Post-intensive care syndrome comprises certain complications in all spheres of life after discharge from the intensive care unit (ICU). In the physical sphere, the high incidence of chronic musculoskeletal pain stands out. Shoulder pain is common (5–80%) and can persist for six to 12 months after discharge from hospital, affecting the functionality of the limb and incurring high costs (work incapacity, low productivity, health care costs, etc.)1,2.
Our objective was to quantify the presence of shoulder pain two months after hospital discharge in patients admitted to the ICU due to COVID-19 pneumonia who needed rehabilitation during their stay, and to study its relationship with patient-dependent factors, treatments received, their ICU and hospital progression.
A prospective cohort study was conducted between March and June 2020 of patients admitted to the ICU of the Toledo Hospital Complex as a consequence of COVID-19 pneumonia and who were assessed and treated during their admission by the rehabilitation department due to ICU-acquired weakness. This department conducted a follow-up during two months after discharge. Variables related to personal characteristics and days of admission to the ICU and to the hospital were collected. Severity scores, corticosteroids use, prolonged prone positioning and mechanical ventilation were collected during the ICU stay. The presence of shoulder pain and the functionality of the upper limb were assessed at the medical consultation (self-completed questionnaire disabilities of the arm, shoulder, and hand score [QuickDASH]).
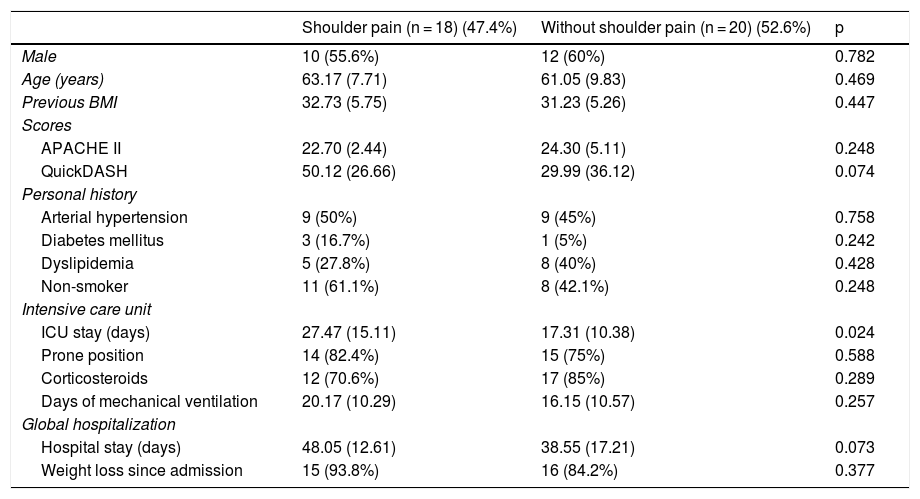
During this period, 120 patients were admitted to the ICU and 62 (51.6%) were discharged from hospital. Forty-one people were evaluated for rehabilitation during admission and 38 were underwent follow-up after hospital discharge, 24 of whom were men (58.5%), with a mean age of 62.6 (8.8) years. All of them were sedated on mechanical ventilation, with a duration of 17.8 (10.35) days. Twenty-nine patients (76.3%) were in prone position and corticosteroids were used in 76.3% of them. The acute physiology and chronic health evaluation (APACHE II) was 23.6 (4.1). Three cases had previous shoulder pain and all worsened after admission. Two months after hospital discharge, 18 people (47.4%) had shoulder pain and the QuickDASH was 39.19 (33.28). Table 1 shows the comparison of the variables according to whether or not the patient had shoulder pain.
Comparison of patients studied, according to whether or not they have shoulder pain.
| Shoulder pain (n = 18) (47.4%) | Without shoulder pain (n = 20) (52.6%) | p | |
|---|---|---|---|
| Male | 10 (55.6%) | 12 (60%) | 0.782 |
| Age (years) | 63.17 (7.71) | 61.05 (9.83) | 0.469 |
| Previous BMI | 32.73 (5.75) | 31.23 (5.26) | 0.447 |
| Scores | |||
| APACHE II | 22.70 (2.44) | 24.30 (5.11) | 0.248 |
| QuickDASH | 50.12 (26.66) | 29.99 (36.12) | 0.074 |
| Personal history | |||
| Arterial hypertension | 9 (50%) | 9 (45%) | 0.758 |
| Diabetes mellitus | 3 (16.7%) | 1 (5%) | 0.242 |
| Dyslipidemia | 5 (27.8%) | 8 (40%) | 0.428 |
| Non-smoker | 11 (61.1%) | 8 (42.1%) | 0.248 |
| Intensive care unit | |||
| ICU stay (days) | 27.47 (15.11) | 17.31 (10.38) | 0.024 |
| Prone position | 14 (82.4%) | 15 (75%) | 0.588 |
| Corticosteroids | 12 (70.6%) | 17 (85%) | 0.289 |
| Days of mechanical ventilation | 20.17 (10.29) | 16.15 (10.57) | 0.257 |
| Global hospitalization | |||
| Hospital stay (days) | 48.05 (12.61) | 38.55 (17.21) | 0.073 |
| Weight loss since admission | 15 (93.8%) | 16 (84.2%) | 0.377 |
APACHE II: acute physiology and chronic health evaluation; BMI: body mass index; QuickDASH: disabilities of the arm, shoulder, and hand score; ICU: intensive care unit.
Quantitative variables are shown as mean (standard deviation) and categorical variables as counts (percentage). Statistical significance is assumed when p < 0.05.
The literature on shoulder pain in patients admitted to the ICU is limited and scarce if the cause is COVID-19 pneumonia3. The factors associated with the presence of shoulder pain after admission to the ICU are age, previous pain and medical comorbidities4. Many of these aspects could be risk factors for the admission of COVID-19 patients.
The factors related to chronic pain one year after hospital discharge are age, severity of disease, prolonged opioid use, mechanical ventilation for more than 12 days, or an ICU stay longer than 15 days1,5. We have not observed any relationship between shoulder pain at two months after hospital discharge with APACHE II score, or with the days of treatment with mechanical ventilation, although there is a statistically significant association with the days of admission to the ICU and a trend only in the overall hospital stay. This could be partially explained by joint immobilization and secondary muscle wasting. One of the strategies for its prevention and treatment is early mobilization, which is why rehabilitation services play a major role.
Prolonged prone positioning is used in patients on mechanical ventilation to improve oxygenation in COVID-19 pneumonia. Prolonged prone positioning seems to increase subacromial compression compared to supine position, however, we have not found studies that link it with shoulder pain when its use is prolonged. Although we have not been able to demonstrate this relationship either, it is important to remember the need for proper patient positioning to reduce potential adverse effects.
Our conclusion is based on the high presence of shoulder pain in patients admitted to the ICU due to COVID-19 pneumonia, having a statistically significant relationship with the stay in the ICU. We found no association with previous comorbidities or ICU treatment in relation to shoulder pain.
Conflict of interestsThe authors declare no conflict of interest.
Please cite this article as: Puentes-Gutiérrez AB, Sánchez-Casado M, Díaz-Jiménez M. Dolor de hombro como lesión residual tras el alta hospitalaria en pacientes ingresados en UCI por neumonía COVID-19. Med Clin (Barc). 2021;156:301–302.