To study the incidence of infection in close contacts with patiens with SARS-CoV-2 infection using a telephone monitoring protocol after the recommendation of isolation and quarantine at home.
Patients and methodsCohort study, with 124 patients older than 15 years, included consecutively, asymptomatic at the time of the consultation, who had had close contact (<2 m) with confirmed or possible cases of SARS-CoV-2 infection. The intervention consisted of 2 weeks of home isolation and quarantine, contacting by phone on days, 2, 4, 7 and 14 after the contact. The event of interest was the appereance of symptoms compatible with SARS-CoV-2 infection.
ResultsThe average age was 45.1 years (55.6% women); 328 phone calls were made (average 2.6 calls for patient). After 2 weeks of follow-up, 6 patients developed symptoms, confirming serologically or by PCR in 3 of them (2.4%, CI 95%: 0.8–6.9).
ConclusionsThe incidence of SARS-CoV-2 infection in close contacts is low 2 weeks after home isolation and quarantine at home.
Estudiar mediante un protocolo de seguimiento telefónico la incidencia de infección en los contactos estrechos de pacientes con infección por SARS-CoV-2 tras la recomendación de aislamiento y cuarentena en el domicilio.
Pacientes y métodosEstudio de cohortes, con 124 pacientes mayores de 15 años, incluidos consecutivamente, asintomáticos en el momento de la visita, con contacto estrecho (<2 metros) con casos confirmados o posibles de infección por SARS-CoV-2. La intervención consistió en aislamiento y cuarentena en domicilio durante 2 semanas, contactando telefónicamente los días 2, 4, 7 y 14 tras el contacto. El evento de interés fue la aparición de clínica compatible con infección por SARS-CoV-2.
ResultadosLa edad media fue de 45,1 años (55,6% mujeres). Se realizaron 328 llamadas telefónicas (media de 2,6 llamadas por paciente). Tras 2 semanas de seguimiento desarrollaron síntomas 6 pacientes, confirmados serológicamente o por PCR en 3 de ellos (2,4%; IC 95%: 0,8–6,9).
ConclusionesLa incidencia de infección por SARS-CoV-2 en los contactos estrechos es baja a las 2 semanas tras el aislamiento y cuarentena domiciliarios.
The infection by the coronavirus called SARS-CoV-2, better known as COVID-19, has had a great impact on health1. Primary Care decided to prioritise telephone monitoring of the infection so as not to expose patients and health personnel to new infections. The strategy focused on: identifying any moderate and severe cases and referring them to the hospital; diagnosing mild cases and sending them home with symptomatic treatment, quarantine and isolation rules, and telephone follow-up; and, finally, follow-up of patients who enquired about having had close contact with with confirmed or possible SARS-CoV-2 infection cases.
However, the results of the follow-up of the contacts in our environment, as well as the effectiveness of the quarantine and isolation measures in these cases, are not well known. A recent Cochrane review2 highlighted the lack of studies, as the available evidence is based mostly on similar virus infections and model-based studies.
The objective of this study is to analyse the incidence of SARS-CoV-2 infection in people with close contact with confirmed or possible cases of said infection by means of a telephone follow-up protocol after the recommendation to isolate and quarantine at home.
MethodsThis is a cohort study, which includes patients over 15 years of age who came to the consultancy in a health centre in the city of Barcelona between 6 March and 24 April 2020, and who had had close contact (less than 2 m, without a mask, in the previous week, indoors or outdoors) with a confirmed or possible SARS-CoV-2 infection case, and who were asymptomatic at the time of the visit, whether in person or by phone, and by their own initiative or referred by other medical services, such as private health insurance companies. Exclusion criteria included patients who only requested a doctor’s note for time off work due to risk factors for SARS-CoV-2 infection if the possible infection from the contact was not well documented according to medical criteria, and cases in which phone follow-up would not be possible at 2 weeks or later (one month from contact).
Inclusion criteria included patients who were given a doctor’s note for time off work if they needed it, with a recommendation for 2 weeks’ isolation and quarantine at home after contact, and the provision of written recommendations if they had to live in the same house together with infected patients3. Three GPs made the follow-up telephone calls on days 2, 4, 7 and 14 after the contact, specifically asking about the most frequent symptoms suggestive of infection: fever, cough, changes in taste or smell, diarrhea, dyspnea, and generally feeling unwell4. Based on clinical criteria, it was decided whether the patient had developed a SARS-CoV-2 infection during the follow-up, in which case a more intensive protocol of telephone follow-up was applied. In this case, patients were called on days 2, 4, 7, 10, and 14 after the onset of symptoms, with additional calls on days 1, 3, and 5 if they had risk factors for SARS-CoV-2 infection4, which enabled respiratory complications to be detected early on. If the patient presented alarm symptoms, such as high fever for more than 3 days, dyspnea with slight effort or a persistent cough, then an urgent chest X-ray was requested and the patient was referred to the hospital if pneumonia was confirmed. If the patient was not located after 2 phone calls, two additional calls were made the following day.
The study variables were the following: age (years), sex, risk factors for SARS-CoV-2 infection known at the beginning of the study4, number of follow-up calls, type of contact (cohabitant in the same address, close family member, friend or acquaintance and work contact), diagnosis in the follow-up of possible SARS-CoV-2 infection and performance of PCR or serology. If a PCR was not available during the clinical phase, then a qualitative rapid test in capillary blood was given at 2 months to obtain serological confirmation of the diagnosis of the cases that developed the infection. This had a sensitivity of 86.4% and a specificity of 99.6% (COVID-19 IGG/IGM Rapid Test Cassette, Guangzhou Wondfo Biotecht Company). The study was approved by the local ethics committee (Fundació Jordi Gol, file 20/087-PCV).
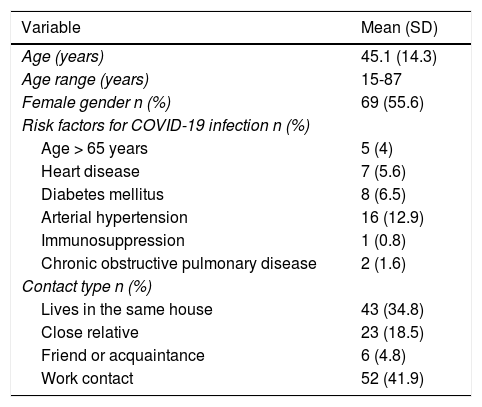
Results124 patients were included. The characteristics are described in Table 1. Most of the contacts were with people who lived at the same address or work colleagues. A total of 328 follow-up telephone calls were made (mean 2.6 calls per patient; SD 1.3).
Characteristics of the patients (n = 124) included in the study.
| Variable | Mean (SD) |
|---|---|
| Age (years) | 45.1 (14.3) |
| Age range (years) | 15-87 |
| Female gender n (%) | 69 (55.6) |
| Risk factors for COVID-19 infection n (%) | |
| Age > 65 years | 5 (4) |
| Heart disease | 7 (5.6) |
| Diabetes mellitus | 8 (6.5) |
| Arterial hypertension | 16 (12.9) |
| Immunosuppression | 1 (0.8) |
| Chronic obstructive pulmonary disease | 2 (1.6) |
| Contact type n (%) | |
| Lives in the same house | 43 (34.8) |
| Close relative | 23 (18.5) |
| Friend or acquaintance | 6 (4.8) |
| Work contact | 52 (41.9) |
Variables expressed as number and (%) and mean and (SD).
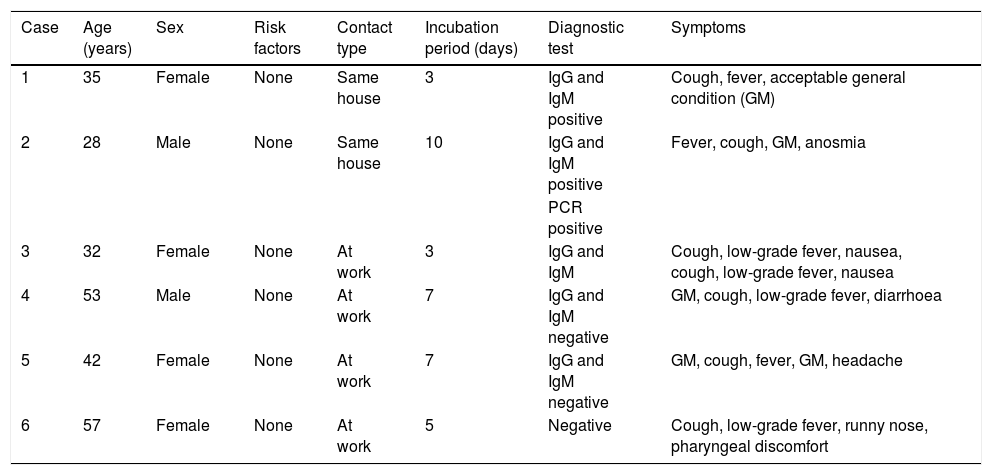
At the end of the follow-up, according to clinical criteria, a total of 6 patients had developed a SARS-CoV-2 infection (4.8%; 95% CI: 1.8–10.2). However, the diagnostic tests were only positive in 3 cases (2.4%; 95% CI: 0.8–6.9), in one case by PCR and in 2 cases by positive IgG and IgM serology (both). The characteristics of the 6 patients are detailed in Table 2. Additionally, PCR was available in 27 of the 118 contacts who did not clinically develop the infection, which was negative in all cases.
Characteristics of the 6 cases that developed symptoms of SARS-CoV-2 infection.
| Case | Age (years) | Sex | Risk factors | Contact type | Incubation period (days) | Diagnostic test | Symptoms |
|---|---|---|---|---|---|---|---|
| 1 | 35 | Female | None | Same house | 3 | IgG and IgM positive | Cough, fever, acceptable general condition (GM) |
| 2 | 28 | Male | None | Same house | 10 | IgG and IgM positive | Fever, cough, GM, anosmia |
| PCR positive | |||||||
| 3 | 32 | Female | None | At work | 3 | IgG and IgM | Cough, low-grade fever, nausea, cough, low-grade fever, nausea |
| 4 | 53 | Male | None | At work | 7 | IgG and IgM negative | GM, cough, low-grade fever, diarrhoea |
| 5 | 42 | Female | None | At work | 7 | IgG and IgM negative | GM, cough, fever, GM, headache |
| 6 | 57 | Female | None | At work | 5 | Negative | Cough, low-grade fever, runny nose, pharyngeal discomfort |
GM: general malaise.
The results of the study indicate that the application of a telephone follow-up protocol accompanied by quarantine and isolation measures is effective, although the absence of a control group means that we must exercise caution when interpreting the results. A recent seroprevalence study5 carried out by the Spanish Ministry of Health showed that the prevalence of infection in our health centre, which is similar to the rest of Catalonia, was around 5%. These figures seem to confirm the efficacy of population isolation and quarantine measures. As our study population is in close contact with confirmed or possible cases of SARS-CoV-2 infection, we think that the figure of 2.4% of new confirmed cases is relatively low.
Although the evidence on the efficacy of quarantine and isolation measures in SARS-CoV-2 contacts is low or very low2, the findings are consistent with the decrease in the incidence and mortality of SARS-CoV-22. In a study of contacts in Taiwan6 in which a 14-day quarantine was also recommended, the probability of developing the disease was also very low (0.7%), although it was higher if the contact was living in the house (4.6%) or was a family member (5.3%). However, in a similar study in China7 the percentage was higher: 6%, although it was at the start of the pandemic.
Our study has limitations. First is the absence of a control group, which is difficult to implement in a pandemic situation for ethical reasons. Second, due to limited availability, PCR tests were not available to confirm infection in all the cases with confirmed or possible infection, prioritising those admitted to hospitals. However, those without compatible symptoms were ruled out. Neither was it possible to rule out possible asymptomatic carriers, and it was assumed that the patients had no infection if there were no symptoms at 14 days after contact. Third, not all the patient’s contacts were followed up, as they frequently belonged to other health centres, which are being used less in this pandemic situation in which the most effective measure is population isolation and quarantine2, and this happened in the same way between the dates of our study. Furthermore, not all patients informed of the situation on the first day of contact, which reduced the average number of telephone calls. Fourth, there was no distinction between indoor and outdoor contact. Finally, we did not have diagnostic tests in all contacts, which would have been the ideal scenario, due to the magnitude of the pandemic. However, PCR was available in 27 asymptomatic contacts (mostly people from the healthcare sector such as nurses, orderlies and assistants, carried out during the first week after contact), with all being negative, and infection in symptomatic contacts was confirmed by PCR or serology.
Other measures are necessary, in addition to home isolation, reduced mobility or limitations on leisure activities and commerce, to reduce community transmission2, such as the use of masks, face shields or social distancing, due to the seriousness of the transmission by SARS-CoV-2 aerosols8. A recent systematic review9 has shown the effectiveness of these three measures, with reductions in contagion greater than 80% for each of these measures. Likewise, it is necessary to quickly detect and control cases and their contacts, and proceed to their quarantine and isolation, in addition to the need for effective surveillance and control services10. In this sense, we think that the role of Primary Care, with teams of doctors and nurses with an important territorial presence and who know the patients and their environment better than other health personnel, could be of great use.
FundingThis work has not received any type of funding.
Conflicts of interestNone.
Please cite this article as: Baena-Díez JM, Pinnegar HP, Paredes-Millán MK, Plaza-Cerrato L, Palomino-Español E, Cots JM. Incidencia de infección por SARS-CoV-2 en contactos estrechos. Seguimiento telefónico en Atención Primaria. Med Clin (Barc). 2021;156:444–446.