The COVID-19 pandemic prompted public health measures to limit the circulation of the virus among the population. The different lockdown periods may have led to changes in drug abuse and medication use patterns, as well as in the intent of their use.
The aim of this study was to compare the characteristics of intoxications treated in a hospital Emergency Department (ED) during the different pandemic lockdown and reopening periods compared to the pre-pandemic period.
This was an observational, retrospective study of acute intoxications in the ED of a university hospital during the following pandemic phases: pre-COVID (1/1/2019-13/3/2020); lockdown (14/3/2020-21/6/2020); reopening (22/6/2020-25/10/2020), 2nd state of emergency (26/10/2020-9/5/2021) and new normal (10/5/2021-31/12/2021). Data were collected on personal details, intent and place of intoxication, toxicant involved, psychiatric and previous intoxication history, discharge destination and mortality. The epidemiological study was approved by the Ethics Committee of our centre.
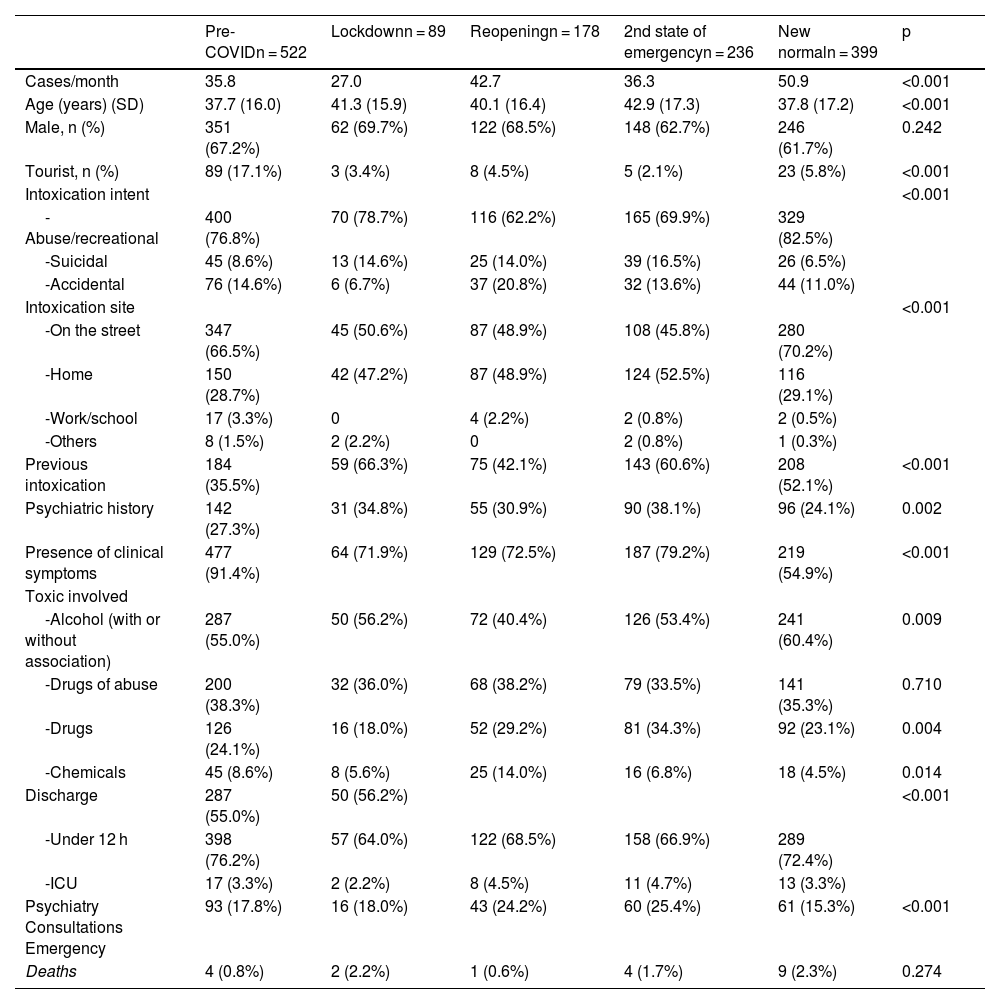
During the study period, 1,424 intoxications were treated, 522 in pre-COVID, 89 during lockdown, 178 in the reopening, 236 in the 2nd state of emergency and 399 in the new normal. During lockdown, a decrease in the number of intoxications per month was observed compared to the rest of the periods (Table 1). During the pandemic there was an increase in age (p < 0.001), predominantly males (65.2%), intoxications at home doubled, patients with previous intoxications increased (p < 0.001), as well as those with a psychiatric history (p = 0.002), and those generated in tourists decreased (p < 0.001). The main cause of intoxication in all phases was recreational, suicidal intent intoxication almost doubled and accidental intoxication decreased by half during lockdown (p < 0.001). The toxicants involved are shown in Table 1.
Description of intoxications.
| Pre-COVIDn = 522 | Lockdownn = 89 | Reopeningn = 178 | 2nd state of emergencyn = 236 | New normaln = 399 | p | |
|---|---|---|---|---|---|---|
| Cases/month | 35.8 | 27.0 | 42.7 | 36.3 | 50.9 | <0.001 |
| Age (years) (SD) | 37.7 (16.0) | 41.3 (15.9) | 40.1 (16.4) | 42.9 (17.3) | 37.8 (17.2) | <0.001 |
| Male, n (%) | 351 (67.2%) | 62 (69.7%) | 122 (68.5%) | 148 (62.7%) | 246 (61.7%) | 0.242 |
| Tourist, n (%) | 89 (17.1%) | 3 (3.4%) | 8 (4.5%) | 5 (2.1%) | 23 (5.8%) | <0.001 |
| Intoxication intent | <0.001 | |||||
| -Abuse/recreational | 400 (76.8%) | 70 (78.7%) | 116 (62.2%) | 165 (69.9%) | 329 (82.5%) | |
| -Suicidal | 45 (8.6%) | 13 (14.6%) | 25 (14.0%) | 39 (16.5%) | 26 (6.5%) | |
| -Accidental | 76 (14.6%) | 6 (6.7%) | 37 (20.8%) | 32 (13.6%) | 44 (11.0%) | |
| Intoxication site | <0.001 | |||||
| -On the street | 347 (66.5%) | 45 (50.6%) | 87 (48.9%) | 108 (45.8%) | 280 (70.2%) | |
| -Home | 150 (28.7%) | 42 (47.2%) | 87 (48.9%) | 124 (52.5%) | 116 (29.1%) | |
| -Work/school | 17 (3.3%) | 0 | 4 (2.2%) | 2 (0.8%) | 2 (0.5%) | |
| -Others | 8 (1.5%) | 2 (2.2%) | 0 | 2 (0.8%) | 1 (0.3%) | |
| Previous intoxication | 184 (35.5%) | 59 (66.3%) | 75 (42.1%) | 143 (60.6%) | 208 (52.1%) | <0.001 |
| Psychiatric history | 142 (27.3%) | 31 (34.8%) | 55 (30.9%) | 90 (38.1%) | 96 (24.1%) | 0.002 |
| Presence of clinical symptoms | 477 (91.4%) | 64 (71.9%) | 129 (72.5%) | 187 (79.2%) | 219 (54.9%) | <0.001 |
| Toxic involved | ||||||
| -Alcohol (with or without association) | 287 (55.0%) | 50 (56.2%) | 72 (40.4%) | 126 (53.4%) | 241 (60.4%) | 0.009 |
| -Drugs of abuse | 200 (38.3%) | 32 (36.0%) | 68 (38.2%) | 79 (33.5%) | 141 (35.3%) | 0.710 |
| -Drugs | 126 (24.1%) | 16 (18.0%) | 52 (29.2%) | 81 (34.3%) | 92 (23.1%) | 0.004 |
| -Chemicals | 45 (8.6%) | 8 (5.6%) | 25 (14.0%) | 16 (6.8%) | 18 (4.5%) | 0.014 |
| Discharge | 287 (55.0%) | 50 (56.2%) | <0.001 | |||
| -Under 12 h | 398 (76.2%) | 57 (64.0%) | 122 (68.5%) | 158 (66.9%) | 289 (72.4%) | |
| -ICU | 17 (3.3%) | 2 (2.2%) | 8 (4.5%) | 11 (4.7%) | 13 (3.3%) | |
| Psychiatry Consultations Emergency | 93 (17.8%) | 16 (18.0%) | 43 (24.2%) | 60 (25.4%) | 61 (15.3%) | <0.001 |
| Deaths | 4 (0.8%) | 2 (2.2%) | 1 (0.6%) | 4 (1.7%) | 9 (2.3%) | 0.274 |
SD: standard deviation; ICU: Intensive Care Unit.
Pre-COVID: from 1/1/2019 to 13/3/2020. Lockdown: from 14/3/2020 to 21/6/2020. Reopening: from 22/6/2020 to 25/10/2020. Second state of emergency from 26/10/2020 to 9/5/2021. New normal from 10/5/2021 to 31/12/2021.
During the pandemic, early discharges (less than 12 hours) decreased and intensive care unit (ICU) admissions increased (p < 0.001), with no significant difference in mortality.
This study corroborates that the COVID-19 pandemic influenced the profile of the intoxications treated, leading to changes in the epidemiology. Whereas in the lockdown periods the number of intoxications decreased, in the reopening periods there was a rebound effect.
An increase in age was observed, which may be attributed to a decrease in the number of tourists and less opportunity for festive activities by the younger age group due to lockdown. As in other studies,1 home intoxications increased.
According to other studies,2–4 suicidal intent increased during the pandemic. The economic consequences, job losses, isolation, limited mobility and therefore limited relationships with family and loved ones, deaths of friends or relatives, as well as uncertainty about the future, may have increased anxiety and depression, with suicidal ideation occurring.
The increase in intoxications with chemical products (disinfectants, cleaners) could be related to involuntary intoxications due to an increased use, or even suicidal intents.1,4 The increase in intoxications caused by drugs has been associated with their inappropriate use due to self-medication and, on occasions, medical errors.1 In our series, the most commonly involved drugs were benzodiazepines, followed by neuroleptics, while in other studies,5 over-the-counter analgesics and antidepressants were the most common.
The negative impact of the pandemic has been linked to an increase in the use of alcohol, recreational drugs and central nervous system (CNS) drugs. Recreational drug intoxications linked to social interactions were expected to decrease during lockdown, with a subsequent resurgence after de-escalation.
Due to the successive restrictions, the pandemic had an impact on mental health, especially on those with psychiatric pathologies, who were a vulnerable group during the pandemic. In our series, one third of the patients had a psychiatric history.
The main limitations of the study include the fact that it was conducted in a single ED, so the profile and characteristics of the intoxications may differ from other geographical areas.
In conclusion, the pandemic has produced changes in the profile of intoxications treated in our ED. The lockdown periods showed a decrease in the number of cases, while in the reopening periods there was an increase in the majority of cases. The development of strategies to deal with intoxication, especially alcohol or drug abuse, in future situations of lockdown or social stress, as well as preventive measures in vulnerable populations, is essential.
Ethical considerationsThe authors confirm compliance with confidentiality and respect for patients' rights.
FundingThis study has not received any funding.
Conflict of interestThe authors declare that they have no conflicts of interest.