Miscarriages are a common complication of pregnancy that can cause psychological and physical distress. This loss may be followed by a period of mourning, so multiple studies have evaluated the quality of life in patients with miscarriages with subsequent medical or surgical treatment, reporting data suggesting that these patients may develop symptoms of depression and anxiety after the procedure.
MethodWe conducted a cross-sectional, survey type analysis of patients with diagnosis of miscarriage who were surgically treated (MVA/D&C). A HADS survey for assessment of depression and anxiety symptoms was applied.
ResultsOne hundred and twenty patients were enrolled with a diagnosis of miscarriage and were surgically treated, of these patients 41.7% reported symptoms suggestive of depression and/or anxiety at some degree. When analyzing the relationship between a history of depression and symptoms of anxiety or depression post-abortion, a significant positive relationship was established (p=0.002).
ConclusionThe application of surveys for symptoms of anxiety or depression is a useful, in-hospital tool to diagnose patients who are prone to any of these entities allowing diagnosis and treatment.
Depression is a mood disorder which causes a state of unhappiness that can be provisional or permanent. The World Health Organization suggests that for the year 2020, depression will be the second cause of work incapacity.1 Anxiety may be defined as an anticipation of future damage or misfortune, accompanied by a feeling of dysphoria and/or somatic symptoms of tension.2 Approximately 15–25% of women at fertile age will present a miscarriage, having medical and psychological consequences.3 The term ‘miscarriage’ refers to the interruption of gestation where the endometrial lining – which is assessed via ultrasonography – is greater than 15mm.4 Moreover, some of the ovular-placental tissues are not completely expelled in a miscarriage, in some cases requiring surgical removal via curettage, the use of oxytocics and even blood transfusions.
When there is a miscarriage diagnosis, treatment may vary based on the gestational age. If the miscarriage occurred below 12 weeks of gestation, the ideal treatment is MVA (manual vacuum aspiration); when it is over 12 weeks of gestation, the treatment is uterine curettage.5
Two weeks after the abortion, the percentage of women who suffer from significant depressive symptoms is 3.4 times greater compared to pregnant women, and 4.3 times higher than the general population.6 Many studies have assessed the magnitude of these symptoms, reporting numbers at 20% and even up to 55% of patients.5 Depression occurs up to 8 times more frequently after delivery rather than after a miscarriage. However, it is present in those cases as well.7
Compared to the general population, women who had a miscarriage obtained higher scores in the HADS (Hospital Anxiety and Depression) scale 10 days after the miscarriage.8
In this article, the study of anxiety and depression symptoms is assessed in women who suffered a miscarriage and were surgically treated with MVA or D&C. The objective of the study is to determine the incidence of anxiety and depression symptoms in our population, as well as to detect whether or not variables like age, marital status, parity, schooling and occupation may exacerbate these symptoms.
Materials and methodsA cross-sectional, survey-type analysis which included patients who attended the gynecology and obstetrics consultation from April to September 2015, was performed at a third level hospital 10–14 days after having a miscarriage diagnosis and surgical treatment with either MVA or D&C, to carry out the HADS questionnaire. The present research was approved by the ethics committee of the institution.
Patients with diagnosis of miscarriage that were treated at our Institution who attended post-treatment control, were included. We excluded those patients who did not come to post-treatment control and/or those who were not treated in our service, as well as patients with a poor filling of the surveys.
The HADS was introduced by Zigmund and Snaith in 1983,9 it has a predictive value for the detection of symptoms of depression and anxiety, and has been translated into more than 25 languages.10 The translation into Spanish and its validation was made by Tejero, Guimerá, Farré and Peri (1986).11 Specifically, in Mexico, it has been validated by demonstrating adequate diagnostic properties.12,13 The HADS is a self-administered questionnaire with a response time of approximately ten minutes. The instructions ask the patient to describe how they have felt during the last week, including the day of the test. It consists of fourteen questions, seven in relation to anxiety and seven in relation to depression. The response options are Likert-type, and range from zero to three, giving a minimum score of zero and a maximum of 21 for each subscale. Originally, cutoff points from zero to seven implied the absence of clinically relevant anxiety and/or depression, from eight to ten requiring consideration (borderline), and from 11 to 21 the presence of relevant symptomatology and a probable case of anxiety and/or depression.14
Using a formula for calculating a finite population proportion of 830 patients treated during the year 2014, with an unknown expected proportion of 0.1% (10%), a 95% confidence interval and 5% accuracy, 119 patients were required.
The included variables to analyze were age, marital status, schooling, gestation, gestational age, history of depression and/or anxiety.15 The data were analyzed using the statistical program SPSS v. 17. For the quantitative variables, measures of central tendency and dispersion were estimated. The qualitative variables were analyzed through chi-square. A 95% confidence interval was considered.
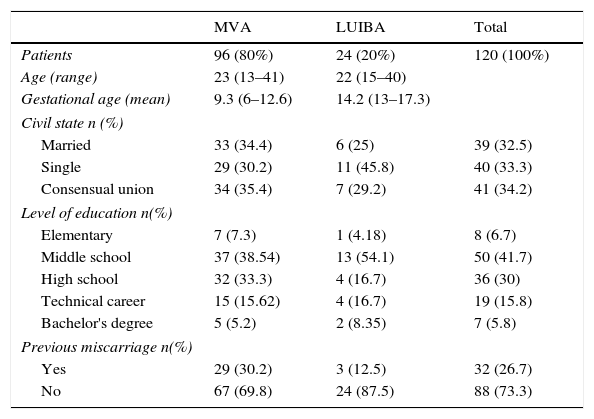
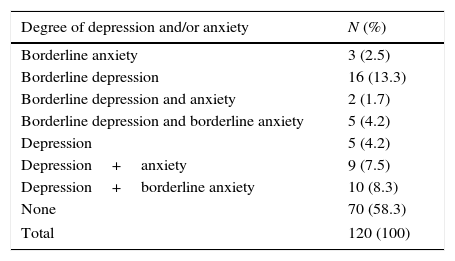
ResultsA total of 120 patients were recruited, the description of their demographic characteristics is presented in Table 1. Of the total number of patients, 50 (41.7%) were diagnosed with some degree of depression or anxiety on the applied scale. Of these, 3 (2.5%) were classified as borderline for anxiety without data of depression and 16 (13.3%) were classified as borderline for depression without data for anxiety. Tests for 5 (4.2%) patients resulted in depression data only. Twenty-six patients had symptoms of depression and anxiety to some degree, 2 (1.7%) patients showed anxiety and borderline data for depression, 5 (4.2%) showed borderline data for both diseases, 9 (7.5%) showed joint data for depression and anxiety, and the remaining 10 (8.3%) showed data on depression and borderline anxiety (Table 2).
Demographic characteristics according to treatment received.
| MVA | LUIBA | Total | |
|---|---|---|---|
| Patients | 96 (80%) | 24 (20%) | 120 (100%) |
| Age (range) | 23 (13–41) | 22 (15–40) | |
| Gestational age (mean) | 9.3 (6–12.6) | 14.2 (13–17.3) | |
| Civil state n (%) | |||
| Married | 33 (34.4) | 6 (25) | 39 (32.5) |
| Single | 29 (30.2) | 11 (45.8) | 40 (33.3) |
| Consensual union | 34 (35.4) | 7 (29.2) | 41 (34.2) |
| Level of education n(%) | |||
| Elementary | 7 (7.3) | 1 (4.18) | 8 (6.7) |
| Middle school | 37 (38.54) | 13 (54.1) | 50 (41.7) |
| High school | 32 (33.3) | 4 (16.7) | 36 (30) |
| Technical career | 15 (15.62) | 4 (16.7) | 19 (15.8) |
| Bachelor's degree | 5 (5.2) | 2 (8.35) | 7 (5.8) |
| Previous miscarriage n(%) | |||
| Yes | 29 (30.2) | 3 (12.5) | 32 (26.7) |
| No | 67 (69.8) | 24 (87.5) | 88 (73.3) |
Frequency of diagnosis of anxiety or depression.
| Degree of depression and/or anxiety | N (%) |
|---|---|
| Borderline anxiety | 3 (2.5) |
| Borderline depression | 16 (13.3) |
| Borderline depression and anxiety | 2 (1.7) |
| Borderline depression and borderline anxiety | 5 (4.2) |
| Depression | 5 (4.2) |
| Depression+anxiety | 9 (7.5) |
| Depression+borderline anxiety | 10 (8.3) |
| None | 70 (58.3) |
| Total | 120 (100) |
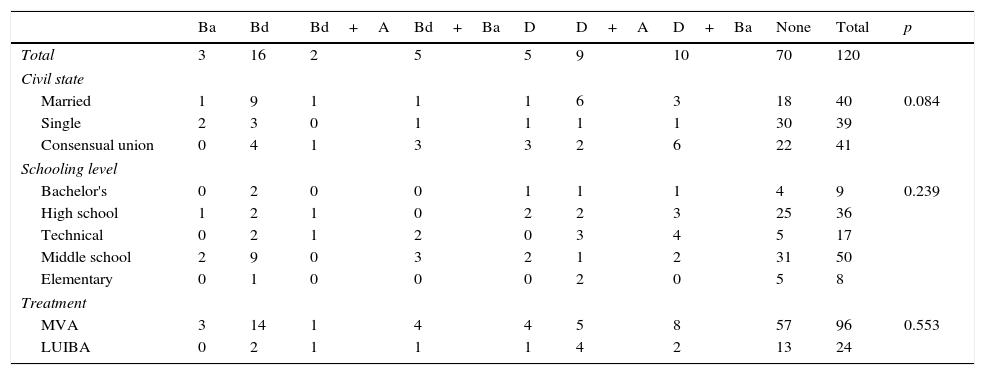
Reviewing the HADS results according to the treatment group, of the 96 patients treated with MVA, 57 (59%) showed no data on depression or anxiety, while the remaining 39 (41%) showed some evidence of depression and/or anxiety. 24 patients were treated with D&C, of which 13 (54%) did not show data on depression or anxiety; the remaining 11 (46%) reported depression or anxiety to some degree (Table 3).
Frequency of diagnosis of anxiety and/or depression according to marital status, schooling and treatment.
| Ba | Bd | Bd+A | Bd+Ba | D | D+A | D+Ba | None | Total | p | |
|---|---|---|---|---|---|---|---|---|---|---|
| Total | 3 | 16 | 2 | 5 | 5 | 9 | 10 | 70 | 120 | |
| Civil state | ||||||||||
| Married | 1 | 9 | 1 | 1 | 1 | 6 | 3 | 18 | 40 | 0.084 |
| Single | 2 | 3 | 0 | 1 | 1 | 1 | 1 | 30 | 39 | |
| Consensual union | 0 | 4 | 1 | 3 | 3 | 2 | 6 | 22 | 41 | |
| Schooling level | ||||||||||
| Bachelor's | 0 | 2 | 0 | 0 | 1 | 1 | 1 | 4 | 9 | 0.239 |
| High school | 1 | 2 | 1 | 0 | 2 | 2 | 3 | 25 | 36 | |
| Technical | 0 | 2 | 1 | 2 | 0 | 3 | 4 | 5 | 17 | |
| Middle school | 2 | 9 | 0 | 3 | 2 | 1 | 2 | 31 | 50 | |
| Elementary | 0 | 1 | 0 | 0 | 0 | 2 | 0 | 5 | 8 | |
| Treatment | ||||||||||
| MVA | 3 | 14 | 1 | 4 | 4 | 5 | 8 | 57 | 96 | 0.553 |
| LUIBA | 0 | 2 | 1 | 1 | 1 | 4 | 2 | 13 | 24 | |
Ba: borderline anxiety, Bd: borderline depression, A: anxiety, D: depression.
The marital status of the patients with anxiety or depression was analyzed. Forty (33.3%) patients were married, of which 22 (55%) reported some degree of depression and/or anxiety and 18 (45%) did not report suggestive data from any of these entities. Of the 41 patients (34.2%) who were in consensual union, 19 (46%) reported a pathology in the HADS survey and the remaining 22 (54%) showed no alteration. The remaining 39 (32.5%) patients belonged to the single patient group, of which 9 (23%) patients reported depression and/or anxiety data, while the remaining 30 (77%) did not report data suggestive of anxiety or depression (Table 3).
Of the total of 120 patients, 47 (39.1%) were primigravidae, of which we found that 12 (25.53%) reported symptoms of anxiety or depression according to HADS, 4 (33.3%) showed a borderline diagnosis for anxiety and depression diagnosis, 2 (16.6%) showed a borderline diagnosis for anxiety and depression, 2 (16.6%) showed a diagnosis for borderline depression, 1 (8.3%) had a diagnosis of anxiety and depression, 1 (8.3%) showed borderline anxiety, 1 (8.3%) had a diagnosis of anxiety and 1 had a diagnosis of depression. The remaining 73 (60.8%) patients were multiparous; 39 (53.42%) reported symptoms of anxiety and depression according to HADS, with 13 (33.3%) borderline cases for depression, 8 (20.5%) cases for anxiety and depression, 8 (20.5%) showed borderline anxiety and borderline depression diagnosis, 3 (7.8%) had borderline anxiety and depression, 3 (7.8%) with a diagnosis of anxiety and borderline depression, 3 (7.8%) with symptoms of depression, and one (2.6%) with borderline anxiety. Although the tendency of multiparous patients to develop symptoms of depression and anxiety was observed, the result was not statistically significant (p>0.423).
When HADS was applied to patients with a history of depression, 9 (81.8%) had more than 8 points on the scale, 3 (33.3%) had a borderline diagnosis for depression, 2 (22.2%) were found to be depressed, 2 (22.2%) were diagnosed with symptoms of anxiety and depression and 2 (22.2%) had depression.
According to the HADS, in the MVA group, 8 patients had history of depression, 6 (75%) were diagnosed with anxiety and depression, described as follows; 4 (66.6%) cases with a borderline diagnosis of depression and two (33.3%) with a diagnosis of depression and borderline anxiety. Of the 3 patients in the D&C group, 3 (100%) reported post-scale anxiety and depression symptoms as follows: two (66.6%) patients were diagnosed with anxiety and depression and one (33.3%) was diagnosed with borderline anxiety and depression. When analyzing the relationship between the history of depression and post-miscarriage depression, a highly significant positive relationship was established (p=0.002).
Of the total of 120 patients, 32 (26.6%) had a previous history of miscarriages. According to the group, 29 (90.63%) patients were treated with MVA and 3 (9.37%) patients with D&C treatment had history of previous miscarriages. Of the 32 patients with previous miscarriages, 2 had a history of 2 previous losses, one patient had a previous abortion and diagnosis of depression according to the scale with 13 points. However, she only had 1 point on the anxiety scale. Finally, one patient had 7 previous miscarriages and, according to the HADS scale, had the highest score, with 16 points for depression (16/16) and 12 (12/16) for anxiety. There was no statistically significant difference between the two groups in relation to miscarriages and depression, according to the type of procedure (p=0.179).
DiscussionSince 1992, the relationship between miscarriages and anxiety disorders and depression, and how it affects the psychology of women, has been addressed. Depression is a state of mind where the emotional state is affected, producing symptoms such as insomnia, changes in eating patterns, sadness and even suicidal thoughts. Anxiety is a disorder characterized by anxiety, tension, a sense of threat and panic attacks.16 The duration of this distress will not depend on the duration of the pregnancy, but on the relationship of the mother to the fetus. For women who have experienced multiple miscarriages, the emotional distress caused by each is cumulative, with greater depression, distress, dysphoria, unhappiness, and a sense of loss of control over their reproductive choices.17
There are risk factors that predominantly coexist with anxiety and depression, thus a correlation of both symptoms of 2%–69% according to previous literature, including factors as maternal age, perinatal factors and history of psychiatric illness.18
Due to the fact that it has been reported in the literature that patients with spontaneous abortions had a broader symptomatology,8 in the present study, the symptoms of anxiety and depression were assessed based on the HADS questionnaire.
An article using the HADS questionnaire to measure symptoms of anxiety and depression was published in Oslo, Norway in December 2005; It was a longitudinal study of 5 years, where the questionnaire was applied at an interval of 10 days, 6 months, two and five years, in addition to the Impact of Event Scale (IES) questionnaire. This study included 120 patients. However, it is important to clarify that only 40 had a miscarriage, while the remaining 80 had an induced abortion, because the latter is legal in that country. Women who had an induced abortion had higher anxiety scores throughout the time interval, while women who had had a miscarriage only had higher levels within 10 days.
In the present study, patients who were treated by means of MVA had a mean gestational age of 9.3 (6–12.6) weeks, and the D&C group had a mean gestational age of 14 (13–17.3) weeks. The average gestational age described in the literature is 10–11 weeks.19 In relation to the gestational weeks and the symptoms of anxiety and depression, 5 controlled studies have been reported that sought to find the impact of gestational age with the symptoms of depression, having controversy in their results, since, although two of these studies demonstrated that there is an increased risk of developing depression and anxiety at a higher gestational age, the other three did not report a relationship between these variables.20,21 It is described in the literature that gestational age is not the only variable that predisposes a patient to the development of these symptoms, but rather that it is the mother–fetus relationship in terms of attachment in addition to maternal age, schooling and gestation number.22 In the present study, gestational age was not statistically related (p>0.226) to incidence of post-miscarriage depression or anxiety.
In this research, the average age of the patients was 23 years, which does not correspond to what is described in the literature, since other researchers refer to patients in a later age range, with an average age of 35–40 years.23
Regarding the patients who suffer most from depression and anxiety and the age group, in this study, the group of 26–30 year-old was the most affected, corresponding to the results found in the literature.24 However, as a single factor for diagnosis, according to the HADS questionnaire, this variable was not statistically significant (p>0.356).
In our study, it was observed that married patients had a higher incidence of symptoms of depression and anxiety, being up to 50% of the cases. This variable corresponds to that described in the literature, which reports on a study where more than four thousand patients were evaluated, that those who were married had a 138% higher probability of clinical depression after a previous miscarriage versus those who had completed their first pregnancy. Single women in this study reported only 30% of predictable miscarriages, while married women reported 74%. According to the authors, this may make the results of married women more reliable.25,26
Regarding parity in the present study, multiparous patients were more prone to the development of anxiety and depression. Although this trend was observed, the result was not statistically significant (p>0.423). This coincides with what has been mentioned by other authors, who refer to multiparous women as having the greatest symptoms of depression, but it is important to clarify that certain articles divide parity as term pregnancies and consider the history of miscarriages as another variable.27
In the present study, almost 40% of the patients with a history of previous miscarriages had some type of symptoms in relation to anxiety and/or depression on the HADS scale, without being statistically significant (p>0.891). We reported a case of a patient with multiple previous miscarriages with very high values on the scale. In the literature, the clinical history of previous miscarriages in relation to developing depression or anxiety is described as a risk factor. Stress associated with repetitive miscarriages has been widely studied, especially in patients treated with assisted reproduction methods, since spontaneous miscarriages occur more frequently. It has been described that the risk of spontaneous post-abortion depression is cumulative, presenting a higher risk of suffering depression in greater degree, besides anxiety.28
Perhaps the most important variable in the patient clinical history for the psychological evaluation of patients with spontaneous miscarriages is precisely the history of depression, since in our study, approximately 82% of the patients (9/11 patients) with this variable reccurred (p<0.002). This justifies psychological assistance or care that is not applied in our environment, although it is necessary, emphasizing the patients with a history of previous spontaneous miscarriages.
There are many ways to help and guide patients and their partners. Couples should be prepared for the possibility of a loss even before they become pregnant. If a spontaneous miscarriage occurs, the couple should be informed that this type of loss is common and multifactorial. In addition to this, the feeling of guilt must be clarified, since it has been reported that, on many occasions, the couple lives with difficulty because they assume responsibility for the loss without having processed it, causing greater difficulty in the assimilation and acceptance of it. Therefore, it is also essential for them to know about the risks of future miscarriages, regardless of what happened in their current situation.29
Among the limitations of this study is the number of patients included in the study, since, although it exceeds that required by the sample calculation, an increase in the number of patients analyzed could provide a clearer and more accurate view of the psychological consequences in this population. Therefore, we suggest that more extensive studies that take the emotional implications of patients after this type of event should be carried out, as well as their responses to therapy or psychological support provided by specialists in the field.
In summary, it can be concluded that about 72% of the participants experienced either anxiety, depression or both, regardless of the method used (MVA/D&C) to resolve their miscarriage. The group most affected by anxiety and/or depression was the group of patients between 26 and 30 years of age, who were married, multiparous and with an undergraduate education, while those who were the least affected were those in the group of 36–40 year olds, who were single, nulliparous and with a middle school level of education. The Hospital Anxiety and Depression Scale is a useful tool for diagnosing patients who are prone to presenting symptoms of anxiety and depression.
Ethical disclosuresProtection of human and animal subjectsThe authors declare that the procedures followed were in accordance with the regulations of the relevant clinical research ethics committee and with those of the Code of Ethics of the World Medical Association (Declaration of Helsinki)
Confidentiality of dataThe authors declare that they have followed the protocols of their work center on the publication of patient data.
Right to privacy and informed consentThe authors have obtained the written informed consent of the patients or subjects mentioned in the article. The corresponding author is in possession of this document.
FundingNo financial support was provided.
Conflict of interestThe authors have no conflicts of interest to declare.