Gunshot wounds in the facial region produce important functional disabilities if they are not properly treated. They may also cause an important effect in the social and psychological development of the patient because of the aesthetic problems that they produce. This article presents a case of a 20 years-old female patient who was referred to our institution because of facial trauma secondary to a gunshot wound, whose treatment consisted of multiple reconstructive surgeries in order to obtain an adequate, functional and esthetic result. Also, we did a review of the bibliography in order to establish the proper management of the wounds found in these type of cases.
Gunshot wounds produce devastating, functional and aesthetical consequences in people,1 specifically those in the maxillofacial region. These have become a challenge for plastic and maxillofacial surgeons due to facial deformities and large scars, as well as the psychological implications which in consequence impact on the subject's image. They may even compromise the patient's life, since they compromise airway, cause massive hemorrhage, cranioencephalic and spinal cord trauma. Hence the importance of an accurate surgical management, aimed to preserve function and life, thus facilitating the adequate development and quality of life after intervention.2
Initial management of patients with these types of wounds is resuscitation, with special attention to the airway, since bleeding and inflammation usually compromise it. In order to accomplish this, either orotracheal intubation or tracheostomy, and subsequently entering to the reconstruction phase.1 Maxillofacial trauma due to firearms produce a situation of high complexity, due to the significant bone and soft tissue loss, which results in aesthetic and functional craniofacial deformities. Gunshot wounds are often linked to panfacial fractures, which involve high kinetic energy causing injuries of the adjacent tissues, which in addition to compromise the patient's life, produce severe posttraumatic deformities.3–5
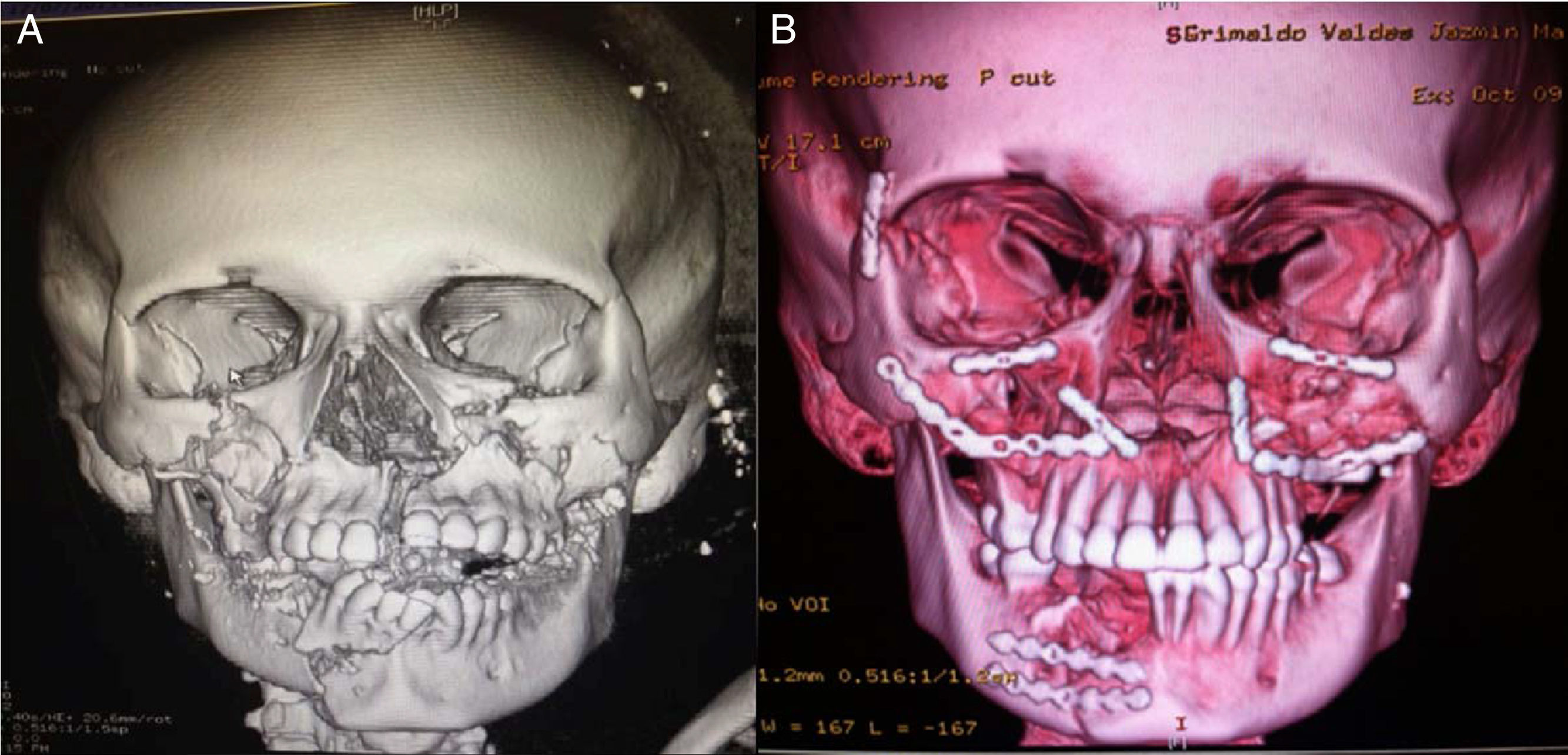
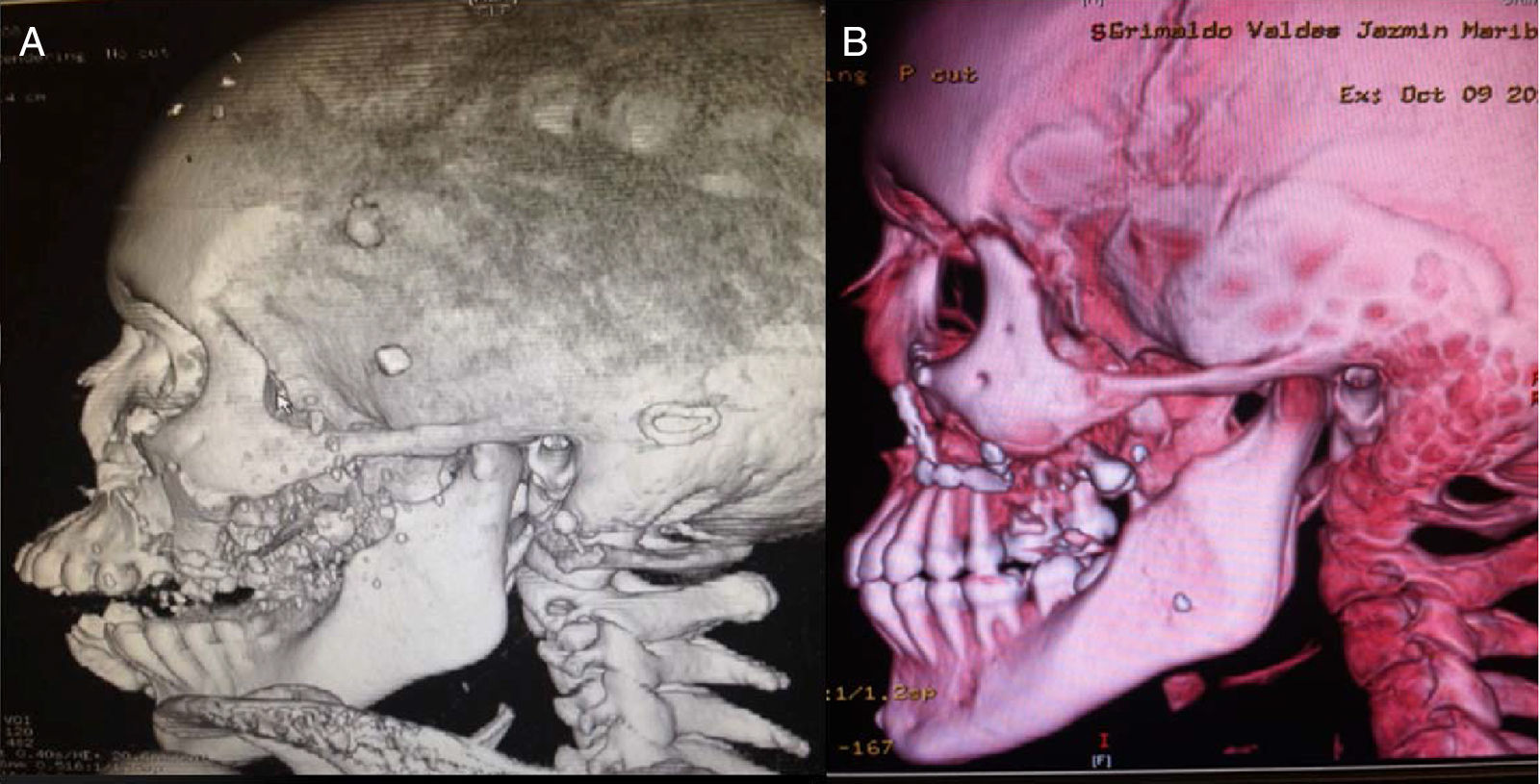
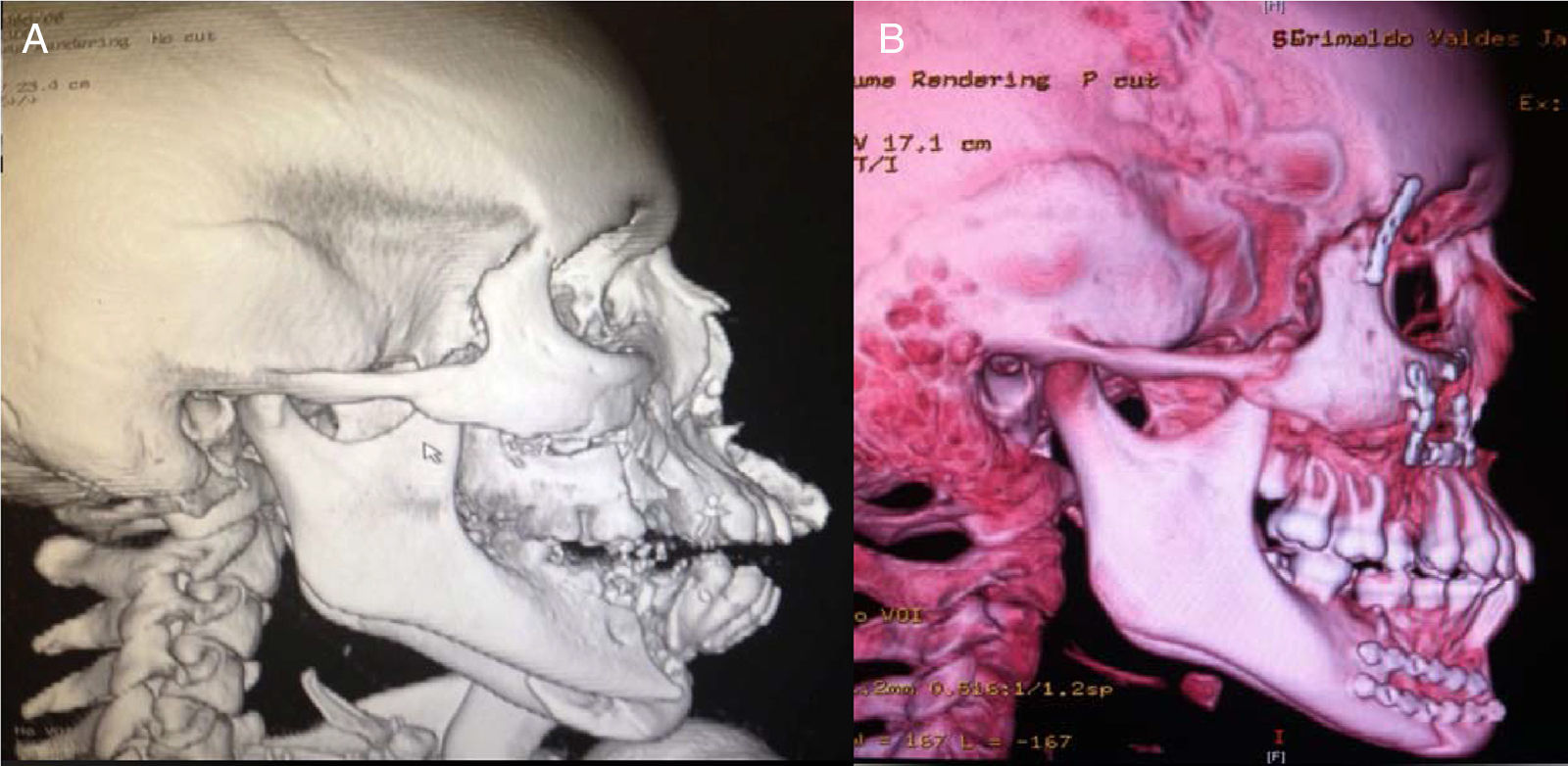
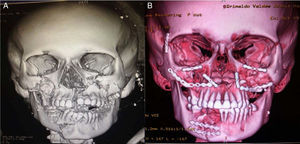
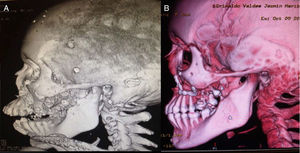
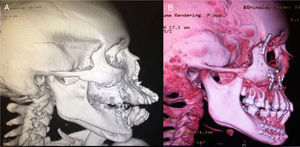
Clinical caseWe present a 20-years-old female patient with no relevant past medical history, who suffered a gunshot wound to the face with an entry hole in the left preparotideal region and an exit hole in the right cheek. Upon her arrival to the emergency services at our unit, reanimation was performed with pertinent imaging studies too. Due to the bleeding and progressive respiratory deterioration a tracheostomy was performed in order to protect the airway. The patient was assessed by the plastic surgery service where the following injuries were documented: an entry wound with a defect of 3×3cm in the left preparotideal region; an exit wound with soft tissue avulsion of 3×3cm in the right cheek region, multiple injuries in the mucose of the hard palate with comminuted fracture; a tongue injury of 13cm from the tip of it with a front to back trajectory toward the base by its right lateral edge and finishing at the posterior third. It was evident the lack of stability of the medial and inferior facial thirds due to the fractures present. Imaging studies showed comminuted fractures of both maxillary bones with involvement of both inferior periorbital borders; fracture of the body of the left malar bone; In the lower jaw, a comminuted fracture at the right mandibular body with a parasinfisiary trace and an alveolar fragment avulsion (which behave as a bone graft); and also a palatine comminuted fracture was found. (Figs. 1A, 2A and 3A)
(A) Three-dimensional reconstruction of cranial tomography. A right jaw parasymphyseal fracture with avulsion of an alveolar fragment, along with maxillary fracture, a fracture in both malar regions and fractures at the bottom of both orbits can be seen. (B) Post-procedure 3D reconstruction, where the placement of plates and the reduction of fractures can be seen.
Debridement of the cheek and preparotideal region's wounds was performed, as well as primary closure by planes. Primary closure of injuries in the mucose of the hard palate, repair of lingual injury, manual fracture reduction of hard palate with no fixation, facial medial third reduction, Erich arches placement, inter-maxillary fixation, and due to the lack of osteosynthesis material at the time of surgery, the Milton Adams technique (wire fixation from the intra-maxillary fixation to the fronto-malar union) was used. She was taken to intensive care unit, and after the hemodynamic and ventilatoryr recovery, she was moved to the plastic surgery floor area, and eventually moved to an outpatient setting. Four weeks after the first procedure, she was programmed for open reduction and permanent fixation of the fractures with mini-plates and removal of the Milton Adams fixation. A subciliary and gingivo-vestibular approach were used on both sides for zygomatic-malar and maxillary complex fixation, with 1.5 and 2.0 rigid fixation systems and an open reduction and internal fixation for the jaw fracture was performed with a two 2.0 mini-plates system. (Figs. 1B, 2B and 3B)
During follow-up, the patient presented a dento-alveolar fragment loss of the mandibular comminuted fracture (the fracture previously mention as bone graft). She remained with inter-maxillary fixation for a period of 6 weeks.
DiscussionFacial fractures constitute a substantial percentage of admissions to the plastic surgery services. At our hospital facial fracture incidence has risen due to the increase in firearm use and violence at our city.6,7,11
Over the last 15 years, facial fracture treatment has suffered a significant evolution with the introduction of craniofacial approaches, open reduction directly in the place of the fracture, and early or immediate fixation, combined with the utilization of pre-operative computed tomography for surgical planning as well as post-operative for fracture reduction assessment.8
Surgical reconstruction phases in patients with gunshot wounds have been controversial. Literature reports favor for a conservative approach, treating soft tissue first, then bone tissue. On the other hand, there are publications arguing a more aggressive intervention of involved structures, in just one reconstruction phase.10 Today, the most accepted approach is the ballistic wound reconstruction approach in phases proposed by Norman et al.8 This approach includes the following phases:(1) immediate stabilization of existing bone in anatomic positions, (2) primary closure of existing soft tissue, (3) periodic “second look” serial debridement procedures, and (4) definitive early reconstruction of soft-tissue and bony defects.
In our patient's management we decided that due to the nature of the injury and the involvement of the airway, once resolved, and due to the characteristics of the wounds and the lack of stability of the medial and lower facial thirds, a damage control surgery as an initial procedure because of the lack of osteosynthesis material at our facilities. The four-week delay to perform the second procedure (rigid systems of fixation placement) was because it was the necessary period of time to get osteosynthesis material. Finally, it is worth to mention that in the first procedure due to the lack of osteosynthesis material, after repair all soft tissue injuries, we performed a rearrangement of both dental arches. Due to the lack of stability of the middle and lower thirds, the Milton-Adams technique allowed us to give some support. By the time of the second surgery we found that the bone fragments of the middle third were in an acceptable position and with some stability, which helped us considerably in the placement of the miniplates without need to manipulate the soft tissues excessively or make large bone movements to reduce the fragments, making all of this procedure simpler that we could imagine.
Reduction and immediate rigid fixation of jaw fractures is not necessary in all patients, as in this case. Sometimes, surgical management can be different, placing interdental wire next to the fracture, or the use of Erich arches, which can afford a certain degree of stability.6 The decision to use a rigid fixation or a functionally stable fixation depends on the fracture itself, and on the load-bearing capability of the adjacent bones. Complex or comminuted fractures, like in this case, require rigid fixation.6 As a general rule, intermaxillary fixation should always precede the placement of plates, to ensure the adequate reduction of fragments.6,12
Type-3 palatal (comminuted) fractures, like those that the patient presented, usually are treated with long intermaxillary fixation, covered up with flaps if defects are present in that area.9
The patient recovered well, with adequate scarring of the soft tissues. There were no secondary effects due to the palatal and the severe tongue injury. After rehabilitation and removal of the interdental wire, we could observe that the patient developed a synechia of the tongue toward a portion of the gum over the right jaw, which was released with a local anesthesic. Due to the kinetics of the wound and its involvement of multiple dental pieces, many of them were lost, including those in the dento-alveolar fragment, which was reabsorbed due to a lack of irrigation of the same, acting as a bone graft. Nevertheless, with the adequate alignment of both jaws, the patient was recovered esthetically and functionally; and in the interdental spaces that remain a removable dental prosthesis.
ConclusionFacial trauma caused by firearm guns are complex and difficult to manage. Current treatment involves a variety of stagged procedures, adhering to the protocols of management and treating each fracture as a unit. With the advent of rigid fixation (plates and screws), patients results have improved notably, and now we are able to help patients to return to their functional activities quickly, and with a better social adaptation. We would like to emphasize that, despite the lack of the rigid fixation material at the beginning of the approach to the patient, it was possible for us to obtain good results using basic principles for the management of complex facial fractures (Erich arches and Milton Adams technique).
Conflict of interestThe authors have no conflicts of interest to declare.