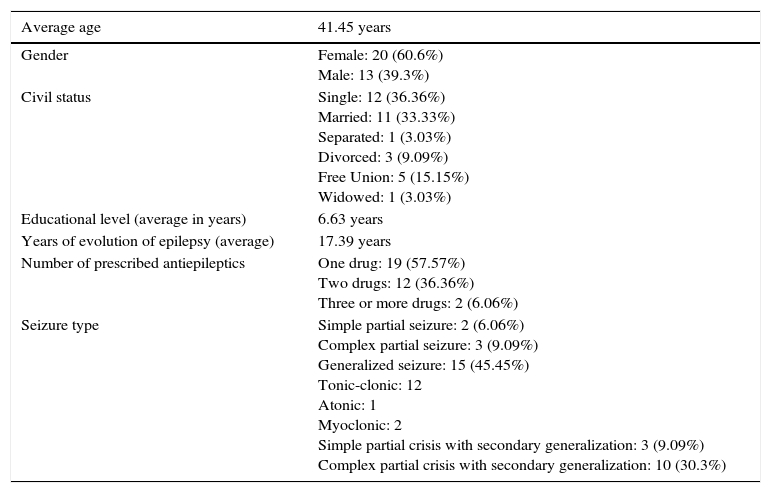
ResultsThe results of the socio-demographic variables are shown in the following table (Table 1). As observed, the average age of the studied sample was 41.45 years old. The majority of the patients were female (60.6%) and mostly single (36.36%). The patients showed a level of education of 6.63 years/patient, with an average time of evolution of epilepsy of 17.39 years. Over half of the patients (57.57%), were -at the time of the study- under treatment with monotherapy, and only 2 patients were taking 3 or more anti-epileptic medications (6.06%). The type of seizure most commonly found was generalized epilepsy (45.45% of the sample), showing that the generalized tonic-clonic type corresponded to 12 patients (36.36%), followed by the partial complex seizure with secondary generalization in 10 patients (30.3%), simple partial seizures with secondary generalization in 3 patients (9.09%), and partial complex seizures in the other 3 patients (9.09%).
Socio-demographic characteristics (N=33).
| Average age | 41.45 years |
|---|---|
| Gender | Female: 20 (60.6%) Male: 13 (39.3%) |
| Civil status | Single: 12 (36.36%) Married: 11 (33.33%) Separated: 1 (3.03%) Divorced: 3 (9.09%) Free Union: 5 (15.15%) Widowed: 1 (3.03%) |
| Educational level (average in years) | 6.63 years |
| Years of evolution of epilepsy (average) | 17.39 years |
| Number of prescribed antiepileptics | One drug: 19 (57.57%) Two drugs: 12 (36.36%) Three or more drugs: 2 (6.06%) |
| Seizure type | Simple partial seizure: 2 (6.06%) Complex partial seizure: 3 (9.09%) Generalized seizure: 15 (45.45%) Tonic-clonic: 12 Atonic: 1 Myoclonic: 2 Simple partial crisis with secondary generalization: 3 (9.09%) Complex partial crisis with secondary generalization: 10 (30.3%) |
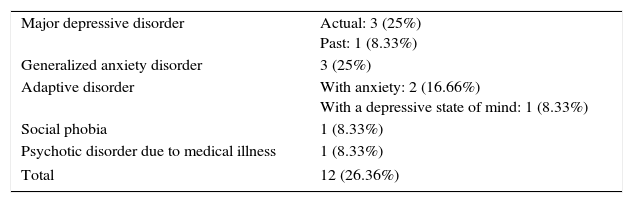
After the application of the MINI PLUS, we were able to see that 12 patients (36.36%) presented a psychiatric disorder comorbid to epilepsy.
The diagnoses discovered were: major depressive disorder in 4 patients (33.33%), generalized anxiety disorder in 3 patients (25%), anxiety disorder in 2 patients (16.66%) and depression in 1 patient (8.33%), in addition to a diagnosis of social phobia in 1 patient (8.33%) and a psychotic disorder associated with co-morbid medical illness in 1 patient (8.33%). This information is summarized in Table 2.
Comorbid psychiatric disorders (N=33).
| Major depressive disorder | Actual: 3 (25%) Past: 1 (8.33%) |
| Generalized anxiety disorder | 3 (25%) |
| Adaptive disorder | With anxiety: 2 (16.66%) With a depressive state of mind: 1 (8.33%) |
| Social phobia | 1 (8.33%) |
| Psychotic disorder due to medical illness | 1 (8.33%) |
| Total | 12 (26.36%) |
Due to the small size of the sample and the type of study performed, no definitive statements can be made about the results found. These findings serve as a basis for future research and should be seen as an approximation to the socio-demographic and clinical characteristics evidenced in patients with epilepsy in the studied population. However the data obtained does correlate with that published in the international literature.
The prevalence of psychiatric disorders varies according to the different studies, ranging from 20 to 50%,7 with a prevalence of 36.36% in the present study. Among the most frequent diagnoses are anxiety disorder, major depressive disorder10 and adaptive disorders. Regarding this last diagnosis, and as an observation, in previous studies the MINI International Neuropsychiatric Interview was applied as a diagnostic tool in its original version, which does not include the adaptive disorder as one of the screening diagnoses,10,12 this being a contribution or finding in the present study, this diagnosis represents 25% of the total psychiatric comorbidities observed.
The adaptive disorder is interesting to briefly address, in light of what has been previously referred. It usually occurs after a significant stressor, which may manifest itself through a wide range of symptoms, without integrating any other defined mental disorder.11 It results from an emotional reaction of “adjustment”, which in general merits only psychotherapeutic interventions such as short supportive psychotherapy, but which, when detected, allows a close follow-up of the patient to evaluate their remission, persistence or worsening of symptoms, which, like other mental illnesses, results in a focus on early detection and management.
ConclusionThe application of standardized interviews such as the MINI-International Neuropsychiatric Interview is accessible, economical and easy to apply. It represents an instrument of great utility in clinical settings, whose strength is aimed at the early recognition of psychiatric disorders that allows the clinician to refer to a specialized psychiatric service as an integral part of the multidisciplinary management of patients with epilepsy.
Ethical disclosuresProtection of human and animal subjectsThe authors declare that no experiments were performed on humans or animals for this study.
Confidentiality of dataThe authors declare that they have followed the protocols of their work center on the publication of patient data.
Right to privacy and informed consentThe authors have obtained the written informed consent of the patients or subjects mentioned in the article. The corresponding author is in possession of this document.
FundingNo financial support was provided.
Conflict of interestThe authors have no conflicts of interest to declare.