SARS-CoV-2 coronavirus infection (Coronavirus Infectious Disease-19 [COVID-19]) has generated a situation of care overload on our health system. To address this imbalance between the clinical needs of the population and the effective availability of advanced life support (ALS) resources, we have been prompted to reflect on the ethical principles and clinical criteria that guide the decisions of health professionals when assessing patients who may require management in an intensive care unit (ICU).
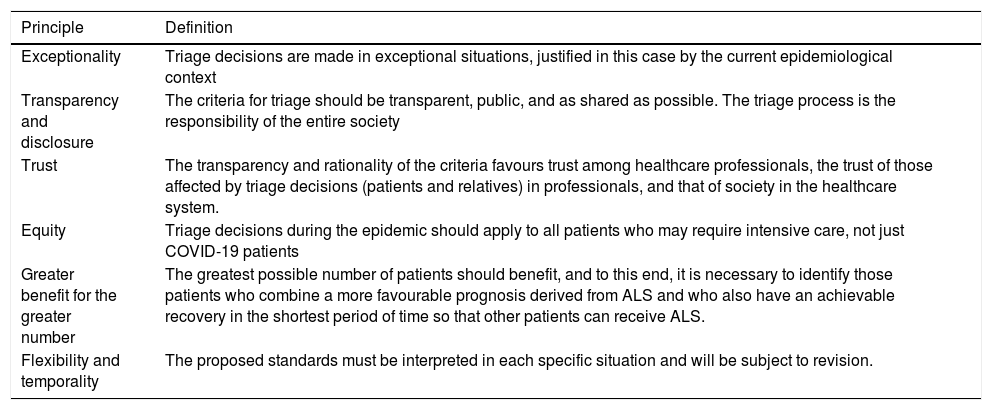
This work differs from and complements the recommendations published to date by different scientific societies, such as the Spanish Society of Intensive, Critical Medicine and Coronary Units, or by public entities such as the Spanish Bioethics Committee or the Ministry of Health itself.1–4 These consensus documents contain the general ethical principles that must guide triage protocols (Table 1). However, logically, they lack the specificity and detail that many clinicians require when making decisions in routine practice. Furthermore, some of the proposed criteria are controversial and have been criticized,5 such as the use of selection strategies by order of access to the health system,1 the prioritization of health professionals when distributing mechanical ventilation resources2 o the use of social value criteria to prioritize access to advanced life support measures.3
General ethical principles governing triage processes of advanced life support measures (adapted from ref. 5).
| Principle | Definition |
|---|---|
| Exceptionality | Triage decisions are made in exceptional situations, justified in this case by the current epidemiological context |
| Transparency and disclosure | The criteria for triage should be transparent, public, and as shared as possible. The triage process is the responsibility of the entire society |
| Trust | The transparency and rationality of the criteria favours trust among healthcare professionals, the trust of those affected by triage decisions (patients and relatives) in professionals, and that of society in the healthcare system. |
| Equity | Triage decisions during the epidemic should apply to all patients who may require intensive care, not just COVID-19 patients |
| Greater benefit for the greater number | The greatest possible number of patients should benefit, and to this end, it is necessary to identify those patients who combine a more favourable prognosis derived from ALS and who also have an achievable recovery in the shortest period of time so that other patients can receive ALS. |
| Flexibility and temporality | The proposed standards must be interpreted in each specific situation and will be subject to revision. |
ALS: advanced life support.
Our aim is different. In the current paper we not only offer general arguments to justify a triage protocol, but we describe the parties involved in the different triage decisions, their roles and the elements or criteria that can guide these decisions. Our primary intention in sharing this document is to assist clinicians in making responsible decisions about individual cases, which may not only be technically and ethically difficult, but emotionally burdensome as well. Furthermore, we wish to be both transparent and straightforward in establishing criteria for the distribution of health resources in the current circumstances of extreme shortage. Finally, we hope that these criteria can serve as a specific starting point for reflection in other centres in Spain or Latin America that still lack specific protocols, or for those to whom the general recommendations already published may be difficult to apply, because they are generic or not very effective.
The current document refers exclusively to one specific aspect of care: the process of triage of patients in relation to decision making about potential ICU admission, initiation of cardiopulmonary resuscitation (CPR) manoeuvres or ALS measures during the COVID-19 epidemic. Therefore, other decisions with important ethical implications will not be the object of this document, such as those on reverse triage (early discharge) or the adaptation or withdrawal of ALS measures in the current context.
Essential considerations in any triage protocolTriage processes assess and classify patients to determine the priority of their care and the most appropriate location for their treatment.6 In many everyday clinical situations decisions are made regarding the level of care each patient receives (home, ward, or ICU), initiation of advanced life support measures (ALS, including cardiopulmonary resuscitation [CPR], and invasive mechanical ventilation [IMV]), the withdrawal of these measures or those related to the shortage of technical means and human resources. This is also the case with public health emergencies. Although we have previous examples of catastrophes in which the use of triage protocols was necessary (11-M, earthquakes or floods, to name a few), never before has it been so essential to establish clear criteria to prioritize the admission of patients in intensive care units and access to resources such as mechanical ventilation.
Professionals require guidelines that facilitate the transition from patient-centred care, with its individual values and preferences, to population-centred health care, promoting equality among patients and equity in the wise use of available resources.7 Triage protocols seek to ensure the greatest good for the greatest number of patients through medical and ethical criteria that allow rapid and effective decision-making in circumstances that, unfortunately, force us to move away from the ideal of shared decision-making between patients and professionals. While this way of working is necessary in the current context given the serious danger to public health, its defence is only justified as a lesser evil in this context.
The public disclosure of these criteria is intended to increase objectivity, transparency and impartiality in the assessment of patients. It is important that other professionals and society know what our way of acting entails in this epidemic. This would not only foster trust between health professionals, but also try to promote trust with patients and their families. Furthermore, it is important to note that regardless of the selection criteria proposed, these should be considered flexible, interpretable in each individual clinical context and, given the significant clinical uncertainty surrounding so many areas of the current epidemic, subject to review over time.
As a starting point, it is important to note that triage decisions rest with clinicians. The responsibility of health professionals as resource managers stems from their social contract with society as a whole. This agreement establishes a certain social consent to assume an individual loss of autonomy in order to protect the access of all to limited resources, with fairness and equal opportunities.8 Thus, while it is essential to try to incorporate patient and family values into decision-making, this should not be understood to mean that the decision not to initiate CPR or IMV should depend solely on their wishes.
A subsequent reflection is that any triage protocol will not only be applicable to patients with COVID-19 but will apply to any patient needing admission to an advanced care unit for the duration of the current epidemic. It is also important to note that triage decisions are not dichotomous. To the extent possible, all possible courses of action should be considered before making a decision, including potential site transfers or the use of other types of respiratory support measures, if these may be clinically relevant (such as non-invasive mechanical ventilation or high flow oxygen therapy). It is beyond the scope of this paper to establish how information can be made available at a national level and how to regulate the potential transfer of the patient to other sites or other communities with fewer cases and ICU vacancies. Unfortunately, to date, this option has not been promoted with sufficient intensity. The number of transfers of patients between communities or ALS resources from the least affected regions to the most affected has been low. Each autonomous community has independently managed ICU beds and triage decisions. Except for the transfer of patients to the large field hospital established in IFEMA, transfers between centres within a community have been minimal and, since there are no regional criteria, each hospital has managed triage autonomously, operating like islands.5
Procedural aspects of triage protocolsPersonnel involved in triage decisionsTriage decisions must be consensual and shared among professionals. At least, it is essential that the medical team in charge and the Intensive Care or Anaesthesia/Resuscitation team, depending on the centre, are part of them. It is the responsibility of the regular medical teams to act as advocates for each patient's interests, recommending what they believe to be the best care strategy based on the overall admission objectives and patient preferences. In contrast, it is the responsibility of the Intensive Medicine, or Anaesthesia/Reanimation services, to perform the role of patient evaluators and resource managers. This decision not only derives from their expert knowledge of the management of therapies typical of intensive care medicine, but also from the fact that they are not part of the patient's routine medical team, thus being able to carry out, at least theoretically, a less subjective assessment, with more "critical distance" from the case.
The creation of decision committees (triage committees) has been suggested in some sites. The purpose of these committees would be to carry out a comprehensive evaluation of patients who are candidates for advanced life support measures considering the available resources and, furthermore, would offer the advantage of relieving the primary care team of the moral and emotional burden that these decisions imply. Analogous to transplant committees, each center would establish a committee that would operate permanently as long as triage decisions have to be made. In this way, decisions would be taken by an independent group of professionals responding to objective criteria and rationale. It has been recommended that these committees include specialists in intensive care medicine, treating doctors who care for patients with COVID-19 and by members of the care ethics committee. However, these committees may have effective operating limitations. Many of these clinical decisions are usually made outside the usual care period, during on-call or weekend shifts, when it is difficult for members to agree. Along these same lines, it is possible that the progression of certain patients makes it necessary to alter the order of priority initially proposed by the committee, transforming their evaluation into redundant.
General working method. Task delimitationThe general assessment of any patient who is a candidate for ALS or ICU admission will be carried out in two stages.
The medical team in charge would be responsible for:
- -
the initial and ongoing clinical evaluation of the patient,
- -
the examination, together with the patient and his relatives, of the patient's baseline situation, his comorbidities and the degree of impact of these on the quality of life (understood as that perceived by the patient and his family),
- -
inform and communicate diagnoses, prognosis and treatment options and
- -
perform a preliminary assessment of which patients would not be (or would not be) candidates for advanced life support measures, based on the criteria recommended in the Triage Criteria section. This assessment, carried out together with the patient and family, will serve as the basis for any possible subsequent joint assessment with the Intensive Medicine team.
The Intensive Medicine department, for its part, would carry out the clinical evaluation of serious hospitalized patients, candidates for admission to the ICU or to receive IMV, at the request of the medical team in charge. The objective of this assessment will be to prioritize certain patients among all possible candidates according to criteria of clinical suitability (Triage Criteria section). Although this assessment could be telematic, collecting severity items, in the vast majority of cases it will be in person with the medical team in charge.
Whatever the clinical decision made regarding patient access to ALS measures or a patient's CPR manoeuvres, this should be clearly documented in their medical history. Likewise, it is necessary to exercise extreme clarity, professionalism and tact in the communication of decisions made with the rest of the health team (nursing and nurse's aides), as well as with the patient and his family.
In summary, the work of both teams is complementary. While the medical team in charge should identify those patients who are not candidates for advanced life support measures or CPR, the work of the Intensive Medicine team, or the triage committee, would be to identify among the possible candidates those with the most options to survive admission to the ICU. It should not be considered the task of routine medical teams, nor would it be clinically or ethically appropriate to discourage the use of advanced life support measures or CPR in patients who can be considered candidates under the proposed criteria without at least a joint assessment with the ICU team. Similarly, the presence of these criteria in no way prevents a professional, in case of a clinical doubt, from consulting any patient regardless of age, baseline or comorbidities.
It is important to note that decisions made about the provision of CPR manoeuvres or about access to IMV should not exclude a patient's access to other diagnostic or therapeutic procedures that may be indicated, such as performing interventional radiology techniques in patients with stroke, emergent coronary intervention, a possible surgical intervention, or any other therapeutic measure (such as treatment with monoclonal antibodies or metabolic pathway inhibitors). Nor should these decisions interfere with the energetic provision of care and treatment for the control of symptoms that any patient may have.
Specifically, in relation to the care of cardiac patients, a population at special risk of SARS-CoV-2 infection, it is important to make special mention of the treatment of ventricular arrhythmias, especially peri-infarction or peri-angioplasty. Cardiac arrest in the context of acute coronary ischemia usually corresponds mainly to shockable rhythm PCR (ventricular fibrillation or pulseless ventricular tachycardia) and does not carry the same prognosis as other causes of cardiac arrest (pneumonia, infections, for example). In this context, it may be indicated to initiate advanced CPR manoeuvres with early defibrillation, even in the event that the patient may not subsequently be a candidate for IMV, since these manoeuvres, even if brief, can be effective.
Triage criteriaOur working group has opted for a triage strategy that prioritizes two essential factors: optimizing options for therapeutic success and maximizing the number of patients with access to the IMV resource.6,9 These criteria translate into the identification and selection of "clinically suitable" patients; that is, those that combine a more favourable prognosis with greater possibilities of benefit derived from the treatment. In other words, those patients who have a greater chance of survival and of achieving this, a priori, in the shortest period of time with an ICU admission.10 Although the criteria have been established to initially prioritize access to IMV, these may also be valid in decisions to rationalize other scarce resources (other modalities of advanced life support or treatment with monoclonal antibodies, for example).
The proposed clinical criteria are based on a clinical evaluation and the use of prognosis scores:
- -
Short-term prognosis estimation: Despite the potential limitations of any risk score, the working group has chosen APACHE-II as a decision support tool.11 The SOFA index has also been widely used in this context. In the use of any of these tools, not only its initial score is relevant, but also changes over time. Since its predictive value for mortality is limited, in no case will the score on these scales be used as the sole criterion for treatment access exclusion.12
- -
Long-term prognosis estimation: For this, the medical team has, among others, the assessment of the baseline situation of the patients and information on the number and severity of the associated comorbidities.
- •
The baseline situation will be evaluated through a functional and cognitive assessment of the patients. The first will be assessed according to the level of independence in baseline activities of daily living (Barthel index) and in instrumental activities. The patient's baseline cognitive situation will be evaluated with the usual tools validated for this purpose (Pfeiffer's test, for example). To avoid discrimination against groups with disabilities, it is important not only to consider the presence of functional or cognitive-intellectual dependency, but also its potential progression over time (stable disability processes, such as congenital intellectual disability, compared to processes that involve increasing disability in the future in the short-medium term, such as neurodegenerative processes with progressive cognitive decline).
- •
To assess comorbidities, we propose a categorization based on an adaptation of the criteria proposed by White et al.13:
- ◦
Absence of comorbidities.
- ◦
Comorbidities with little impact on the long-term prognosis and that are not expected to condition the short-term progression of a possible ICU admission (for example, benign prostatic hypertrophy, dyslipidaemia).
- ◦
Comorbidities that affect long-term survival or that could complicate the progression of a possible ICU admission (obesity, stable and revascularized ischemic heart disease, chronic kidney disease, COPD).
- ◦
Comorbidities that substantially affect long-term survival (estimated survival < 2 years).
- ◦
- •
Age: The working group initially established a tentative and revisable cut-off point of 80 years of age to unilaterally limit access to advanced life support measures. This non-unanimous decision, is ethically controversial and has subsequently been criticized.2 Age undoubtedly relates directly to the potential life expectancy and should be incorporated as a relevant variable in the decision-making process. The inclusion of age in decision-making is not intended to reflect value judgments on quality of life or the value of life of older patients, but we do recognize that, in cases of severe viral pneumonia, the consequences of prolonged artificial ventilation required by this disease are difficult to overcome in situations of clinical frailty or old age. In these circumstances, treatment can lead to situations of therapeutic obstinacy, aggravated by the loss of opportunity to use the artificial ventilation resource for other patients with a greater probability of survival and, secondarily, more years of life saved in a situation of serious disproportion of need and availability of resources.
Finally, it may be the case that the clinical conditions of two or more patients are reasonably equal (similar clinical suitability condition), competing for an IMV resource. In order to make a decision at this stage, a new joint assessment of the different cases will be necessary between the Intensive Care Medicine teams and the medical teams in charge. In it, the clinical data on the progression from admission, the prediction of the expected time of use for the specific resource, the consideration of possible transfers and/or the possible use of bridging therapies (NIV or high-flow oxygen) will be particularly relevant. The working group considers that the use of a «first come, first served» policy (allocation of the resource to the patient who has been waiting the longest) should not be used, except as a last resort.9
Limitations of this paperThe article offers the perspective prepared by a multidisciplinary team of specialists from a single tertiary hospital in the community of Madrid. Thus, the process of preparing this protocol, like so many others at national or international level, has not been structured. The proposal made does not follow a strict qualitative methodology in its development, but rather part of a narrative review of the literature on triage in pandemic situations to adapt the general recommendations to the local idiosyncrasy of our site. Although this could limit the generalization of its conclusions, there are two aspects that suggest that our proposal may be implemented in other clinical contexts. First, the Autonomous Community of Madrid (ACM) has been the region with the most cases of COVID-19 and the first where saturation of hospital and, in particular, ICUs, was reached. This experience has been reasonably homogeneous and shared by all the major hospitals in the region, as several of the authors have been able to verify. In this sense, DRA, as a participant in the working group that has elaborated the ACM general guidelines for hospital triage, has had the opportunity to review multiple protocols and regional triage proposals. These are, in essence, compatible with the proposal presented here.
Second, current reflections seem to focus solely on decisions about the provision of CPR manoeuvres or ventilatory support. Although it is true that critically ill patients may require other types of ALS, such as renal replacement therapies, with the current data on the epidemic, it does not seem that there is currently saturation in these resources, or, at least, not to the degree experienced by IMV. In any case, the current reflections can also be applied to decisions about other ALS modalities or specific treatment that may be considered a scarce resource at some point, as might occur with monoclonal anti-IL-6 antibodies.
ConclusionsThe COVID19 pandemic has overstretched our healthcare system and tested routine clinical decision-making mechanisms. This document proposes a specific protocol that, incorporating the general recommendations of different institutions, identifies the parties involved in the different triage decisions, the roles of these parties and the elements or criteria that can guide these decisions. Our intention is to encourage critical debate among professionals and facilitate the establishment of protocols in other hospitals that will help in the transition from patient-centred care, with its individual values and preferences, to care focused on the health of the population, minimising its morbidity and mortality through the sensible use of available resources.
Authorship and participationConception and design of the manuscript: DRA, JMG, JI, JF
Data Collection: Not applicable
Analysis and interpretation of data: Not applicable
Drafting, revision, approval of the submitted manuscript: DRA, JMG, DR, PA, JI, RM, TA, MC, JS, BR, FC, IG, AC, JF
FundingThe present research has not received a specific grant from public, commercial, or non-profit agencies.
Conflict of interestsThe authors declare no conflict of interest.
The authors wish to thank the comments and suggestions of different members of the Healthcare Ethics Committee of the University Hospital of La Princesa who have participated in the process of creating the document. The current manuscript is not a direct transcript of the hospital's action protocol but has been edited to suit editorial requirements.
Please cite this article as: Real de Asúa D, Galván JM, Iglesias J, Fernández J. Criterios de triaje para reanimación cardiopulmonar y soporte vital avanzado durante la epidemia COVID-19. Med Clin (Barc). 2020;155:215–219.