Operative procedures and anti-tuberculosis combinations are controversial for tuberculous spondylitis (TS) management in cases with risk of deformity, fragments, instability, and neurological disorders.
PurposeTo assess the effectiveness of a combination of anti-tuberculosis and pedicle screw sublaminary wiring (PSSW) for treating TS.
MethodThis study was a cohort study with a pre-test/post-test control design. This study was conducted at the Dr. Zainoel Abidin Hospital (Banda Aceh) from March 2005 to March 2007. Sampling technique was judgement sampling. Neurological data deficit (Frankel classification) was analyzed before and after treatment using the Spearman test. Kyphosis angles were analyzed before and after treatment using the regression correlation test.
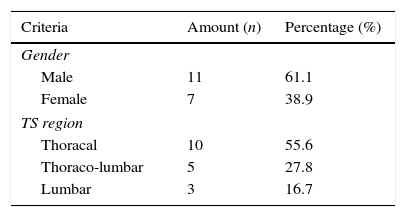
ResultsA total of 18 patients (61.1% male and 38.9% female) participated in this study. The spinal column involved in this study was 55.6% thoracic, 27.8% thoraco-lumbar, and 16.7% lumbar. Neurological status before the treatment was 11.1% Frankel C, 72.2% Frankel, D, and 16.7% Frankel E. Neurological status after the treatment was 5.55% Frankel C and 94.4% Frankel E. It showed that there was no significant association between a combination of anti-tuberculosis and PSSW for neurological deficit improvement (P=0.212). The mean angle of kyphosis before the treatment was 23.05±11.9 while after the treatment it was 10.5±5.9. It showed that there was a significant association between a combination of anti-tuberculosis and PSSW for kyphosis degree improvement (P=0.000).
ConclusionsA combination of anti-tuberculosis and PSSW for six months provided significant results if assessed from degree of kyphosis, but did not provide significant results if assessed from Frankel classification.
Tuberculosis spondylitis (TS) is one of the oldest known human diseases. This disease was first described in 1779 by Percival Pott, therefore this disease is also known as Pott's disease.1 The average number of extra-pulmonary tuberculosis (TB) in the world has remained stable. TS is most commonly musculoskeletal TB, the prevalence of which is about 40–50% of all cases of musculoskeletal TB2 and an estimated 1–2% of all cases of TB.3 TS incidence is 1.17 per 100,000 in females and 0.916 per 100,000 in males.4 Furthermore, the incidence of neurological complications of TB is about 10–43%.5
TS is the most dangerous musculoskeletal TB. It can cause damage due to bone deformity, serious morbidity, bone disorders, and severe neurological deficits.6 The regions of the spine that were most often affected by TS were 35% lumbar, 31% thoracal, 15% thoraco-lumbar, 13% cervical, and 6% cervico-thoracal,7 but this percentage was varied in several other publications. Garg and Somvanshi8 revealed that the thoracic region of the vertebral column was most frequently affected. Godlwana et al.4 found that the spinal region affected was 42% thoracic, 30% lumbar, 11% cervical, 10% thoraco-lumbar, 5% lumbosacral, and 2% sacral. Turgut3 found that the spinal region affected was 55.8% thoracic, 22.8% lumbar, 16.9% thoracolumbar, and 4.2% cervical. Kotil et al.9 found that the most common region of Pott's disease was the thoracolumbar junction (41%), followed by the thoracic (36%), and lumbar (23%) regions.
Until now, the management of TS is still controversial due to the high variation in clinical TS. The Medical Research Council of the United Kingdom (MRC, London) suggested the use of an isoniazid and rifampicin regimen for six months as standard therapy for TS, but it did not include TS with damage to three or more areas of the spine.10 Other studies revealed that the risk of deformity, instability, and progressive neurological deficits were related to the number of spinal areas damaged and indicated that operative management should maintain spinal stability.6,11 Therefore, although the MRC10 suggested that drug therapy is a standard treatment for TS, it is not applicable to all cases of TS.
One of the operative procedures for TS is pedicle screw sublaminary wiring (PSSW). PSSW, besides correcting kyphosis degrees, is also expected to improve neurological deficits.12 A study conducted by Jutte and Van Loenhout-Rooyackers13 and Issack and Boachie-Adjei14 revealed that surgical management could improve the degree of kyphosis.
In this study, we conducted the observation of kyphosis improvement after PSSW combined with anti-tuberculosis drugs, as associated with neurological status.
Material and methodResearch designThis was an observational analytical study. The design of this study is a cohort study with a pretest/posttest control design.
Research schedule and locationThe study was conducted at the Orthopaedic Department of the Centre of Surgery Installation and the Radiology Installation at the Dr. Zainoel Abidin Teaching Hospital, from March 2005 to March 2007.
Research population and sampleThe samples in this study were TS patients who agreed to receive a combination of anti-tuberculosis therapy with PSSW based on clinical indications. The sampling technique used in this study was judgement sampling. The inclusion criteria of this study were (1) patient age >18 years, (2) diagnosed clinically, microbiologically, and radiologically as TS, (3) the lesion's regions were found in the thoracal, thoraco-lumbar, and/or lumbar regions. Exclusion criteria of this study were (1) patients with other spine disorders and (2) patients with severe systemic disorders.
Research proceduresThe procedure of this study was (1) provision of explanations and recording of baseline data, including personal, demographic, and clinical information, consisting of neurological deficits according to the Frankel classification and the kyphosis angle. (2) Examination of radiographs of the spine using a CT Scan or MRI. (3) Anti-tuberculosis treatment with isoniazid at 7.5mg/kg BW/day, rifampicin at 10mg/kg BW/day, and ethambutol at 20mg/kg BW/day, divided into two doses for six months. (4) PSSW operative procedure with a posterior approach (resection of spinous process lamina, transverse process, ribs, resection of pedicles, middle column, posterior wall, controlled closure of posterior defect, and cantilever Pedicle Screw Sublaminar Wiring instrumentation).15 (5) After the wound healed, patients were re-examined about neurological deficits and radiology to determine the angle of kyphosis after surgery, (6) The data obtained was processed using SPSS ver 16.0 to assess descriptively and analytically to access the association between variables.
Research variablesFrankel classificationThis method of classification is used as a system to evaluate and document the neurological progress of an individual patient, a large number of patients, or a subgroup of patients with spinal injuries following a full neurological examination.16 Data was obtained by neurological examination, and the ordinal scale was used to assess this variable.
Kyphosis angleThe angle measured from lines drawn from the superior border of the upper end vertebra and the inferior border of the lower end vertebra, with perpendicular lines drawn from the end vertebra lines to measure the intersecting angle.17 The data were obtained by an X-ray measurement. The interval scale was used to assess this variable.
Statistical analysisData was analyzed using univariate and bivariate analysis. Data on neurological deficits before and after treatment was analyzed using the Spearman test. Data of kyphosis angle before and after treatment was analyzed using the regression correlation test. Data was considered significant if P<0.05.18
ResultsA total of 18 patients participated in this study. 61.1% of them were male and 38.9% of them were female. The average age of TS patients in this study was 27.88 years. The spinal region affected was 55.6% thoracic, 27.8% thoraco-lumbar, and 16.7% lumbar (see Table 1).
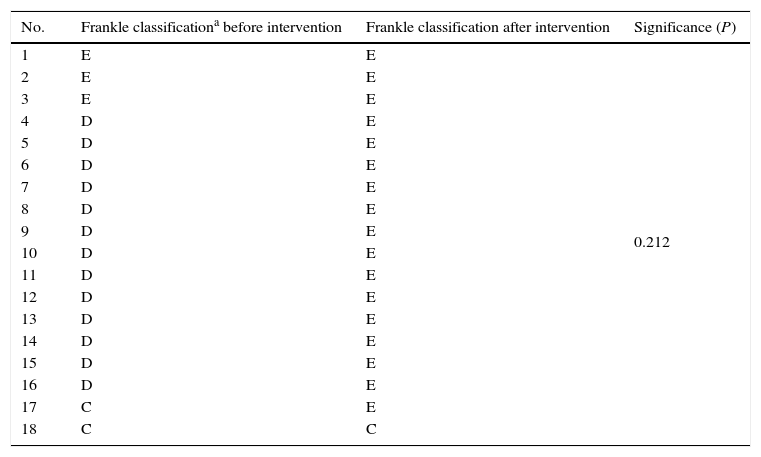
Neurological status of patients before the intervention was 11.1% Frankle C, 72.2% Frankle D, and 16.7% Frankle E. Neurological status after intervention was 5.6% Frankle C and 94.4% Frankle E (see Table 2). An explanation regarding is a Frankel classification19 is described in Table 2.
Frankel classification before and after intervention.
| No. | Frankle classificationa before intervention | Frankle classification after intervention | Significance (P) |
|---|---|---|---|
| 1 | E | E | 0.212 |
| 2 | E | E | |
| 3 | E | E | |
| 4 | D | E | |
| 5 | D | E | |
| 6 | D | E | |
| 7 | D | E | |
| 8 | D | E | |
| 9 | D | E | |
| 10 | D | E | |
| 11 | D | E | |
| 12 | D | E | |
| 13 | D | E | |
| 14 | D | E | |
| 15 | D | E | |
| 16 | D | E | |
| 17 | C | E | |
| 18 | C | C |
Frankel's classification19:
Grade A, complete loss of both motor and sensory functions.
Grade B, complete motor loss, some sensations preserved.
Grade C, motor functions present, but useless.
Grade D, motor function useful, but weak.
Grade E, neurologically intact.
Table 2 shows neurological deficits before and after the intervention. The Spearman test was performed to find an association of neurological deficits before and after the intervention. The Spearman test results obtained P=0.212 (P>0.05), and it was concluded that there was no statistically significant association between a combination of PSSW and anti-tuberculosis therapy and improvement of neurological deficits in patients with TS.
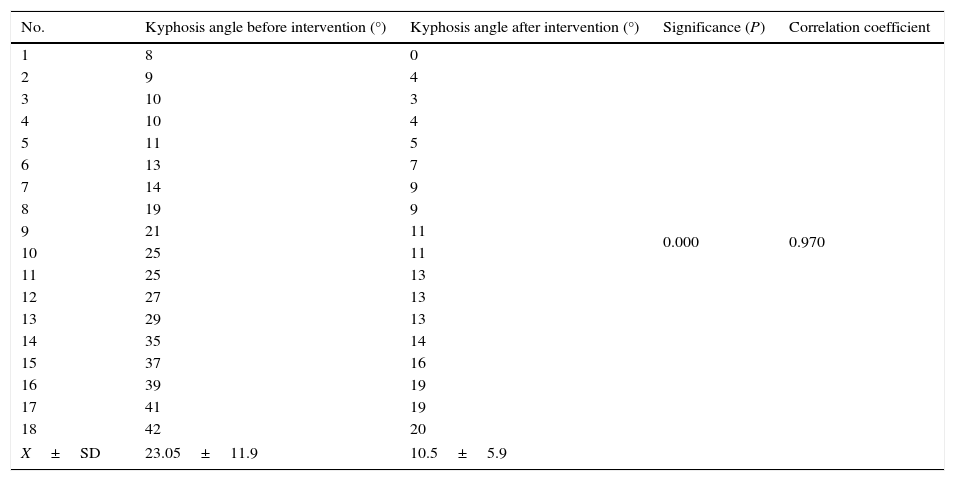
The Regression correlation test was performed to assess the degree of kyphosis before and after the intervention. It obtained P=0.000 (P>0.05), so we concluded that there was a statistically significant association between a combination of PSSW and anti-tuberculosis therapy with improved degree of kyphosis in TS patients (see Table 3).
Kyphosis angle before and after intervention.
| No. | Kyphosis angle before intervention (°) | Kyphosis angle after intervention (°) | Significance (P) | Correlation coefficient |
|---|---|---|---|---|
| 1 | 8 | 0 | 0.000 | 0.970 |
| 2 | 9 | 4 | ||
| 3 | 10 | 3 | ||
| 4 | 10 | 4 | ||
| 5 | 11 | 5 | ||
| 6 | 13 | 7 | ||
| 7 | 14 | 9 | ||
| 8 | 19 | 9 | ||
| 9 | 21 | 11 | ||
| 10 | 25 | 11 | ||
| 11 | 25 | 13 | ||
| 12 | 27 | 13 | ||
| 13 | 29 | 13 | ||
| 14 | 35 | 14 | ||
| 15 | 37 | 16 | ||
| 16 | 39 | 19 | ||
| 17 | 41 | 19 | ||
| 18 | 42 | 20 | ||
| X±SD | 23.05±11.9 | 10.5±5.9 | ||
Tuberculosis spondylitis (TS) is a secondary infection disease of the spine. TS is the most common and the most dangerous of TB infections. TS is a common musculoskeletal TB with that makes up nearly half of all cases of musculoskeletal TB.2 The incidence of TS has no difference between male and female.3 This study showed that TS was more common in males (61.1%) than females (38.9%), with the average age of patients at (27.89±2.48). These results were not much different from other studies. Several studies reported that the incidence of TS was 34.6% in females and 65.4% in males,20 39.5% in females and 60.5% in males,21 54.2% in females and 45.8% in males,22 25% in females and 75% in males,23 50% in females and 50% in males,3 48% in females and 52% in males,9 66.6% in females and 33.3% in males,24 and 1.17 per 100,000 in the female population and 0.916 per 100,000 in the male population.4
The generally affected spinal regions are often not significantly different. A review by Garg and Somvanshi8 revealed that the thoracic region of the vertebral column was most frequently affected. A study by Punamiya et al.7 showed that the spinal regions affected were 35% lumbar, 31% thoracic, 15% thoraco-lumbar, 13% cervical, and 6% cervico-thoracic. Godlwana et al.4 found that the spinal regions affected were 42% thoracic, 30%lumbar, 11% cervical, 10% thoraco-lumbar, 5% lumbosacral, and 2% sacral. Turgut3 found that the spinal regions affected were 55.8% thoracic, 22.8% lumbar, 16.9% thoracolumbar, and 4.2% cervical. Kotil et al.9 found that the most common region of Pott's disease was the thoracolumbar junction (41%), followed by the thoracic (36%), and lumbar (23%) regions. Our results found that the spinal regions affected were thoracic (55.6%), thoraco-lumbar (27.8%), and lumbar (16.7%).
This study also reported kyphosis angles and neurological deficits in patients with TS. In this study, the average angle of kyphosis in TS patients before the intervention was 23.05±11.9 and 10.5±5.9 after. Kyphosis occurs due to the destruction of the spine. Kyphosis can be found in almost all TS patients who have spinal damage in the affected region. Kyphosis occurs due to the destruction of the corpus vertebrae. It is caused by infection in the anterior region. Kyphosis has a greater tendency to occur in the thoracic region compared to other regions.25 Furthermore, this study found that Frankel D neurologic deficits occurred in 83.3% of patients, and found that 94% of patients showed an improvement of neurological status after the intervention. Neurological deficits can be found in almost all cases of TS, with manifestations such as paraplegia, paresis, reduced sensibility, or cauda equina syndrome. The manifestations of neurological deficits depends on the region of the damage. TS manifestations appear between 3 and 4 months after infection of the spine. The manifestations appeared a little longer in the lumbar region. This is due to the spinal canal of the lumbar region being wider, and thus more tolerant to neurological disorders, while the spinal canal of the thoracic region is narrow, which results in neurological symptoms appearing faster.13
A combination of anti-tuberculosis drugs and PSSW results in total management of TS. The restoration of the patient's condition is this management's goal, so that patient can return to social life, family, and the work environment.15 PSSW, or shortening procedure, is part of the total treatment approach for TS. The shortening procedure is performed by removing laminae and facet joints, precessus transversus, adjacent ribs, and middle segments until circumferential decompression of the duramater and cord is achieved. Then, the correction is performed by closing the posterior gap with posterior segmental instrumentation (cantilever pedicle screw sublaminar wiring instrumentation).26 Management of TS is different in each instance, but has the same basic principles. No study has reported a combination of PSSW and anti-tuberculosis drugs in patients with TS. However, several similar studies have reported results that were not much different from this study. Zhang et al.27 conducted a study on surgical management for multilevel noncontiguous thoracic spinal tuberculosis by single-stage posterior transforaminal thoracic debridement, limited decompression, interbody fusion, and posterior instrumentation (modified TTIF) combined with anti-tuberculosis chemotherapy for 3 months. Follow-up was conducted at 10 months after surgery. The results showed improvement in patients with TS. The kyphosis angle decreased from 19.21±12.63 to 8.07±6.91. The neurological status of the 12 patients with preoperative neurological deficits were 6 with grade D recovered to normal; 2 with grade B, both of them to grade D; 4 with grade C, 2 to grade D, 1 to grade E, and 1 still in grade C. Sahoo et al.24 conducted a study about aposterior-only approach surgery for fixation and decompression of thoracolumbar spinal tuberculosis combined with anti-tuberculosis drugs and chemotherapy for 6 months for the treatment of TS. Follow-up was observed at 24 months after surgery. The results showed that kyphosis improved from a preoperative value of 17.7±5.8 degrees to 9.4±4.6 degrees postoperatively and neurological recovery occurred in 94.4% of patients. Ma et al.28 conducted a study about the outcomes of anterior and posterior instrumentation under different surgical procedures combined with anti-tuberculosis chemotherapy for 3 weeks for treating thoracic and lumbar spinal tuberculosis in adults. The sample was divided into 2 groups. Anterior instrumentation was used in 74 patients (group A) and 83 patients (group B) were fixed posteriorly. Follow-up was observed at 12 weeks after surgery. The results found that the kyphosis degree was corrected by a mean of 11.5° in group A and 12.6° in group B, respectively. Fu et al.29 conducted a study about a combination of intensified anti-tuberculosis treatment, posterior transpedicular screw system internal fixation, intertransverse bone grafting, and an anterior approach focus debridement for the treatment of thoracolumbar tuberculosis. Follow-up was conducted at 12–23 months after surgery. The results showed that all the patients achieved successful bony fusion 6–18 months after operation, and the Cobb angle was 7–21 degrees (average 15.2 degrees) 12 months after operation, without aggravation. The Frankel grading system was used to assess postoperative neurological function. 1 patient in grade B before the operation was improved to grade C after the operation, 1 patient in grade B was improved to grade D, 1 patient in grade C was improved to grade D, 4 patients in grade B were improved to grade E, and 7 patients in grade D were improved to grade E. Xu et al.30 conducted a study on the effects of one stage surgical treatment of thoracolumbar spinal tuberculosis by anterior radical debridement with bone graft fusion and posterior pedicle screw-rod system fixation combined with anti-tuberculosis chemotherapy for 9 months. The patients were all complicated, with kyphosis deformity and an average Cobb angle of (28.0+/−9.7) degrees (before surgery). According to the Frankel neurological function grade system, there were 3 cases in grade B, 5 in grade C, 1 in grade D, and 12 in grade E (before surgery). Follow up was conducted 2.5 years after surgery. The results showed that the kyphosis deformity was corrected by 17.2 degrees in the thoracolumbar region, on average. According to the Frankel neurological functional grade system, 1 case was in grade C, 3 in grade D, and 17 in grade E (after surgery). Yang et al.31 conducted a study on the effect of one-stage anterior debridement of infection in function reconstruction of the anterior and middle column combined with anti-tuberculosis chemotherapy for 9 months for the treatment of thoracolumbar spinal tuberculosis. In 14 cases with spinal cord injury (before surgery), there were 5 cases of grade C and 9 cases of grade D, according to the Frankel classification. The kyphotic Cobb angle was 20–65 degrees (41 degrees on average). Follow-up was conducted 12 months after surgery. The results showed that at 12 months after operation, the pain disappeared, and there were 7 cases of grade D and 7 cases of grade E, according to the Frankel classification. The kyphotic Cobb angle was 0–33 degrees (24 degrees on average). This study assessed radical surgery and posterior implant placement combined with anti-tuberculosis chemotherapy for six months for the treatment of TS. The results showed that it was effective for patients with TS to correct spinal kyphosis.
ConclusionPSSW, combined with anti-tuberculosis chemotherapy for six months, was effective for patients with TS to correct spinal kyphosis, but it did not show a statistically significant difference to improve the neurological deficits although approximately 94% of the patients showed an improvement in neurological status.
Conflicts of interestThe authors have no conflicts of interest to declare.
FundingNo financial support was provided.
Thanks to the Director and staff of DGHIE-IU Jakarta and HEI-IU University of Syiah Kuala. Thanks to Director and staff of General Hospital Dr. Zainoel Abidin, Banda Aceh.