The aim of this study was to assess the psychological impact among healthcare workers who stand in the frontline of the SARS-CoV-2 crisis and to compare it with the rest of healthcare professionals, by means of a systematic review of Western publications. The systematic review was carried out in PubMed, Scopus and Web of Science databases and 12 descriptive studies were reviewed. The European and American quantitative studies reported moderate and high levels of stress, anxiety, depression, sleep disturbance and burnout, with diverse coping strategies and more frequent and intense symptoms among women and nurses, without conclusive results by age. In the first line of assistance the psychological impact was greater than in the rest of the health professionals and in the Asian area. It is necessary to go deeper into the emotional experiences and professional needs for emotional support in order to design effective interventions for protection and help.
El objetivo de este estudio fue conocer el impacto psicológico entre el personal sanitario de primera línea en la asistencia a pacientes con SARS-CoV-2 y compararlo con el resto de profesionales sanitarios, a través de una revisión sistemática de la producción científica en el ámbito occidental. La revisión se realizó en las bases PubMed, Scopus y Web of Science y se seleccionaron 12 artículos. Los estudios cuantitativos realizados en Europa y EE. UU. refirieron niveles moderados y altos de estrés, ansiedad, depresión, alteración del sueño y burnout, con estrategias de afrontamiento diversas y síntomas más frecuentes e intensos entre mujeres y enfermería, sin resultados concluyentes por edad. En la primera línea de asistencia, el impacto fue mayor que en el resto de profesionales sanitarios y que en el ámbito asiático. Se requiere profundizar en las experiencias emocionales y necesidades profesionales de apoyo emocional, para diseñar intervenciones eficaces de protección y ayuda.
The declaration of the pandemic in March 20201 and the confinement measures imposed by the SARS-CoV-2 outbreak generated an unprecedented public health situation, with consequences for the mental health of the general population2 and especially that of health personnel, according to studies carried out mainly in China and other Asian countries3–12. Although there are various systematic reviews that reflect the increase in the prevalence of stress, anxiety, depression, insomnia, or burnout among healthcare professionals during the current pandemic13–17, there are only a few studies that focus on professional well-being during the pandemic, with priority having been given to the epidemiological aspects of the disease18.
During the SARS-CoV-1 (2003)19–23, H1N1 (2009)24,25, MERS-CoV (2012)26,27 and Ebola (2014)28,29 outbreaks the impact on healthcare personnel’s mental health was documented. Moderate and high levels of anxiety24,27, depression, post-traumatic stress20 and absenteeism27,29 were observed, with higher prevalence among nursing professionals, younger individuals19,22,23 and those with direct contact with infected patients22,30,31.
In the current COVID-19 crisis, the frontline healthcare workers, especially those in the Emergency Services, Intensive Care Units (ICU) and the Pulmonology departments, were particularly susceptible to developing psychiatric disorders4,32. Despite a social and professional identity based on experience and preparation to cope with intense emotional and cognitive demands33 – resilient personality or hardiness34 –, a lack of knowledge, preparedness9 and stable protocols of action32 can lead to demotivation and mental health problems5, such as a higher levels of stress3,6, anxiety or depression35. Other authors associated the greatest psychological impact among the “soldiers on the frontline”14 to working conditions (use of personal protective equipment, reorganisation of the workspace, management of the lack of material resources and workload, extra shifts, and longer hours), social and family aspects (social distancing, fear of infecting loved ones) and factors related to patients (high mortality rate, contact with suffering, death and ethical dilemmas)15.
In Asia, studies carried out exclusively with frontline health personnel36–39 or compared with other health professionals3,4, indicated the need to promote the psychological well-being of the professionals. However, it is unknown whether support plans and measures implemented in other geographical and cultural settings would be applicable here. This means there is an urgent need to explore the psychological effects of COVID-19 in the Western world, and to understand the associated risks and possible protection factors. Then, optimal and efficient strategies to support and help mental health can be designed.
Therefore, the objective of this study was to identify the psychological impact among frontline healthcare personnel when caring for SARS-CoV-2 patients and to compare it with the rest of healthcare professionals, through a systematic review of the scientific production in the Western world.
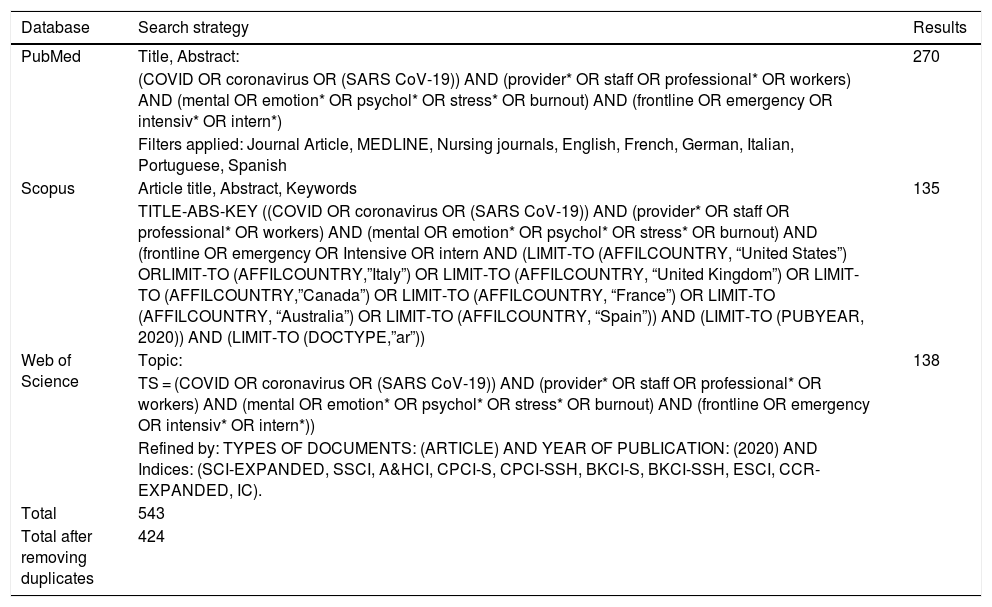
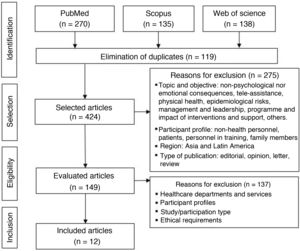
MethodsA systematic review of the bibliography available in the PubMed, Scopus and Web of Science databases was carried out. The search terms used were organised around four elements: 1. Context, epidemiological situation of the SARS CoV-19 pandemic (terms used: COVID, coronavirus, SARS CoV-19); 2. Agents, health personnel who treated patients with COVID (terms used: provider, personnel, professional, workers); 3. Results, impact and consequences on mental and emotional health (terms used: mental, emotion, psychol*, stress, burnout); and 4. Scope, services and units that offered frontline healthcare (frontline, emergency, intensiv*, internal*). For each block, the indexed terms were located in Medical Subject Heading (MeSH) and Health Science Descriptors (DeCS), which were combined with free designation terms.
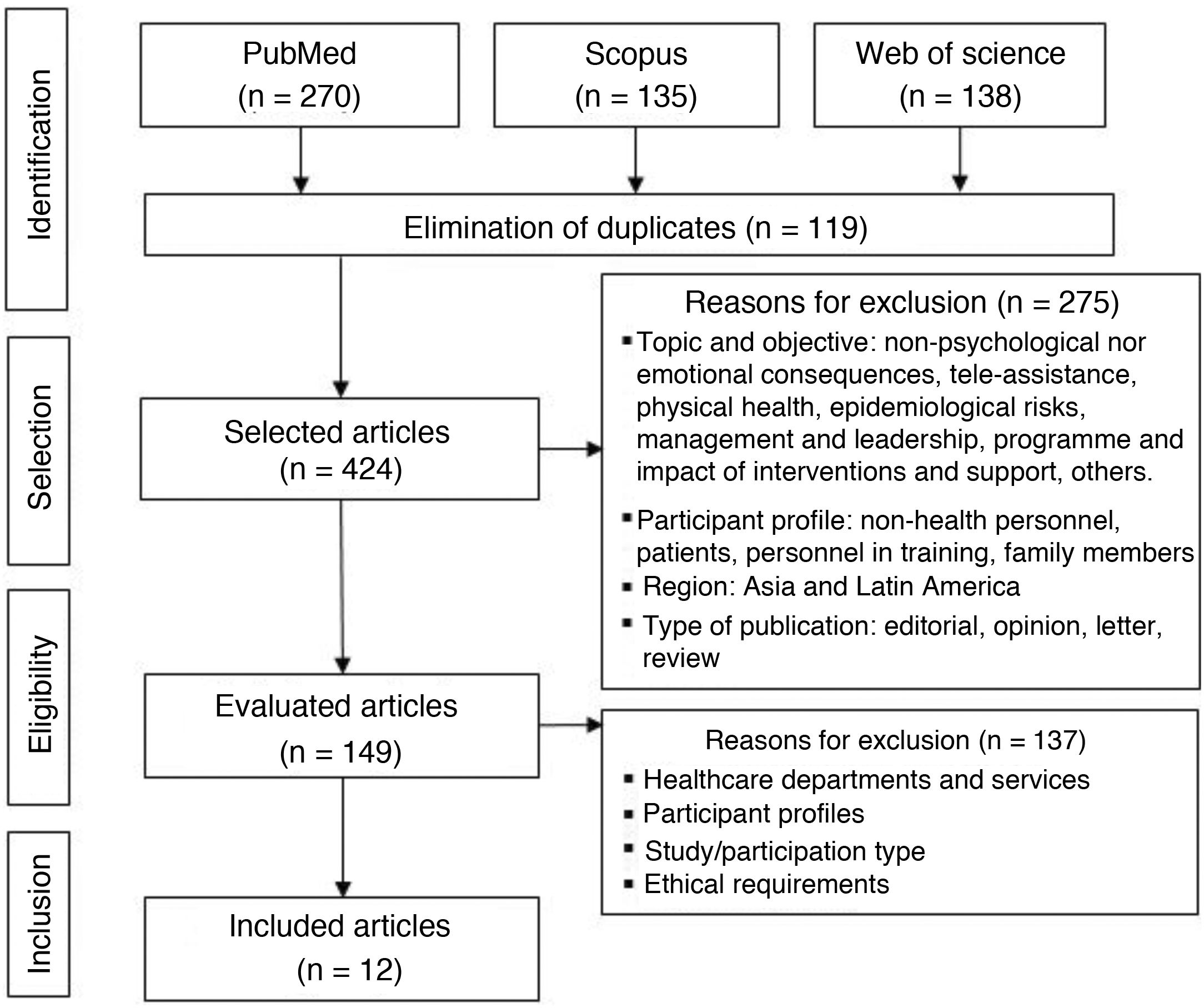
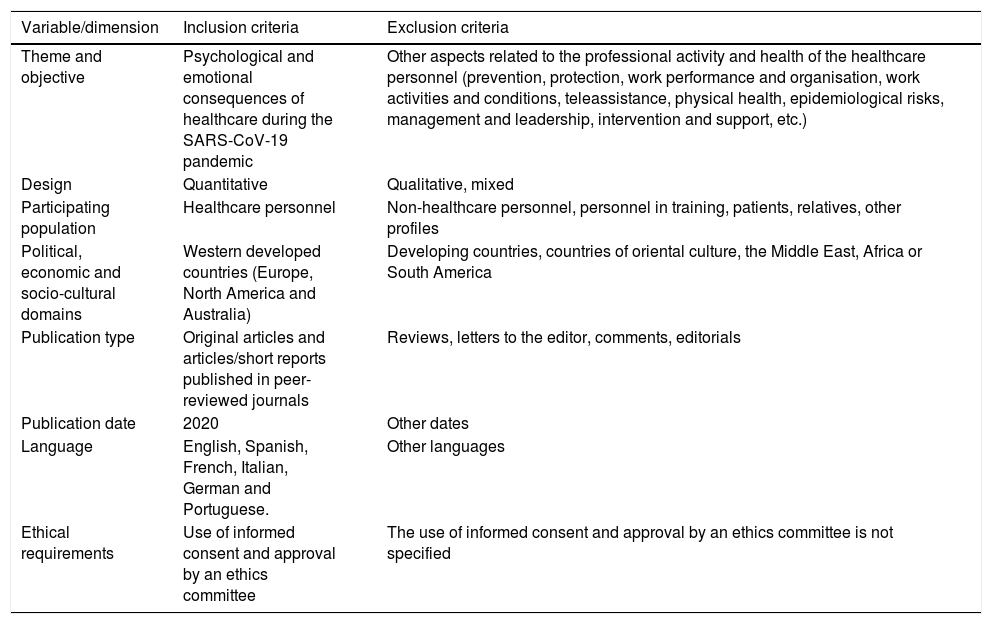
The search was carried out on 5th and 6th August 2020 and included all the publications available since the start of the pandemic. Table 1 shows the strategies and terms used for each database, as well as the results obtained. Once the articles had been identified and duplicates eliminated, a process of (pre)selection, selection and analysis was carried out in four phases (Fig. 1), following the Prisma guidelines40. In the selection process, the inclusion and exclusion criteria described in Table 2 were used.
Search strategy, terms and descriptors used.
| Database | Search strategy | Results |
|---|---|---|
| PubMed | Title, Abstract: | 270 |
| (COVID OR coronavirus OR (SARS CoV-19)) AND (provider* OR staff OR professional* OR workers) AND (mental OR emotion* OR psychol* OR stress* OR burnout) AND (frontline OR emergency OR intensiv* OR intern*) | ||
| Filters applied: Journal Article, MEDLINE, Nursing journals, English, French, German, Italian, Portuguese, Spanish | ||
| Scopus | Article title, Abstract, Keywords | 135 |
| TITLE-ABS-KEY ((COVID OR coronavirus OR (SARS CoV-19)) AND (provider* OR staff OR professional* OR workers) AND (mental OR emotion* OR psychol* OR stress* OR burnout) AND (frontline OR emergency OR Intensive OR intern AND (LIMIT-TO (AFFILCOUNTRY, “United States”) ORLIMIT-TO (AFFILCOUNTRY,”Italy”) OR LIMIT-TO (AFFILCOUNTRY, “United Kingdom”) OR LIMIT-TO (AFFILCOUNTRY,”Canada”) OR LIMIT-TO (AFFILCOUNTRY, “France”) OR LIMIT-TO (AFFILCOUNTRY, “Australia”) OR LIMIT-TO (AFFILCOUNTRY, “Spain”)) AND (LIMIT-TO (PUBYEAR, 2020)) AND (LIMIT-TO (DOCTYPE,”ar”)) | ||
| Web of Science | Topic: | 138 |
| TS = (COVID OR coronavirus OR (SARS CoV-19)) AND (provider* OR staff OR professional* OR workers) AND (mental OR emotion* OR psychol* OR stress* OR burnout) AND (frontline OR emergency OR intensiv* OR intern*)) | ||
| Refined by: TYPES OF DOCUMENTS: (ARTICLE) AND YEAR OF PUBLICATION: (2020) AND Indices: (SCI-EXPANDED, SSCI, A&HCI, CPCI-S, CPCI-SSH, BKCI-S, BKCI-SSH, ESCI, CCR-EXPANDED, IC). | ||
| Total | 543 | |
| Total after removing duplicates | 424 |
Flow diagram of the bibliographic selection process. Own elaboration based on the Prisma guidelines51.
Inclusion and exclusion criteria.
| Variable/dimension | Inclusion criteria | Exclusion criteria |
|---|---|---|
| Theme and objective | Psychological and emotional consequences of healthcare during the SARS-CoV-19 pandemic | Other aspects related to the professional activity and health of the healthcare personnel (prevention, protection, work performance and organisation, work activities and conditions, teleassistance, physical health, epidemiological risks, management and leadership, intervention and support, etc.) |
| Design | Quantitative | Qualitative, mixed |
| Participating population | Healthcare personnel | Non-healthcare personnel, personnel in training, patients, relatives, other profiles |
| Political, economic and socio-cultural domains | Western developed countries (Europe, North America and Australia) | Developing countries, countries of oriental culture, the Middle East, Africa or South America |
| Publication type | Original articles and articles/short reports published in peer-reviewed journals | Reviews, letters to the editor, comments, editorials |
| Publication date | 2020 | Other dates |
| Language | English, Spanish, French, Italian, German and Portuguese. | Other languages |
| Ethical requirements | Use of informed consent and approval by an ethics committee | The use of informed consent and approval by an ethics committee is not specified |
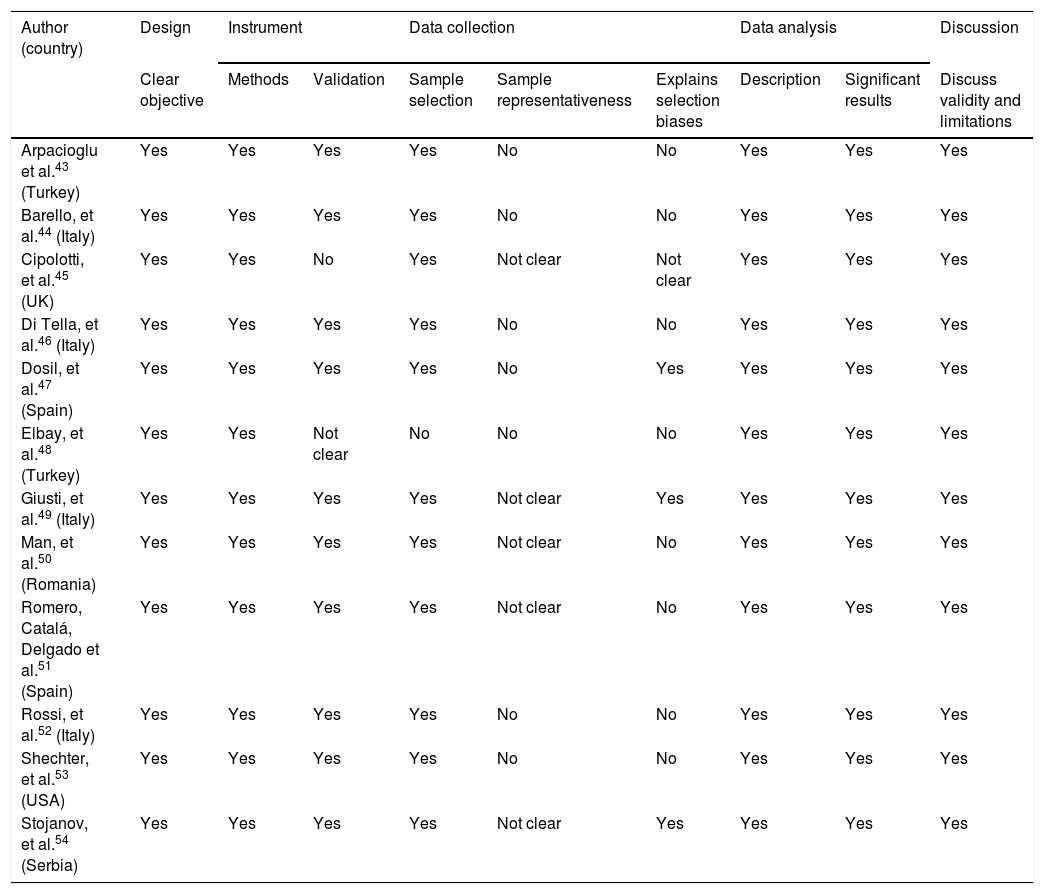
The 12 selected articles were reviewed, and data was extracted regarding: setting/country, objectives, methodology (design, participants, and instruments) and main results. The evaluation of the methodological quality was based on the good practices standard criteria for questionnaire-based, cross-sectional, quantitative studies41. Table 3 includes the checklist of PRISMA 40 and AMSTAR-242 items for the critical appraisal of the systematic review.
PRISMA and AMSTAR-2 items checklist for critical evaluation of the systematic review.
| Items PRISMA (2009) | |
|---|---|
| Title. Identify the publication as a systematic review, meta-analysis, or both | Yes |
| Structured summary | Yes |
| Introduction. Justification | Yes |
| Introduction. Objectives | Yes |
| Methods. Protocol and registration | Yes, partial (no registration) |
| Methods. Eligibility criteria | Yes |
| Methods. Information sources | Yes |
| Methods. Search | Yes |
| Methods. Study selection | Yes |
| Methods. Data collection process | Yes, partial |
| Methods. Data list | Yes |
| Methods. Risk of bias in the individual studies | Yes |
| Methods. Summary measures | Yes |
| Methods. Synthesis of results | Yes |
| Methods. Risk of bias between studies | No |
| Methods. Additional analysis | No |
| Results. Study selection | Yes |
| Results. Study characteristics | Yes |
| Results. Risk of bias in the studies | Yes |
| Results of the individual studies | Yes |
| Removed. Synthesis of results | Yes |
| Results. Risk of bias between studies | No |
| Results. Additional analysis | No |
| Discussion. Summary of the evidence | Yes |
| Discussion. Limitations | Yes |
| Discussion. Conclusions | Yes |
| Funding | Yes |
| AMSTAR-2 (2017) criteria | |
| Do the research questions and inclusion criteria for the review include PICO components? | Yes |
| Does the review report contain an explicit statement that the review methods were established prior to the review and justify any significant deviations from the protocol? | Yes, partial (no registration) |
| Do the review authors explain their decision about the study designs to include in the review? | Yes |
| Do the authors use a comprehensive bibliography search strategy? | Yes |
| Do the authors duplicate the selection of studies? | No |
| Do the authors duplicate data extraction? | No |
| Do the authors provide a list of excluded studies and justify the exclusions? | Yes, partial |
| Do the authors describe the included studies in sufficient detail? | Yes |
| Do the authors use a satisfactory technique to assess the risk of bias of the individual studies (for non-randomised intervention studies)? | Yes, partial |
| Do the authors report the sources of funding for the studies included in the review? | No (not available) |
| If a meta-analysis was performed, do the authors use appropriate methods for the statistical combination of results? | No meta-analysis |
| If a meta-analysis was performed, do the authors assess the potential impact of risk of bias in the individual studies on the results of the meta-analysis? | No meta-analysis |
| Do the authors consider the risk of bias of the individual studies when interpreting/discussing the results of the review? | Yes |
| Do the authors provide a satisfactory explanation and discuss any observed heterogeneity in the results of the review? | Yes |
| If a quantitative synthesis was performed, do the authors conduct an adequate investigation of publication bias and discuss its likely impact on the results of the review? | No meta-analysis |
| Do the authors report any potential conflict of interest, including any funding received to carry out the review? | Yes |
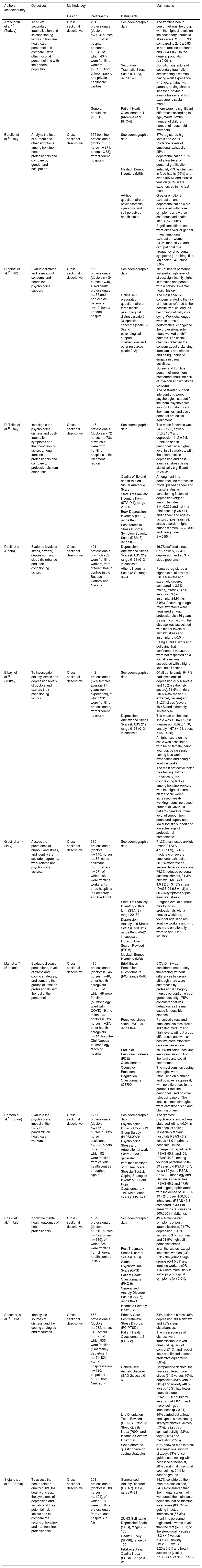
The 12 articles reviewed43–54 were based on cross-sectional descriptive studies conducted in Italy44,46,49,52, Spain47,51, Turkey43,48, UK45, Romania50, Serbia54 and USA53, with quantitative methodology and study populations made up of frontline and other health professionals, except for one study with only frontline health personnel44.
Non-probability convenience sampling was used in the participant selection process and samples varying from 115 professionals50 to 1671 professionals51 were generated, within which the percentage of participants who were frontline carers for SARS-CoV-2 patients ranged from 42%50 to 82%53. In one of the studies, no information was provided regarding direct assistance to COVID-19 patients by the respondents45. The description of the samples was carried out jointly, with no discrimination regarding specific sociodemographic characteristics of the frontline personnel, except in one study53.
The main variables -stress, depression, anxiety, sleep disturbances and burnout- were measured with the following specific instruments: Depression, Anxiety and Stress Scale (DASS 21), Generalized Anxiety Disorder Scale (GAD), State-Trait Anxiety Inventory (STAI), Insomnia Severity Index (ISI), Pittsburg Sleep Quality Index (PSQI) and Maslach Burnout Inventory (MBI). Aspects related to health and perception of COVID-19 were measured with: Patient Health Questionnaire (PHQ), SF-36 Health Questionnaire and Illness Perception Questionnaire (IPQ). Data on coping strategies and support measures were also collected, through our own made-up instruments and the Cognitive Emotional Regulation Questionnaire (CERQ).
Table 4 contains the information synthesised from the analysis of the selected sources.
Description and results of the studies included in the review.
| Authors (scope/country) | Objectives | Methodology | Main results | ||
|---|---|---|---|---|---|
| Design | Participants | Instruments | |||
| Arpacioglu et al.43 (Turkey) | To study secondary traumatization and its conditioning factors in frontline healthcare personnel and compare it with other hospital personnel and with the general population. | Cross-sectional descriptive | 251 professionals (doctors n = 124; nurses n = 93, other hospital personnel n = 34), of which 43% were frontline workers (n = 109) from different public and private healthcare centres | Sociodemographic data | The frontline health personnel was the group with the highest levels on the secondary traumatic stress scale: 2.66 ± 0.93 compared to 2.46 ± 0.83 in non-frontline personnel and 2.34 ± 0.76 in the general population (p< 0.001). |
| Secondary Traumatic Stress Scale (STSS), range 1–5 | Conditioning factors of secondary traumatic stress: being a woman, having work experience < 10 years, living with parents, having chronic illnesses, having a trauma history and high exposure to social media. | ||||
| General population (n = 312) | Patient Health Questionnaire-4 (Kroenke et al. PHQ-4) | There were no significant differences according to age, marital status, number of children, number of household members. | |||
| Barello, et al.44 (Italy) | Analyze the level of burnout and other symptoms among frontline health professionals and compare by gender and occupation. | Cross-sectional descriptive | 376 frontline professionals (doctor n = 67, nurse n = 271, others n = 38), from different hospitals | Sociodemographic data | 37% registered high levels and 22.9% moderate levels of emotional exhaustion, 25% of depersonalization. 15% had a low level of personal gratification. |
| Maslach Burnout Inventory (MBI) | Irritability (59%), changes in food habits (56%) and sleep (55%), and muscle tension (48%) were experienced in the last month. | ||||
| Ad-hoc questionnaire of psychosomatic symptoms and self-perceived health status | Greater emotional exhaustion and depersonalization were associated with more symptoms and worse self-perceived health status (p < 0.001). | ||||
| Significant differences were observed for gender (mean emotional exhaustion: women 24.05, men 18.74) and occupational role (frequency of personal symptoms (1-nothing; 5- a lot) doctor 2.47, nurse 3.05). | |||||
| Cipolotti et al.45 (UK) | Evaluate distress and learn about concerns and needs for psychological support. | Cross-sectional descriptive | 158 professionals (doctors n = 34, nurses n = 45, allied health professionals n = 35 and non-clinical personnel n = 44) from a London hospital | Sociodemographic data | 78% of health personnel suffered a high level of stress, significantly higher in females and people with a previous mental health history. |
| Online self-elaborated questionnaire of three blocks: psychological distress (scale 0–3), specific concerns (scale 0–3) and psychological support interventions and other resources (scale 0–2) | The main specific concern related to the risk of infection referred to the possibility of colleagues becoming critically ill or dying. Work challenges were in terms of performance, changes to the professional role, hours worked or shift patterns. The social changes reflected the concern about distancing from family and friends and being unable to engage in usual activities. | ||||
| Nurses and frontline personnel were more concerned about the risk of infection and workforce concerns. | |||||
| The best-rated support interventions were: psychological support for the team, psychological support for patients and their families, and use of personal protective equipment. | |||||
| Di Tella, et al.46 (Italy) | Investigate the psychological distress and post-traumatic symptoms and their conditioning factors among frontline professionals and compare to professionals from other units | Cross-sectional descriptive | 145 professionals (doctors n = 72, nurses n = 73), of which 63 were from frontline hospitals in the Piedmont region | Sociodemographic data | The mean for stress was 24.7 ± 17.1, anxiety 51.3 ± 13.9 and depression 11.5 ± 9.5. Frontline health personnel had a higher level in all variables, with the differences in depression and post-traumatic stress being statistically significant (p < 0.05). |
| Quality of life and health-related Visual Analogue Scale | Among front-line personnel, the regression model placed gender and marital status as conditioning factors of depression (higher among females β = −0,252 and not in a relationship β = 0.441) and gender and age as factors of post-traumatic stress disorder (higher among women β = −0.398 and being older β = 0.554). | ||||
| State-Trait Anxiety Inventory Form (STAI Y1), range 20–80 | |||||
| Beck Depression Inventory (BDI-II), range 0–63 | |||||
| Post-traumatic Stress Disorder Symptom Severity Scale (DSM-5), range 0–80 | |||||
| Dosil, et al.47 (Spain) | Evaluate levels of stress, anxiety, depression, and sleep disturbance and their conditioning factors | Cross-sectional descriptive | 421 professionals, of which 292 were frontline workers, from different health centres in the Basque Country and Navarra. | Depression, Anxiety and Stress Scale (DASS 21), range 0–63 (0–21 in subscale) | 46.7% suffered stress, 37% anxiety, 27.4% depression and 28.9% sleep problems. |
| Athens Insomnia Scale (AIS), range 0–24. | Females registered a higher level of anxiety (20.9% severe and extremely severe, compared to 3.6% males), stress (13.6% versus 2.6%) and insomnia (24.9% vs 3.9%). According to age, more symptoms were registered among professionals >36 years. | ||||
| Being in contact with the disease was associated with higher levels of anxiety, stress and insomnia (p < 0.01). | |||||
| Being afraid at work and believing that confinement measures were not respected on a social level was associated with a higher level on all scales. | |||||
| Elbay, et al.48 (Turkey) | To investigate anxiety, stress and depression levels of doctors and explore their conditioning factors. | Cross-sectional descriptive | 442 professionals (57% females, average 11 years work experience), of which 231 were frontline professionals, from different hospitals | Sociodemographic data | Of all participants, 64.7% had symptoms of depression (9.5% severe and 10.2% extremely severe), 51.6% anxiety (10.6% severe and 11 extremely severe) and 41.2% stress (severe 10.4% and extremely severe 5%). |
| Depression, Anxiety and Stress Scale (DASS 21), range 0–63 (0–21 in subscale) | The mean on the total scale was 19.04 ± 12.93 (depression 6.92 ± 4.70, anxiety 4.67 ± 4.21, stress 7.46 ± 4.85). | ||||
| A higher score on the scale was associated with being female, being younger, being single, having less work experience and being a frontline worker. | |||||
| The main protective factor was having children. | |||||
| Specifically, the conditioning factors among frontline workers with the highest scores on the scale were: increased weekly working hours, increased number of Covid-19 patients cared for, lower level of support from peers and supervisors, lower logistic support and lower feelings of professional competence. | |||||
| Giusti et al.49 (Italy) | Assess the prevalence of burnout and stress, and identify the sociodemographic, work-related and psychological factors. | Cross-sectional descriptive | 330 professionals (doctors n = 140, nurses n = 86, nurse assistant n = 38, others n = 67), of which 188 were frontline workers, from three hospitals in Lombardy and Piedmont | Sociodemographic data | 71.2% manifested anxiety (mean STAI-S 47.3 ± 11.9), 67.6% moderate or severe emotional exhaustion, 26.1% moderate or severe depersonalisation, 74.3% reduced personal accomplishment, 31.3% anxiety (DASS-21 4.0 ± 2.3), 34.3% stress (DASS-21 6.8 ± 4.8) and 36.7% symptoms of post-traumatic stress. |
| State-Trait Anxiety Inventory - State form (STAI-S), range 20–80 | A higher level of burnout was found in professionals with a heavier workload, younger age, who are frontline workers and who are more emotionally worried about the situation. | ||||
| Depression, Anxiety and Stress Scale (DASS 21), range 0–63 (0–21 in subscale) | |||||
| Impactof Event Scale - Revised (IES-6) | |||||
| Maslach Burnout Inventory (MBI) | |||||
| Man et al.50 (Romania) | Evaluate disease perceptions, levels of stress and coping strategies, and compare the groups of frontline professionals with the rest of the personnel. | Cross-sectional descriptive | 115 professionals (doctors n = 46, nurses n = 46, other health caregivers n = 23), of which 48 were frontline (pulmonology ward with COVID-19 and in the ICU: doctors n = 26, nurses n = 27, other health caregivers n = 14) from the Cluj-Napoca pulmonology teaching hospital | Brief Illness Perception Questionnaire (IPQ), range 0–80 | COVID-19 was considered moderately threatening, without differences by group, although there were differences by professional category (nurses perception was of greater severity). 75% considered “at-risk” behaviour as the main cause for possible disease. |
| Perceived stress scale (PSS 10), range 0–40 | Perceived stress and emotional distress profile indicated medium and high levels, without group differences and with a positive correlation with disease perception. | ||||
| Profile of Emotional Distress (PDE) Questionnaire | 59.9% indicated receiving emotional support from the family and social environment. | ||||
| Cognitive-Emotional Regulation Questionnaire (CERQ) | The most common coping strategies were refocusing on planning and positive reappraisal, with no differences in the groups. Frontline personnel used positive refocusing more. The least common strategies were catastrophising and blaming others. | ||||
| Romero et al.51 (Spain) | Evaluate the psychological impact of the COVID-19 pandemic on healthcare workers. | Cross-sectional descriptive | 1761 professionals (doctors n = 1761, nurses n = 825, nurse assistants n = 238, others n = 285), of which 921 were frontline, from various health centres throughout Spain | Sociodemographic data | The greatest psychosocial impact was observed with p < 0.01 in the hospital setting (especially tertiary hospitals PSAS 43.9 versus 41.0 in primary hospitals), in the Emergency departments (PSAS 45.1) and ICU (PSAS 44.3), among younger personnel (20–39 years old PSAS 46.7, vs. a >60 years PSAS 37.6), Pulmonology and Geriatrics specialities (PSAS 48.3 and 47.6) and in geographic areas with incidence of COVID-19 > 245.5 per 100,000 inhabitants (PSAS 46.8 compared to 39.1 in areas with <33 cases per 100,000 inhabitants). |
| Psychological Impact of Covid-19 Group Survey (IMPSICOV): Psychological Stress and Adaptation at work Score (PSAS), generated | |||||
| from modifications of: 1. Healthcare Stressful Test; 2. Coping Strategies Inventory; 3. Font Roja Questionnaire; 4. Trait Meta-Mood Scale (TMMS-24) | |||||
| Rossi, et al.52 (Italy) | Know the mental health outcomes of health professionals | Cross-sectional descriptive | 1379 professionals (doctors n = 519, nurses n = 472, others n = 386), of which 725 were frontline, from different health centres in Italy | Sociodemographic data | 49.4% manifested symptoms of post-traumatic stress, 24.7% depression, 19.8% anxiety, 8.3% insomnia and 21.9% high self-perceived stress. |
| Post-Traumatic Stress Disorder Scale (PTSS) | In all the scales, except insomnia, women (OR 2.31), the younger age groups (OR 0.69) and frontline workers (OR 1.37) were more likely to suffer psychological symptoms (p < 0.01). | ||||
| Global Psychotrauma Scale (GPS) | |||||
| Patient Health Questionnaire (PHQ-9) | |||||
| Generalised Anxiety Disorder Scale (GAD-7), range 0–21 | |||||
| Insomnia Severity Index (ISI) | |||||
| Shechter, et al.53 (USA) | Identify the sources of distress, and the coping strategies and resources | Cross-sectional descriptive | 657 professionals (doctors n = 282, nurses 313, others n = 62), of which 536 were frontline (Emergency department n = 74, ICU n = 262, hospitalisation n = 126, outpatient n = 25) from New York | Primary Care Post-traumatic Stress Disorder (PC-PTSD) | 54% suffered stress, 48% depression, 30% anxiety and 75% sleep disturbances. |
| Patient Health Questionnaire-2 (PHQ-2) | The main sources of distress were: transmission to loved ones (74%), lack of control (71%) and lack of tests and limited personal protective equipment (68%). | ||||
| Generalised Anxiety Disorder (GAD-2), scale 0–6 | Compared to doctors, the nurses suffered more stress (64% versus 40%), depression (53% versus 38%) and anxiety (40% versus 15%), had fewer hours of sleep (5.62 ± 0.06 hours/day versus 6.24 ± 0.10) and more feelings of loneliness (p < 0.01). | ||||
| Life Orientation Test - Revised (LOT-R), Pittsburg Sleep Quality Index (PSQI) and Insomnia Severity Index (ISI) | 80% carried out at least one type of stress coping strategy: physical activity (59%), religious or spiritual activity (23%), yoga (25%) and meditation (25%). | ||||
| Self-elaborated questionnaire on coping strategies | 51% showed high interest in at least one support strategy: 33% for self-guided counselling with access to a therapist, 28% traditional individual counselling, 24% for support groups. | ||||
| Stojanov, et al.54 (Serbia) | To assess the health-related quality of life, the quality of sleep, the symptoms of depression and anxiety and their potential risk factors and to compare the results of frontline and non-frontline professionals. | Cross-sectional descriptive | 201 professionals (doctors n = 80, nurses n = 121), of which 118 were frontline professionals from various hospitals in Nis. | Generalised Anxiety Disorder (GAD-7) Scale, range 0–21 | 14.7% considered their mental status as bad, 64.3% considered that their mental status had worsened, the main factor being the fear of infecting loved ones (83.3%) or getting infected themselves (65.3%). |
| ZUNG Self-rating Depression Scale (SDS), range 25–100 | Front-line personnel registered a worse level than the rest (p < 0.01) on the sleep quality scales (8.3 ± 4.5 versus 5.3 ± 3.7), anxiety (13.26 ± 5.32 vs. 8.25 ± 5.61) and health subscales (vitality 77.3 ± 24.5 vs 81.3 ± 25.6) | ||||
| Health Survey (SF-36), range 0–100 | |||||
| Pittsburg Sleep Quality Index (PSQI), Range 0–21 | |||||
Stress. In the global samples including frontline personnel – mainly from the Emergency Services, ICUs and Pulmonology departments – and those from other units, the percentage of healthcare personnel who suffered stress ranged from 37%49 to 78%45, with a more frequent interval between 40% and 50%47,48,52 and 54% among front-line personnel53.
Regarding direct care of COVID-19 patients, the studies reflected more stress among front-line personnel43,45–48,51,52, except for the Man et al.50 study that did not find statistically significant differences. The departments with the highest levels of stress were the ICUs and Emergency departments, and the medical specialties most affected were Pulmonology and Geriatrics51.
Psychological stress varied in intensity, from mild and moderate to severe and extremely severe. On the DASS-21 scale, the mean global stress was 7.46 ± 4.8548 and 6.8 ± 4.849, with >2 points difference between frontline professionals (6.07 ± 4.10 vs 8.48 ± 4.76)47. The comparison using the post-traumatic stress symptoms Severity Scale (DSM-5), with a range 0–80, indicated a mean of 29.2 for frontline workers, compared to 21.3 for the rest of the health personnel (p < 0.01)46. Finally, on the Secondary Traumatic Stress Scale (STSS), with interval 1-5, significant differences were observed between the mean in the frontline workers (2.66 ± 0.93) compared to the other health professionals (2.46 ± 0.83) and the general population (2.34 ± 0.76)43.
By gender and professional category, the results (p < 0.05) unanimously indicated more stress among women43,45–49,52 and the nursing personnel50,53. The analysis by age drew contradictory conclusions: different studies found the highest levels of stress among younger professionals48,51,52, older professionals46,47 or reached no conclusive results43. Other factors aggravating stress were: suffering from chronic diseases or a history of mental health43,45, less work experience, greater exposure to the mass media and being single48, have a worse perception50 or living in areas with a higher incidence of the disease51.
Anxiety. On a general level, anxiety symptoms affected participating healthcare personnel in varying percentages: 20% in Italy52, 37% in the Basque-Navarre, Spain study47, 52% in Turkey48 and up to 72% in the Italian area with the highest prevalence of COVID-1949.
The intensity of symptoms, measured in Italy using the STAI tool (range 20-80) placed the total mean between 47.3 ± 11.949 and 51.3 ± 13.9 (53 in the frontline and 50 among the rest of the professionals, p > 0.05)46. The specific anxiety subscale of DASS-21 showed mean results of 2.26 ± 2.83 in the total population and 3.77 ± 3.58 in frontline professionals in Spain47, compared to the global average of 4.67 ± 4.21 in Turkey48. Finally, the GAD Scale (range 0–21) indicated 20% of professionals with >15 points in Italy52 and an average in Serbia of 8.25 ± 5.61 (n = 83) in the general group and 13.26 ± 5.32 (n = 118) in the frontline group54.
Overall, the comparative results indicated greater anxiety among frontline professionals47,48,52,54, although not always with statistical significance46, with the most affected being the nursing personnel, with 40% compared to 15% of other categories53. According to sex, women suffered a higher level of anxiety47,48,52: 21% with severe or very severe anxiety, compared to 4% of men in the north of Spain47. In some studies, older in years was a protective factor for anxiety48,52, while in others it entailed more symptoms47.
Depression. Between 25%52 and 31%49 of all healthcare professionals showed symptoms of depression in Italy, while in a Turkish study the percentage reached 65%, of which 20% were severe or extremely severe48. In the United Kingdom, 64% of the total sample responded affirmatively to the phrase “I feel low, sad or depressed”45.
The quantification of the symptoms of depression showed variable results in the different studies, with a greater impact on the frontline personnel and, within this group 53% were nurses, compared to 38% of other professional categories53. In BDI-II (range 0-63), the general mean score was 13.7 (compared to 9.8 for the rest of the professionals, p< 0.05)46. The global mean scores in the measurement with the DASS-21 subscale ranged from 2.68 ± 3.14 in Spain (3.78 ± 3.85 in the frontline workers, p < 0.05)47, 4.0 ± 2.3 in Italy49 and up to 6.92 ± 4.70 in Turkey48. In Serbia, after applying the Zung Self-Rating Depression Scale (SDS), with an interval 25-100, the results indicated a mean of 46.39 ± 10.61, vs 53.14 ± 11.41 in frontline professionals (p > 0.05)54.
Symptoms of depression affected women to a greater extent46,48,52, single people46,48 and younger age groups52 or those with less work experience48.
Sleep disturbance. Sleep disorders were observed in 8%52 and 55%44 of the total samples in Italy, 29% in Spain47 and up to 72% in the UK45. Frontline personnel showed greater sleep disturbance, with a mean of 9.42 ± 3.47 vs 8.77 ± 3.27 on the Athens Insomnia Scale with range 0-2447 and 8.3 versus 4.5 mean in the Pittsburg Sleep Quality Index, with a range of 0-2154. Among the frontline personnel, nursing had least rest: 5.6 h/day compared to 6.2 h/day among the other professionals53. Women had severe and very severe insomnia problems in 25%, compared to 4% of men47.
Burnout. In Italy, all health personnel reported high (32%) and medium (36%) levels of emotional exhaustion and depersonalisation (12% high and 14% moderate), with higher burnout among frontline personnel who had a greater workload and were younger (p< 0.05)49. In the frontline population, the percentages of high and medium emotional exhaustion reached 37% and 23% and in depersonalisation they reached 25% and 22.9% respectively44, being more intense among women and nursing personnel, and related to a worse self-perceived state of health.
Coping strategies and measures. Most of the health personnel showed interest and positively valued individual and group psychological support measures45,53 and practiced physical, religious, and spiritual activities to reduce stress, anxiety and depression53. The most used coping strategies were refocusing and positive reappraisal50.
In the critical evaluation of the methodology (Table 5), it was observed that, in general, the studies met most of the standard criteria of good practices for cross-sectional quantitative studies. The aspects with the poorest quality were sample representativeness, the selection biases and validation of the data collection instrument.
Evaluation of methodological quality.
| Author (country) | Design | Instrument | Data collection | Data analysis | Discussion | ||||
|---|---|---|---|---|---|---|---|---|---|
| Clear objective | Methods | Validation | Sample selection | Sample representativeness | Explains selection biases | Description | Significant results | Discuss validity and limitations | |
| Arpacioglu et al.43 (Turkey) | Yes | Yes | Yes | Yes | No | No | Yes | Yes | Yes |
| Barello, et al.44 (Italy) | Yes | Yes | Yes | Yes | No | No | Yes | Yes | Yes |
| Cipolotti, et al.45 (UK) | Yes | Yes | No | Yes | Not clear | Not clear | Yes | Yes | Yes |
| Di Tella, et al.46 (Italy) | Yes | Yes | Yes | Yes | No | No | Yes | Yes | Yes |
| Dosil, et al.47 (Spain) | Yes | Yes | Yes | Yes | No | Yes | Yes | Yes | Yes |
| Elbay, et al.48 (Turkey) | Yes | Yes | Not clear | No | No | No | Yes | Yes | Yes |
| Giusti, et al.49 (Italy) | Yes | Yes | Yes | Yes | Not clear | Yes | Yes | Yes | Yes |
| Man, et al.50 (Romania) | Yes | Yes | Yes | Yes | Not clear | No | Yes | Yes | Yes |
| Romero, Catalá, Delgado et al.51 (Spain) | Yes | Yes | Yes | Yes | Not clear | No | Yes | Yes | Yes |
| Rossi, et al.52 (Italy) | Yes | Yes | Yes | Yes | No | No | Yes | Yes | Yes |
| Shechter, et al.53 (USA) | Yes | Yes | Yes | Yes | No | No | Yes | Yes | Yes |
| Stojanov, et al.54 (Serbia) | Yes | Yes | Yes | Yes | Not clear | Yes | Yes | Yes | Yes |
The review of studies carried out in the Western world reflected variable levels of stress, anxiety, depression, sleep disturbance and burnout in the population of health professionals from different countries in Europe and the USA. The presence of more frequent and intense symptoms was seen among frontline personnel, as well as among females and individuals in the nursing category. In addition to the relative scarcity of published studies, a joint but not always comparative approach of data analysis was observed, with no discrimination between frontline professionals and the rest of the health personnel. In this respect, this review evidenced the need for rigorous knowledge of the socio-demographic and professional profile of the personnel directly involved in the health care of COVID-19 patients.
The methodological quality of the studies was optimal, except regarding the participation rate and the control of possible selection biases and sample representativeness which were justified in the epidemiological context, and the generalised difficulties imposed by the SARS outbreak, both in the healthcare and research teams55.
This review had a number of limitations. Despite the systematic search and selection method, there was an idiomatic bias, and some articles may have been omitted, especially because of including the specification of frontline health personnel in the search strategy. Furthermore, in the context of maximum prioritisation of the topic and rapid management of the publications, a comparative study that was sensitive to the differences between the characteristics and the impact of acute and chronic psychological stress was not possible. The socio-demographic heterogeneity of the participating samples, as well as the instruments and questionnaires used, made it difficult to compare and extrapolate results and to analyse biases. However, to date, there are no known systematic reviews focused on frontline professionals in the Western world, which may represent the main strength of this study.
The heterogeneity of samples, instruments, and results already observed in previous reviews on the psychological impact of the pandemic in China and other Asian countries13–17, made it difficult to compare the psychological impact of the SARS-CoV-2 outbreak on health personnel in different geographical settings. However, this review showed a higher prevalence of anxiety in Western studies compared to those carried out in China, where anxiety was below the European percentages (between 23 and 44%)4,7,11 and only 6.2% of professionals exceeded the threshold of 15 points (severe anxiety) on the GAD-7 scale, compared to 20% in Italy52, with means in Asia of 1.3011 or 8.2 points7, compared to 8.25 (13.26 in frontline personnel) in Serbia54. This review also recorded a higher level of stress compared to the range of 4% to 68% found in professionals in China13.
Regarding the symptoms of depression and sleep disturbance, the results were similar to those observed in Asia, with the condition varying from one quarter13,15 to over half4,5,11 of professionals affected by mild or moderate depression and approximately one third by insomnia4,13,15,16. This indicated more moderate symptoms than during the SARS or MERS health crises15. However, these data should be interpreted with caution, as symptoms such as depression, shown in 23% of professionals31 or burnout, post-traumatic stress and addictive behaviors can continue medium- to long-term, with some being recorded two years after exposure to the SARS-CoV-1 outbreak55.
In relation to the differences between frontline personnel and the rest of the professionals, the Western studies showed that the greatest psychological impact occurred in cases of direct contact with infected patients. This confirmed the data observed in China regarding the level of stress (OR 1.60; CI 1.25–2.04), depression (OR 1.52; CI 1.11–2.09), anxiety (OR 1.57; CI 1.22–2.02) and insomnia (OR 2.97; CI 1.92–4.60)4. Other authors also highlighted that the long working hours, the concentration, and permanent vigilance required when working in the Emergency Services, ICUs and Pulmonology departments in situations of pandemic respiratory diseases, as well as the contact with suffering and death10 worsened the psychological state of the professionals8,56.
While the effect of age was not conclusive, the main explanatory variables for a higher prevalence of psychological symptoms were gender and professional category. The results were similar to those in Asia4,15,16, where females and nursing personnel suffered more anxiety (25.7% females versus 11.6% males and 26.9% nurses versus doctors 14.3%)11, depression (mean GAD-7: females 4.0 [1–7] versus males 2.0 [0–6] and nurses 5.0 [2–8] versus doctors 4.0 [1–7])4 and stress.
Given the increased risk and exposure to mental health problems among women, both in pandemic situations and on a general level29, and taking into account the high feminisation of the health sector in the western world57, the planning and design of support measures and interventions to reduce the psychological impact, widely documented in recent months58, would have to include the gender perspective59. Furthermore, in light of the evidence that the majority of professionals accept and seek these interventions, an individualised approach would be necessary to optimise the results. This approach should take into account socio-demographic variables, the professional role, direct contact with patients or a history of mental health60, while bearing in mind that protective measures and psychological support are necessary despite the mildness of the symptoms7.
Finally, this review highlights the need to use qualitative methodologies to delve deeper into the experiences and specific needs of healthcare personnel, especially the frontline workers, as well as to explore the medium- and long-term implications on their physical and mental health and emotional.
Conflict of interestsThe author declares that she has no conflict of interest.
Please cite this article as: Danet Danet A. Impacto psicológico de la COVID-19 en profesionales sanitarios de primera línea en el ámbito occidental. Una revisión sistemática. Med Clin (Barc). 2021;156:449–458.