In recent years there has been an extensive national and international debate on whether residency years constitute a risk to the mental health of the resident physician.1 The specialty training period involves a level of general activation and coping with new situations that most residents find stimulating and rewarding. However, for others it may mean an increase in the body's response to stress, which, when prolonged in time and intensity, does not allow adequate adaptation, and leads to psychobiological exhaustion or burnout.2
Stress is a term used to refer to the state of anti-homeostatic biological activation that occurs when the body fails in its attempts to adapt to the demands of its immediate environment.3 This biological activation is accompanied by unpleasant emotions (anxiety, sadness, irritation) and by physiological modifications of the adaptive subsystems (autonomic and neuroendocrine activation and immune and behavioural inhibition) that decrease the capacities to maintain homeostasis when interacting with the environment. Therefore, stress is a complex biological state that results from the cerebral processing of the subject's interaction with the environment,3 which is specific to each person, and which will also depend on the threatening stimulus (e.g., more intense in social threats than in physical ones).3 Uncontrollable stress is a biological state of transition to disease3 and can precipitate various cardiovascular, digestive, musculoskeletal diseases, as well as mental disorders such as anxiety and depression.3,4
Work stress can be defined as the response that occurs when work demands, and pressures do not correspond to the knowledge and skills of the worker and exceed his/her ability to cope.2 All workers experience pressure at work, but when the individual perceives that the demands are beyond his or her resources to cope, work stress and the risk of burnout2 may occur. On the other hand, and according to the effort-reward model at work,3 the risk of stress and psychosomatic disorders would occur when effort is not compensated by reward factors, such as salary, recognition, career advancement or job security.
Although the weight of the work environment is key in burnout, chronic work-related stress affects the biological functioning of the body. The feeling of lack of control in the face of the multiple stressors faced by doctors on a daily basis can in some cases lead to a state of uncontrollable stress, affecting brain functioning. From a neurobiological perspective, there is increasing evidence to support the biological substrate of the syndrome,4 whereby a prefrontal cortex dysfunction exerts a top-down regulatory effect on cognition, behaviour, and mood. The prefrontal cortex is involved in many cognitive functions essential to the medical profession, such as abstract reasoning, decision-making, working memory, insight and empathy.4 Chronic uncontrollable work stress can lead to a decrease in motivation, concentration, impaired working memory, organisational skills, decision-making, insight and empathy, characteristic of the worker with burnout.
The current COVID-19 pandemic situation carries a high degree of uncertainty, causing a significant impact on the mental wellbeing of healthcare workers, especially those who work on the frontline or who have been exposed to extreme and continuous pressure, causing physical exhaustion, emotional stress, stigmatisation and insomnia.5 Before the COVID-19 pandemic, health professions were already considered as highly stressful.5 Research on stress in medical residents has shown that this group of professionals is particularly vulnerable and has a high proportion of burnout.6 Obviously, not all doctors are equally vulnerable, and a number of risk factors have been identified related to the individual (e.g. socio-demographic variables or personality traits), to the healthcare profession itself (e.g. dealing with serious illnesses or long working hours) and to the organisation of care (e.g. excessive workload or lack of oversight).2,6 In general, professionals can function with high levels of stress if their work gives them positive feedback, which will depend on the degree of resilience and the presence of protective factors.7
Traditionally, the burnout syndrome has been clinically diagnosed using Maslach's burnout scale (Maslach Burnout Inventory [MBI]), which assesses the 3 main dimensions of the syndrome: emotional exhaustion, depersonalization and personal accomplishment.8Emotional exhaustion refers to the experience of being emotionally exhausted by the demands of work. Depersonalization assesses the degree to which each one recognizes attitudes of unfeeling and impersonal response from the recipients of their care. Finally, the personal accomplishment dimension assesses feelings of self-efficacy and accomplishment at work.8
The American Psychiatric Association's classification of mental disorders, the DSM-5 (2013), does not include burnout syndrome as a specific disease, but rather it is included in other problems that can be the object of medical care, in this case related to employment. However, in 2019 the World Health Organisation has officially recognised burnout as an occupational phenomenon following the ratification of the eleventh revision of the International Statistical Classification of Diseases and Related Health Problems (ICD-11), which is due to come into force on 1 January 2022.9 Thus, the burnout syndrome has been identified as one of the main mental health problems and the prelude to many mental disorders resulting from this syndrome's poor control and lack of primary prevention. This already challenging situation will be exacerbated by the high stress that caring for COVID-19 patients places on many health care workers, including resident doctors. Resident doctors have had their current clinical care work and training programme disrupted and are experiencing particularly stressful situations.
In this context, the aim of this paper has been to provide an update through a literature review of the main evidence on burnout in medical residents, its prevalence, risk, and protective factors, before and during the COVID-19 pandemic.
MethodologyA review was made of publications in English or Spanish on burnout in residents in PubMed databases for the last 5 years (2016–2020), as well as publications referring to the first wave of the COVID-19 pandemic. The keywords "burnout", "resident training", "prevalence", "risk factors", "Maslach Burnout Inventory", "Oldenburg Burnout Inventory" and "COVID-19" and the Boolean operators AND and OR were used. Studies with samples smaller than 50 subjects and non-observational studies have been ruled out. Literature reference lists have been used to identify additional studies. Finally, a subgroup of studies with a higher degree of evidence was selected, with a preference for systematic reviews with or without meta-analysis for data on prevalence and longitudinal studies regarding risk factors and protection of burnout in residents.
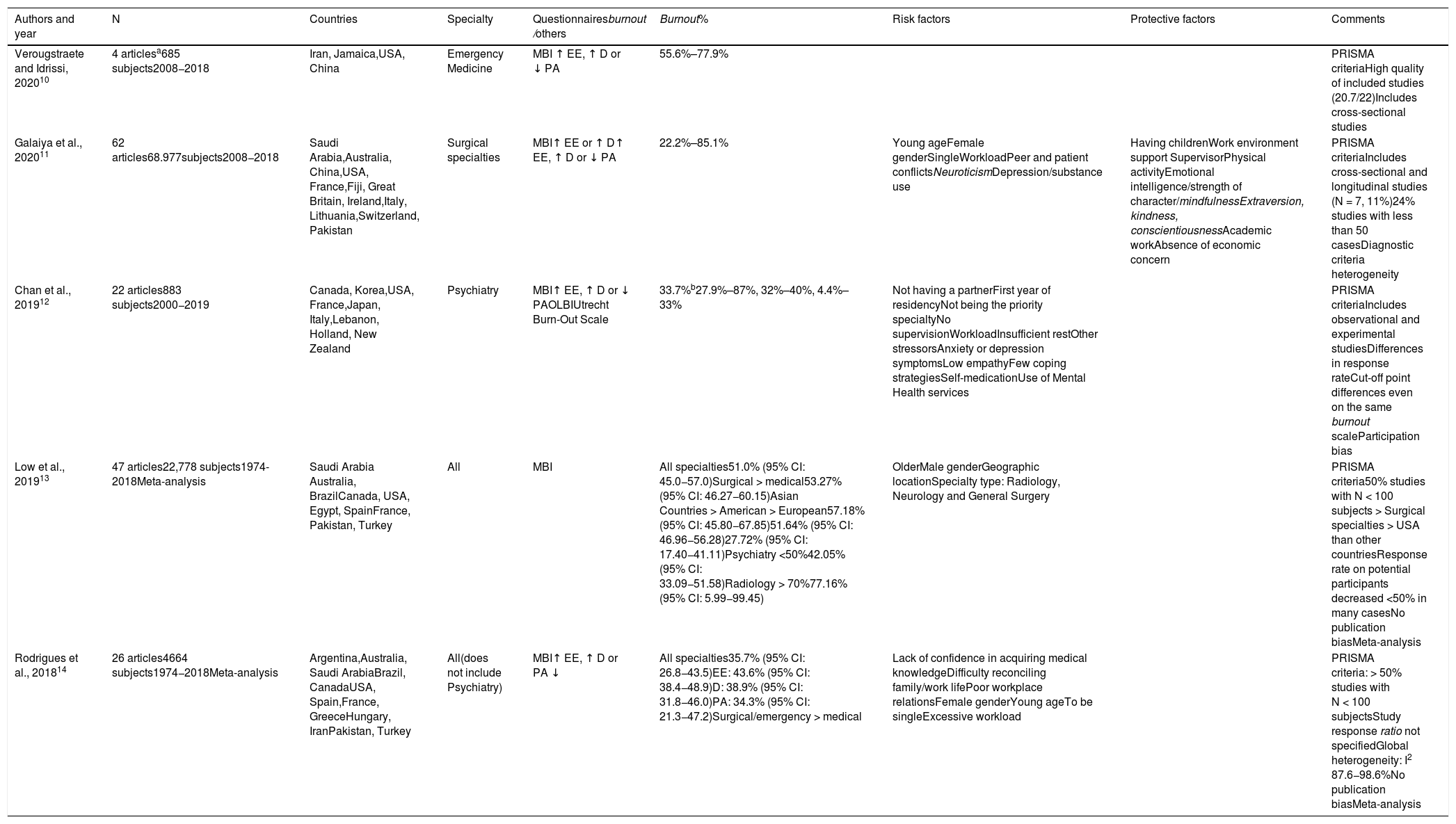
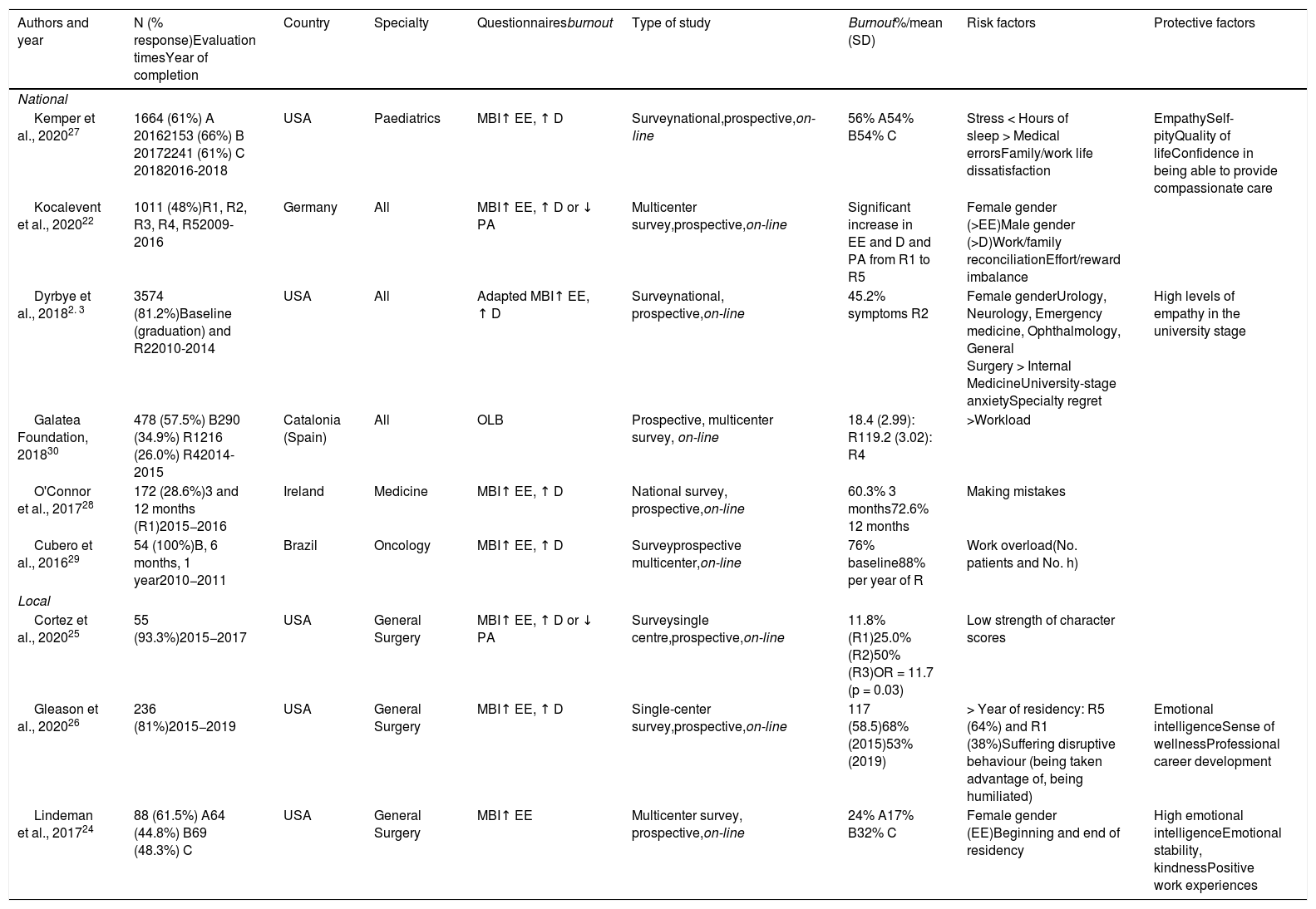
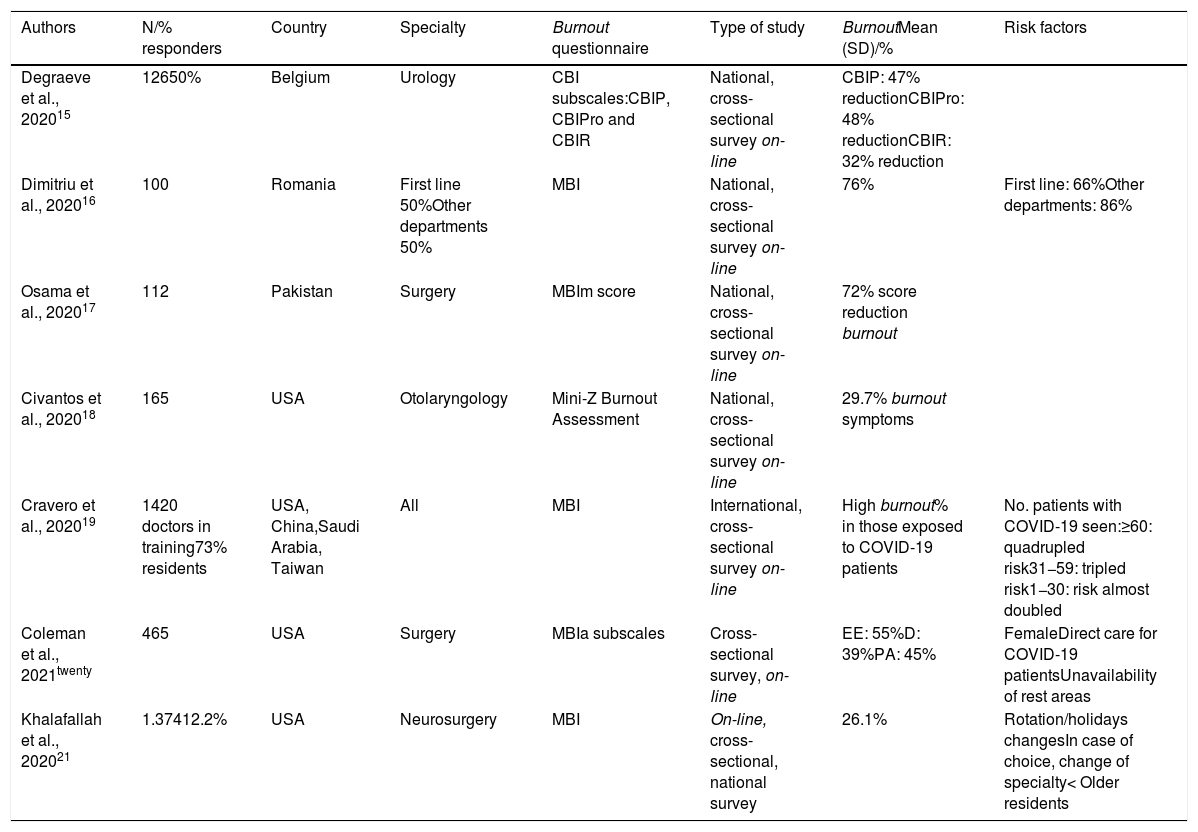
Stress and burnout during residencyA total of 210 studies published in these years were found in the literature search Thirteen were excluded due to duplication, 77 due to being studies in other samples (e.g., medical students), 8 due to sample size, 13 due to being non-observational studies (e.g., clinical trials) or not relevant to the study subject. Two systematic reviews and a longitudinal article were included from the literature review. Of the total of the selected studies (N = 98), 5 were systematic reviews with and without meta-analysis, 9 longitudinal studies and the rest were cross-sectional studies (N = 84), 7 during the pandemic. Table 1 shows the results of burnout prevalence data from systematic reviews and Table 2 shows the results of risk factors in longitudinal studies. Finally, Table 3 shows the results of cross-sectional studies of prevalence and risk factors associated with burnout in residents during the first wave of the COVID-19 pandemic.
Systematic reviews on the prevalence and risk factors of the burnout syndrome in residents published in the last 5 years in PubMed (using the Maslach or Oldenburg burnout scales).
| Authors and year | N | Countries | Specialty | Questionnairesburnout /others | Burnout% | Risk factors | Protective factors | Comments |
|---|---|---|---|---|---|---|---|---|
| Verougstraete and Idrissi, 202010 | 4 articlesa685 subjects2008−2018 | Iran, Jamaica,USA, China | Emergency Medicine | MBI ↑ EE, ↑ D or ↓ PA | 55.6%–77.9% | PRISMA criteriaHigh quality of included studies (20.7/22)Includes cross-sectional studies | ||
| Galaiya et al., 202011 | 62 articles68.977subjects2008−2018 | Saudi Arabia,Australia, China,USA, France,Fiji, Great Britain, Ireland,Italy, Lithuania,Switzerland, Pakistan | Surgical specialties | MBI↑ EE or ↑ D↑ EE, ↑ D or ↓ PA | 22.2%–85.1% | Young ageFemale genderSingleWorkloadPeer and patient conflictsNeuroticismDepression/substance use | Having childrenWork environment support SupervisorPhysical activityEmotional intelligence/strength of character/mindfulnessExtraversion, kindness, conscientiousnessAcademic workAbsence of economic concern | PRISMA criteriaIncludes cross-sectional and longitudinal studies (N = 7, 11%)24% studies with less than 50 casesDiagnostic criteria heterogeneity |
| Chan et al., 201912 | 22 articles883 subjects2000−2019 | Canada, Korea,USA, France,Japan, Italy,Lebanon, Holland, New Zealand | Psychiatry | MBI↑ EE, ↑ D or ↓ PAOLBIUtrecht Burn-Out Scale | 33.7%b27.9%–87%, 32%–40%, 4.4%–33% | Not having a partnerFirst year of residencyNot being the priority specialtyNo supervisionWorkloadInsufficient restOther stressorsAnxiety or depression symptomsLow empathyFew coping strategiesSelf-medicationUse of Mental Health services | PRISMA criteriaIncludes observational and experimental studiesDifferences in response rateCut-off point differences even on the same burnout scaleParticipation bias | |
| Low et al., 201913 | 47 articles22,778 subjects1974-2018Meta-analysis | Saudi Arabia Australia, BrazilCanada, USA, Egypt, SpainFrance, Pakistan, Turkey | All | MBI | All specialties51.0% (95% CI: 45.0−57.0)Surgical > medical53.27% (95% CI: 46.27−60.15)Asian Countries > American > European57.18% (95% CI: 45.80−67.85)51.64% (95% CI: 46.96−56.28)27.72% (95% CI: 17.40−41.11)Psychiatry <50%42.05% (95% CI: 33.09−51.58)Radiology > 70%77.16% (95% CI: 5.99−99.45) | OlderMale genderGeographic locationSpecialty type: Radiology, Neurology and General Surgery | PRISMA criteria50% studies with N < 100 subjects > Surgical specialties > USA than other countriesResponse rate on potential participants decreased <50% in many casesNo publication biasMeta-analysis | |
| Rodrigues et al., 201814 | 26 articles4664 subjects1974−2018Meta-analysis | Argentina,Australia, Saudi ArabiaBrazil, CanadaUSA, Spain,France, GreeceHungary, IranPakistan, Turkey | All(does not include Psychiatry) | MBI↑ EE, ↑ D or PA ↓ | All specialties35.7% (95% CI: 26.8−43.5)EE: 43.6% (95% CI: 38.4−48.9)D: 38.9% (95% CI: 31.8−46.0)PA: 34.3% (95% CI: 21.3−47.2)Surgical/emergency > medical | Lack of confidence in acquiring medical knowledgeDifficulty reconciling family/work lifePoor workplace relationsFemale genderYoung ageTo be singleExcessive workload | PRISMA criteria: > 50% studies with N < 100 subjectsStudy response ratio not specifiedGlobal heterogeneity: I2 87.6−98.6%No publication biasMeta-analysis |
MBI: Maslach burnout inventory and its dimensions (EE: emotional exhaustion, D: depersonalization and PA: personal accomplishment); OLBI: Oldenburg burnout inventory.
Longitudinal studies of burnout syndrome in residents published in the last 5 years in PubMed (using Maslach's or Oldenburg's burnout inventories).
| Authors and year | N (% response)Evaluation timesYear of completion | Country | Specialty | Questionnairesburnout | Type of study | Burnout%/mean (SD) | Risk factors | Protective factors |
|---|---|---|---|---|---|---|---|---|
| National | ||||||||
| Kemper et al., 202027 | 1664 (61%) A 20162153 (66%) B 20172241 (61%) C 20182016-2018 | USA | Paediatrics | MBI↑ EE, ↑ D | Surveynational,prospective,on-line | 56% A54% B54% C | Stress < Hours of sleep > Medical errorsFamily/work life dissatisfaction | EmpathySelf-pityQuality of lifeConfidence in being able to provide compassionate care |
| Kocalevent et al., 202022 | 1011 (48%)R1, R2, R3, R4, R52009-2016 | Germany | All | MBI↑ EE, ↑ D or ↓ PA | Multicenter survey,prospective,on-line | Significant increase in EE and D and PA from R1 to R5 | Female gender (>EE)Male gender (>D)Work/family reconciliationEffort/reward imbalance | |
| Dyrbye et al., 20182. 3 | 3574 (81.2%)Baseline (graduation) and R22010-2014 | USA | All | Adapted MBI↑ EE, ↑ D | Surveynational, prospective,on-line | 45.2% symptoms R2 | Female genderUrology, Neurology, Emergency medicine, Ophthalmology, General Surgery > Internal MedicineUniversity-stage anxietySpecialty regret | High levels of empathy in the university stage |
| Galatea Foundation, 201830 | 478 (57.5%) B290 (34.9%) R1216 (26.0%) R42014-2015 | Catalonia (Spain) | All | OLB | Prospective, multicenter survey, on-line | 18.4 (2.99): R119.2 (3.02): R4 | >Workload | |
| O'Connor et al., 201728 | 172 (28.6%)3 and 12 months (R1)2015−2016 | Ireland | Medicine | MBI↑ EE, ↑ D | National survey, prospective,on-line | 60.3% 3 months72.6% 12 months | Making mistakes | |
| Cubero et al., 201629 | 54 (100%)B, 6 months, 1 year2010−2011 | Brazil | Oncology | MBI↑ EE, ↑ D | Surveyprospective multicenter,on-line | 76% baseline88% per year of R | Work overload(No. patients and No. h) | |
| Local | ||||||||
| Cortez et al., 202025 | 55 (93.3%)2015−2017 | USA | General Surgery | MBI↑ EE, ↑ D or ↓ PA | Surveysingle centre,prospective,on-line | 11.8% (R1)25.0% (R2)50% (R3)OR = 11.7 (p = 0.03) | Low strength of character scores | |
| Gleason et al., 202026 | 236 (81%)2015−2019 | USA | General Surgery | MBI↑ EE, ↑ D | Single-center survey,prospective,on-line | 117 (58.5)68% (2015)53% (2019) | > Year of residency: R5 (64%) and R1 (38%)Suffering disruptive behaviour (being taken advantage of, being humiliated) | Emotional intelligenceSense of wellnessProfessional career development |
| Lindeman et al., 201724 | 88 (61.5%) A64 (44.8%) B69 (48.3%) C | USA | General Surgery | MBI↑ EE | Multicenter survey, prospective,on-line | 24% A17% B32% C | Female gender (EE)Beginning and end of residency | High emotional intelligenceEmotional stability, kindnessPositive work experiences |
B: baseline; MBI: Maslach burnout inventory and its dimensions (EE: emotional exhaustion, D: depersonalization and PA: personal accomplishment); OLBI: Oldenburg burnout inventory; R1: first year of residency; R4: fourth year of residency.
Studies on burnout syndrome in residents during the first wave of the COVID-19 pandemic in 2020.
| Authors | N/% responders | Country | Specialty | Burnout questionnaire | Type of study | BurnoutMean (SD)/% | Risk factors |
|---|---|---|---|---|---|---|---|
| Degraeve et al., 202015 | 12650% | Belgium | Urology | CBI subscales:CBIP, CBIPro and CBIR | National, cross-sectional survey on-line | CBIP: 47% reductionCBIPro: 48% reductionCBIR: 32% reduction | |
| Dimitriu et al., 202016 | 100 | Romania | First line 50%Other departments 50% | MBI | National, cross-sectional survey on-line | 76% | First line: 66%Other departments: 86% |
| Osama et al., 202017 | 112 | Pakistan | Surgery | MBIm score | National, cross-sectional survey on-line | 72% score reduction burnout | |
| Civantos et al., 202018 | 165 | USA | Otolaryngology | Mini-Z Burnout Assessment | National, cross-sectional survey on-line | 29.7% burnout symptoms | |
| Cravero et al., 202019 | 1420 doctors in training73% residents | USA, China,Saudi Arabia, Taiwan | All | MBI | International, cross-sectional survey on-line | High burnout% in those exposed to COVID-19 patients | No. patients with COVID-19 seen:≥60: quadrupled risk31−59: tripled risk1−30: risk almost doubled |
| Coleman et al., 2021twenty | 465 | USA | Surgery | MBIa subscales | Cross-sectional survey, on-line | EE: 55%D: 39%PA: 45% | FemaleDirect care for COVID-19 patientsUnavailability of rest areas |
| Khalafallah et al., 202021 | 1.37412.2% | USA | Neurosurgery | MBI | On-line, cross-sectional, national survey | 26.1% | Rotation/holidays changesIn case of choice, change of specialty< Older residents |
CBI: Copenhagen Burnout Inventory (burnout subscales: CBIP: personal; CBIPro: professional; CBIR: relational); MBI: Maslach burnout scale and dimensions (EE: emotional exhaustion, D: depersonalization, and PA: personal accomplishment); MBIa: abbreviated Maslach burnout inventory; Mini Z-Burnout assessment: consists of a single burnout assessment item.
The results of the systematic reviews carried out in recent years show a high prevalence of burnout syndrome in resident physicians, ranging between 30 and 50%.10–14 A systematic review with meta-analysis, which included 47 cross-sectional and cohort observational studies with more than 22,000 residents from different specialties and from various countries in Europe, Asia, and America, found a 51.0% mean prevalence of burnout using Maslach's questionnaire (95% CI: 45.0%–57.0%).13 This prevalence was higher than that found in a previous meta-analysis that included 26 cross-sectional studies from different countries, with almost 5000 residents of medical and surgical specialties assessed with the same questionnaire, 35.7% (95% CI: 26.8%–43.5%)14 (Table 1).
Since the onset of the COVID-19 pandemic several studies have investigated its impact on the occurrence of burnout in medical residents showing a wide range of prevalence, between 26% and 76%.15,16 This may be due to the heterogeneity of the studies conducted, for example, using different burnout17,18 assessment scales. Some of the studies found higher prevalence depending on the number of COVID-19 patients seen.19,20 Others found prevalence lower than those obtained before the pandemic with the same assessment itools21 (Table 3).
Individual and psychosocial factors related to the occurrence of stress and burnout syndrome during residencySociodemographic variablesThere are a wide variety of individual and work factors that can affect burnout rates in resident physicians.
First, sociodemographic variables have been analysed. Regarding gender, the results are contradictory. In a systematic review by Low et al. (2019),13 male gender was a risk factor, as was being older, while in Rodrigues et al. (2018) it was being a woman and being young.14 However, the results of longitudinal studies seem to confirm an increased risk for women22–24 (Tables 2 and 3).
With respect to the burnout dimensions, it seems that there could be sociodemographic differences. Thus, there are studies that show that women score more in emotional exhaustion and men in depersonalization.22 In relation to marital status, being married or with a partner appears to be a protective factor,1,12 as does responsibility for childcare, contrary to what might be assumed.11
As to cultural differences, the review by Low et al. (2019),13 which includes studies from several Asian countries, found a higher burnout syndrome prevalence in Asia, close to 60%, compared to 30% in European residents, without reaching statistical significance (Table 1).
During the pandemic, several studies found that the female gender is a risk factor for burnout.20 This greater vulnerability in women may be related to the already known propensity to develop anxiety and depression (Table 3).
Personality traitsNeurotic and introverted personalities have been associated with a higher risk of burnout, with extroversion being a protective factor.11 As well as emotional stability, kindness24 and strength of character.25 On the other hand, several studies have found that emotional intelligence and empathy are strong predictors of well-being during residency and are protective against burnout.23,24,26,27 In terms of coping styles, those based on emotional reactions (self-blame, anger, irritation, self-concern) seem to be a risk factor for developing burnout.12
The relationship between personality factors and the occurrence of stress or burnout in residents has not yet been studied in this pandemic period.
Type of specialty and year of residencyAnother debated issue is the possible difference in terms of the chosen specialty. In a systematic review by Low et al. (2019),13 Radiology, Neurology and General surgery were the specialties with the highest prevalence of burnout syndrome in its residents (>60%), followed by Internal Medicine, Traumatology, Dermatology, Gynaecology and Neurosurgery (50%), and those of Medical Oncology and Family Medicine (40%). The studies that included Psychiatry residents (N = 245) showed a prevalence of 43%.12,13 Data from Rodrigues et al. (2018)14 show that prevalence was higher in surgical and emergency specialties (40%) compared to medical specialties (25%). In relation to other factors, it has been described that both the first year and the last year of residency,24 other recent stressful events15,28 and dissatisfaction with the chosen specialty12,23 constitute risk factors for burnout (tables 1 and 2).
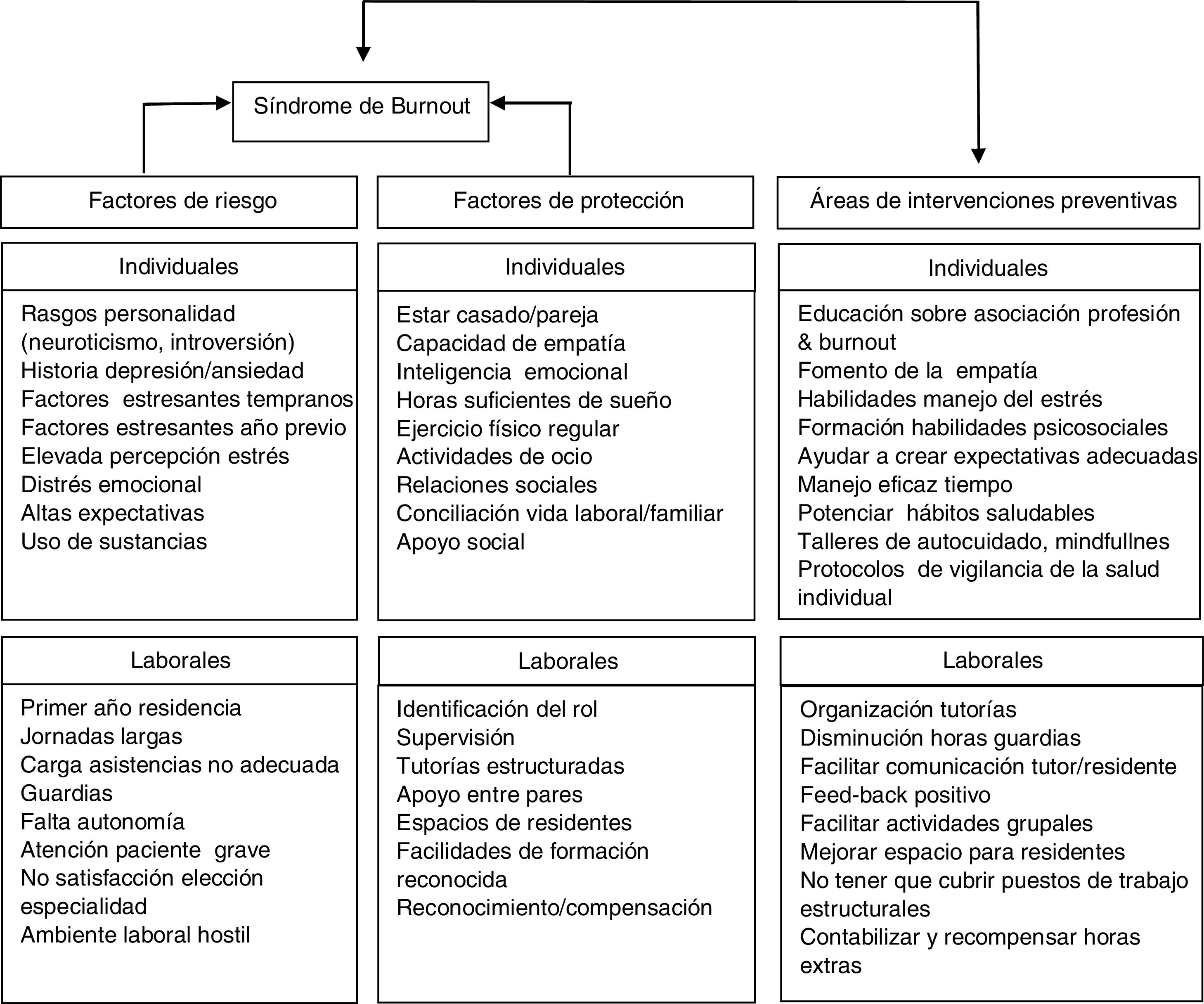
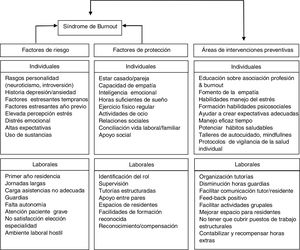
Most of the studies on burnout among resident physicians during the COVID-19 pandemic that we have found were cross-sectional and conducted in surgical specialties15,17,20,21. This group has had to move on many occasions to other units, such as Intensive Care Units or specific care wards for COVID-19 patients, which is an added stress factor.21 During the pandemic, being a first-year resident was also a risk factor for burnout.21 This fact reflects the need not to neglect the mentoring of especially younger residents at this time (Table 3) (Fig. 1).
Working conditionsA high workload with excessive working hours, a hostile work environment and generally poor workplace conditions have been reported as risk factors for the occurrence of stress and burnout8,12,22,29,30 among residents. Poor oversight and support, not having an identifiable manager, poor relationships with superiors and diminished perception of peer support are other risk factors that may contribute to poor adaptation and have been associated with the development of stress and burnout in residents12,22,26,30 (Fig. 1). There are many differences in practice depending on the type of hospital. General, university hospitals may generate more tension due to high internal competition, although they tend to have a higher number of residents per year and from different specialties, which favours a peer support network. Smaller hospitals create more cohesive work groups, with a more familiar environment that can mitigate the effects of stress.30
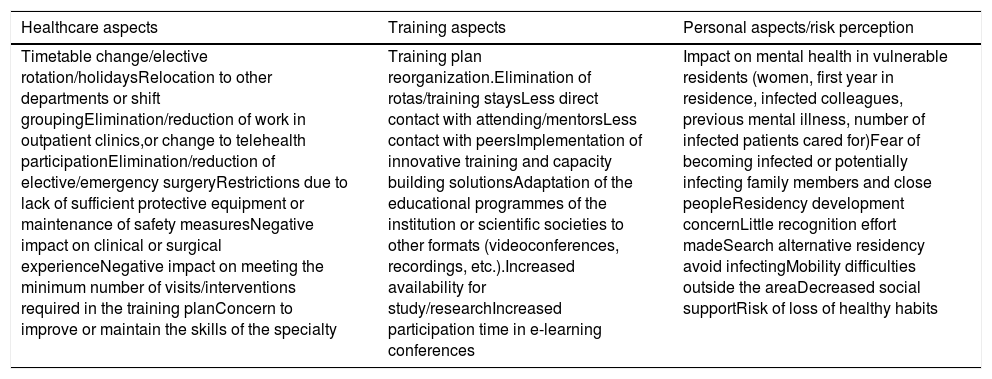
During the pandemic, the large hospitals with the greatest number of Intensive Care Unit beds have been the hospitals that have treated the greatest number of COVID-19 patients, which, on the one hand, has led to a high number of residents being in the front line of action, generating a situation of uncertainty and insecurity and great added work stress.18 However, the existence of clear protocols, practical trainings with staff on protective measures, access and proper use of protective equipment have acted as protective factors for burnout16,19,20 (Tables 3 and 4).
Impact of the COVID-19 pandemic on resident doctors in the following dimensions: healthcare, training and personal.
| Healthcare aspects | Training aspects | Personal aspects/risk perception |
|---|---|---|
| Timetable change/elective rotation/holidaysRelocation to other departments or shift groupingElimination/reduction of work in outpatient clinics,or change to telehealth participationElimination/reduction of elective/emergency surgeryRestrictions due to lack of sufficient protective equipment or maintenance of safety measuresNegative impact on clinical or surgical experienceNegative impact on meeting the minimum number of visits/interventions required in the training planConcern to improve or maintain the skills of the specialty | Training plan reorganization.Elimination of rotas/training staysLess direct contact with attending/mentorsLess contact with peersImplementation of innovative training and capacity building solutionsAdaptation of the educational programmes of the institution or scientific societies to other formats (videoconferences, recordings, etc.).Increased availability for study/researchIncreased participation time in e-learning conferences | Impact on mental health in vulnerable residents (women, first year in residence, infected colleagues, previous mental illness, number of infected patients cared for)Fear of becoming infected or potentially infecting family members and close peopleResidency development concernLittle recognition effort madeSearch alternative residency avoid infectingMobility difficulties outside the areaDecreased social supportRisk of loss of healthy habits |
An important aspect of residency training is emergency and on-call training. For some residents it is a stimulating activity, while for others it is a source of high anticipatory anxiety, extreme professional difficulty, and fear of making mistakes.27,28,30 Studies have shown that on-call duty is one of the most stressful situations for residents.10 This is compounded by many factors, inexperience, situations of poor oversight, the risk of making mistakes, dealing with potentially life-threatening situations and the regular disruption of circadian rhythms. Objectively, the study of the hypothalamic-pituitary-adrenal axis during an on-call period shows that the plasma cortisol concentration curve over the course of an on-call day is significantly higher than that of a day without an on-call period, regardless of the year of residency.31
During the pandemic, the emergency department has been a frontline site of care for patients with COVID-19, overloading an already high-stress activity for residents16 (Table 4).
Protective stress factors and burnout during residencyHours and quality of sleepOne of the factors that can contribute to and even predict the occurrence of stress and burnout is the decrease in sleep hours (< 6 h) and alteration of the circadian rhythm. This relationship holds even when considering other variables, such as work demand or work pressure or thoughts about work during leisure time.32 Poor quality of sleep and decreased hours of sleep have been observed as specific risk factors for burnout in residents of different specialties.12,27 The longitudinal survey of residents from all over Catalonia in 2018 showed that before starting the residency only 10% of residents slept less than 6 h a day, a year into the residency this was the case for 50% of them and at the end of the residency it reached 60%. The decrease in sleeping hours was related to the increase in the number of working hours.30 Sleep deprivation and fatigue are known to produce metabolic and physiological abnormalities that lead to cognitive deficits.4 Therefore, paying attention to this aspect could be a relatively easy way to decrease the risk of burnout in residents also, to the extent possible, in a crisis situation such as the current pandemic (Fig. 1).
Physical exercise and dietRegular physical exercise and relaxation techniques such as mindfulness have been shown to be protective against burnout in residents. Regular exercise was the only burnout-protective activity in a study of nearly 5000 American obstetrics and gynaecology residents.32 However, several studies show that residents reduce physical activity during the training period from 60% at the beginning to 40% in the final year.30 These data are in line with the results of a sample of 2623 doctors, nurses, and residents from 5 European countries which found that insufficient exercise and increased consumption of fast food were associated with the occurrence of burnout.33Exercise and a healthy diet meet the high energy needs for proper brain function, particularly that of the prefrontal cortex. Maintaining both of these healthy habits despite the stressful work situation should be considered a priority in order to support proper functioning.4
During the pandemic, restrictions put in place by governments have limited access to gyms or the possibility of practicing sports. We did not find data on this particular aspect in our review, but it is likely that this situation limited access to a protective stress factor in residents. Finally, the consumption of alcohol and other psychoactive substances has also been linked to burnout.32,33 Those residents who consume alcohol on 4 or more occasions per week during residency have a 3.3 increased risk (odds) of developing burnout syndrome.32 Alcohol consumption, although it may initially produce a sense of stress relief, worsens brain physiology in the long term, promoting emotional distress and depression.4
Social and leisure activitiesAdequate social support, being involved in social activities and a suitable work-life balance have been reported as burnout protectors in residents22,26,30 (Fig. 1). The 'within work' activities that residents associated with relaxation were the possibility of having time to review clinical notes, talk to patients and to be able to assess articles and study. Also, having areas where they could relax (office) and having a chance to hold informal conversations or discuss patients improved the stress of the professionals. Unfortunately, there is an increasing tendency to eliminate this type of areas in the workplace.
In general, during the pandemic, institutions have prioritised the physical safety of their workers, with less emphasis on measures to support the emotional well-being. A shortage of wellness spaces at work has been reported as a risk factor for burnout in residents during this pandemic.20 These results underline the importance of implementing wellness programmes in institutions and maintaining them during times of health crisis such as formal counselling space, relaxation spaces or relaxation and meditation programmes.20 Despite the social restrictions imposed by the pandemic, residents reported in several studies that during this period they had more time to spend on study activities or pursuing a hobby at home, and this was rated positively by them21 (Table 4).
LimitationsThe literature review carried out has the limitation of not being systematic. However, it highlights the lack of consensus on the most widely used validated instrument, the MBI, due to the use of different cut-off points, different criteria for the subscales (emotional exhaustion, depersonalisation, personal accomplishment) needed to make the diagnosis and different versions of the inventory (Tables 1–3). This represents a challenge in understanding the prevalence of burnout syndrome in the resident physician population with greater accuracy. Most of the studies reviewed have a cross-sectional design and few studies have a longitudinal design that allows an analysis of incidence and risk/protective factors. In the case of resident burnout during COVID-19, a longitudinal follow-up will be of great interest in order to observe what happens throughout the different stages of the pandemic. On the other hand, the samples do not always include all specialties or study the same risk or protective factors. As all studies were conducted through on-line surveys, it was not possible to study any biological variables associated with the presence of burnout. Another limitation is the sample size and response rate of some of the surveys.
ConclusionsThe average prevalence of burnout in residents observed in the systematic reviews examined, mostly cross-sectional studies, is around 50%. Burnout syndrome seems to increase over time throughout residency in the longitudinal studies reviewed. The most commonly observed risk factors for burnout during residency were confirmed by those found in the cross-sectional studies; they were female gender (greater emotional exhaustion), male gender (greater depersonalisation), surgical specialities, making mistakes, little sleep, difficulty in reconciling family/work life and work overload. The protective factors were emotional intelligence, empathy and being able to develop a professional career.
Due to the heterogeneity of the studies, the prevalence of burnout in residents during the first wave of the COVID-19 pandemic in the cross-sectional studies reviewed was found to encompass a very wide range (26%–76%). The most important associated risk factor was the number of COVID-19 patients cared for directly by the resident. Caring for 1−30 patients almost doubled the risk and the risk quadrupled in those who cared for 60 or more patients.
The management and prevention of burnout syndrome during residency remains a pending issue, which should consider not only the psychosocial aspects of the work environment, but also the underlying biological changes in the person experiencing it. The COVID-19 pandemic has underlined the importance of being aware of this problem among professionals in training because of the enormous impact it can have both on the individual and on adequate patient care.
FundingThis work has been carried out in part thanks to the PREVENT XI grant: DN040611 (VO, RN) and the support of the Comisionado para las Universidades e Investigación DIUE of the Generalitat de Catalunya (2017/SGR/1798 [RMS]). FF has the support of Acció instrumental d'Intensificació de Professionals de la Salut-Facultatius especialistes (PERIS: SLT006/17/00014).
Conflict of interestsAll authors declare that they have no conflict of interest. The funding sources had no participation in the design, development, or publication of the study.
Please cite this article as: Navinés R, Olivé V, Fonseca F, Martín-Santos R. Estrés laboral y burnout en los médicos residentes, antes y durante la pandemia por COVID-19: una puesta al día. Med Clin (Barc). 2021;157:32–42.