Good syndrome is a rare condition in which a thymoma is associated with hypogammaglobulinemia. It is also characterized by low or absent B-cells, CD4+ T-cell lymphopenia, inverted CD4/CD8+ T-cell relation, and repeated bacterial, viral, and fungal infections, as well as with various autoimmune disorders.
Case reportWe report the case of a 62-year-old female patient who after resection of a thymoma developed constipation and recurrent lower respiratory and urinary tract infections. She underwent left hemicolectomy as well as symptomatic and antibiotic treatment. Two years later the patient develops refractory anemia; a bone marrow biopsy shows hypo-cellularity and no red cell precursors with negative CD 71 staining. The diagnosis of pure red cell precursor aplasia (PRCA) is made. Recurrent bacterial infections of the respiratory and urinary tracts continue, and therefore treatment with G and A immunoglobulins starts. Finally, the absence of B lymphocytes and inversion of CD4/CD8 relation confirms the diagnosis of Good syndrome associated with PRCA.
DiscussionThe discovery of Good Syndrome and PRCA after the resection of a thymoma, as seen in the current case, is very unusual. This case illustrates both the rareness presentation of Good syndrome with PRCA and the persistent infections seen in these patients. Early recognition of these entities results in lower mortality and morbidity.
Thymoma is the most common type of malignancy of the anterior mediastinum (47%).1–3 Symptoms vary greatly in relation to the former's anatomical situation. However, this neoplasm is linked with several paraneoplastic syndromes, such as, myasthenia gravis, which is the most frequent one, occurring in approximately 10–45% of cases.4–7 Thymoma has also been related to pure red cell aplasia (PRCA), occurring in 5–15% of the cases, and hypogammaglobulinemia in the 5%.4,5 When a thymoma is associated with immunodeficiency, it is called Good syndrome. This rare condition was first recognized by Robert Good in 1954 as the association of hypogammaglobulinemia, a decrease of B lymphocyte count and altered CD4/CD8 T lymphocyte ratio in association with thymoma.8 It increases the susceptibility to opportunistic infections related to the B and T cell deficiency, such as autoimmunity, bacterial, viral, and fungal infections.9–11 The treatment of this condition is the surgical removal of the thymoma due to their potential for malignancy, and the administration of intravenous immunoglobulin to prevent infections. Complete resection of the thymoma is an important prognostic factor and should always be sought, even when it involves the resection and reconstruction of an important thoracic structure.2
As mentioned before, pure red cell aplasia also relates to thymoma. This entity is characterized by normocytic anemia, reticulocytopenia, and absence of erythroid precursors in the bone marrow. Its treatment consists of the surgical removal of the tumor and immunosuppressive drugs. The coexistence of Good syndrome and pure red cell aplasia is very rare, and to our knowledge, there are only 20 cases reported in the literature with such combination. Therefore, Good syndrome should be suspected in patients with hematological and autoimmune diseases that occur with unusual infections.
We describe the case of a Latin female with a rare association between Good syndrome and PRCA.
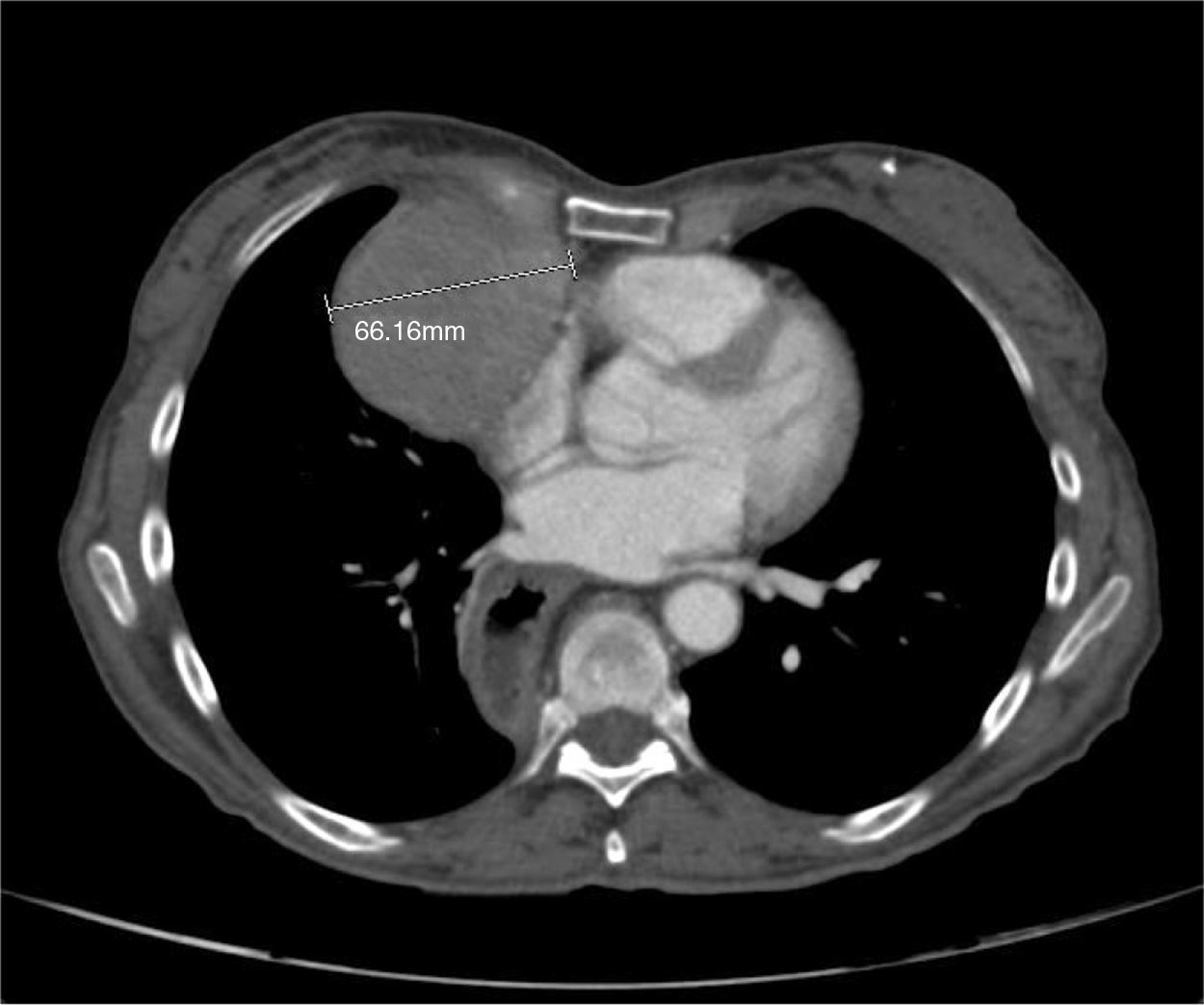
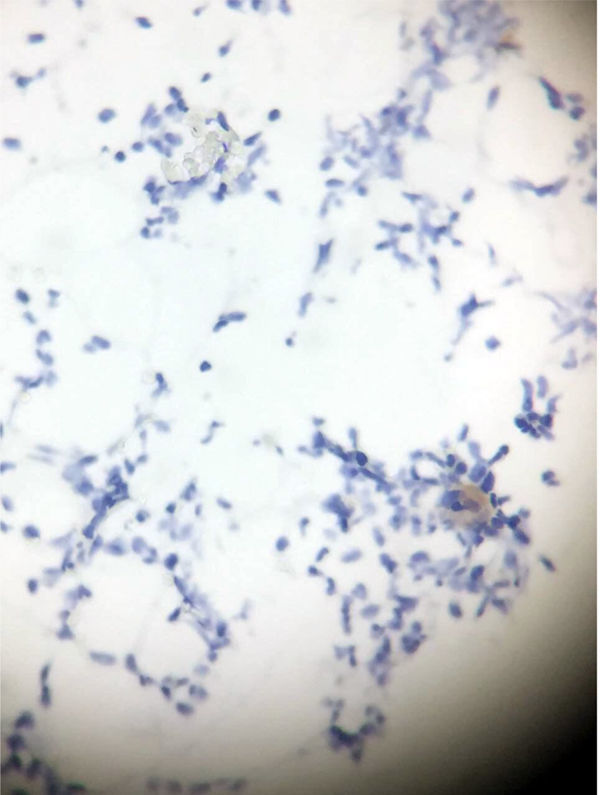
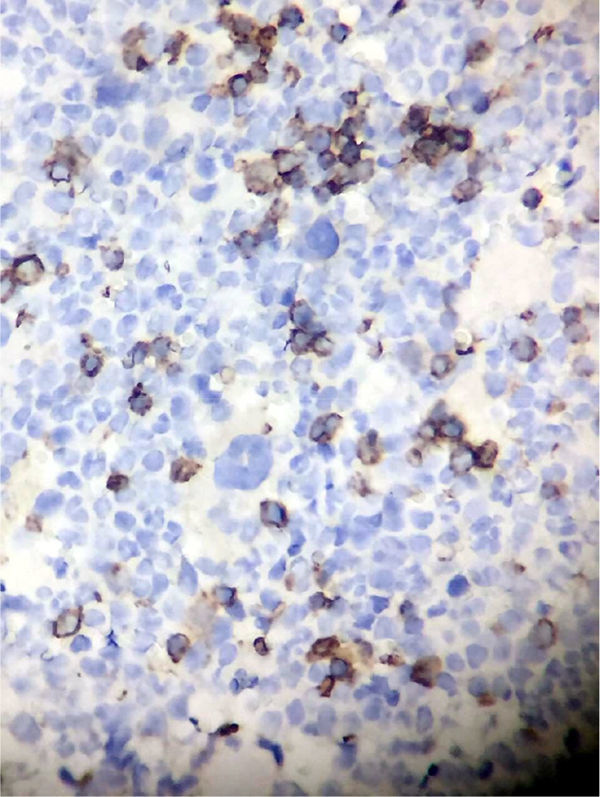
Clinical presentationA 62-year-old female patient presents with a diagnosis of achalasia and a gastric bypass surgery in 2013. In August 2014 she underwent surgery because of a mediastinal tumor that was fully resected (see Images 1–3) and was reported histopathologically as type C thymoma. After the surgery, she evolved torpidly with multiple gastrointestinal symptoms that lead to the need of a left hemicolectomy, as well as symptomatic treatment for constipation, reflux (related to the previous esophageal surgery), recurrent lower respiratory and urinary tract infections. In March 2016, she was referred to a Hematology consultation for the assessment of a refractory anemia and high transfusion requirements. During the initial assessment, we found a reticulocyte count of 0.6% with a hemoglobin of 4.9g/dl, hematocrit of 14.25%, MCV of 96fl, platelets and leukocytes in normal ranges, elevated erythropoietin levels, iron profiles with 97% transferrin saturation and ferritin 829. Bone marrow morphologic evaluation found erythroid lineage to be inexistent with some giant pro-erythroblasts, and the flow cytometry revealed that no erythroid precursors were detected. The bone marrow biopsy was reported as hypo-cellular at the expense of the absence of red cell precursors with negative CD 71 staining (see Images 4 and 5) the diagnosis of pure red cell aplasia was concluded. Due to recurrent bacterial infections of the respiratory and urinary tracts, immunoglobulin levels were evaluated, resulting in immunoglobulin A (IgA) 16 (reference levels of 60–392mg/dl) and immunoglobulin G (IgG) 108 (reference levels of 710–1540mg/dl). We then evaluated lymphocyte subpopulation, detecting a complete absence of B lymphocytes and inversion of CD4/CD8 relation. With this information, we concluded that the patient had Good syndrome associated with PRCA. This diagnosis confirms the immunosuppressive state seen in the patient and explains its predisposition for recurrent infections.
The patient initiated treatment for intravenous immunoglobulin G to keep its levels above 700mg/dl and therefore reducing the risk of infections. The treatment for the PRCA began with cyclosporine since the patient rejected the use of corticoids. The patient persisted with high transfusion requirements and developed deep venous thrombosis in the left subclavian vein (site of insertion of a central venous catheter with subcutaneous port), so we started treatment with anticoagulants. Infectious endocarditis was later evidenced so the use of cyclosporine was suspended and the patient received long-term treatment with antibiotics. Once the antimicrobial scheme was completed we decided to resume immunosuppression with 1mg/kg/day of prednisone associated to tacrolimus, 2mg every 12h, due to cyclosporine intolerance. The patient evolution was torpid with further infectious complications despite immunoglobulin and antimicrobial treatment. Transfusion requirements diminished for a period of 2–3 months and increased later on again to the basal pre-treatment requirements. Because of the nonresponsiveness to the immunosuppressive drugs and infectious complications, we decided to stop tacrolimus and start prednisone. The patient developed autoimmune encephalitis in August 2017 (we discarded the infectious causes of encephalitis) and began treatment with high doses of methylprednisolone without any improvement in neurological or hematological conditions. Finally, she passed away secondary to complications of hospital-acquired pneumonia.
DiscussionGood syndrome is a rare condition in which a thymoma associates with hypogammaglobulinemia. It is characterized by low or absent B-cells, CD4+ T-cell lymphopenia, inverted CD4/CD8+ T-cell relation, and repeated bacterial, viral, and fungal infections, as well as with various autoimmune disorders. Good syndrome generally presents itself in the fourth or fifth decade of life, with a similar frequency in males and females.12 In the treatment of this syndrome, it is based on the resection of the thymoma and the restitution of the immunoglobulin levels.
The association with autoimmune diseases as myasthenia gravis, pure red cell aplasia, pernicious anemia, diabetes mellitus and idiopathic thrombocytopenia may be present in these patients.13 The association between Good Syndrome and PRCA is extremely rare.4,5,14–16 To our knowledge there are only around 20 cases reported worldwide and most of them have been reported in patients of Asian ancestry.4,14,15 The response rate of patients with PRCA to the thymectomy ranges from 25 to 30%, yet Good syndrome generally does not disappear after surgery.15 In our case, both paraneoplastic affections were detected long after the thymectomy and without any evidence of relapse using different imaging studies. The discovery of Good Syndrome and PRCA after the resection of a thymoma, as seen in the current case, is very unusual.5 The patient mentioned in this case presented various infectious events despite the replenishment of immunoglobulin G, causing the immunosuppressive treatment to be suspended on several occasions.
The importance of this case lies in the rareness of Good syndrome and PRCA simultaneously presented in this patient. As well as their presence in a patient of Latin American origin, since there is evidence of only one other case like this in a patient from Chile, and the rest have been documented on patients of European or Asian ancestry. Early recognition of these entities results in lower mortality and morbidity. Therefore further studies have to be done to improve patient results.
Conflict of interestThe authors have no conflicts of interest to declare.