Esophagitis is a group of clinical entities manifesting with inflammation and lesions in the esophageal mucosa. These conditions can be linked to multiple etiopathogenic mechanisms in addition to gastroesophageal reflux, with the most common ones being the consumption of certain medications, infectious agents, or involvement of the mucosa in the context of immunoallergic diseases.
In this paper we describe the case of an immunocompetent patient presenting with symptoms of esophagitis two days after receiving the first dose of messenger ribonucleic vaccine (mRNA) mRNA-1273 (Moderna) against the 2019 coronavirus disease (COVID-19).
This was a 20-year-old male patient with a history of recurrent episodes of streptococcal pharyngitis. As remarkable immunological history he reported rhinitis and allergic conjunctivitis since his childhood, a reaction to the pertussis vaccine (fever and irritability), and atopic dermatitis.
He visited the Emergency Room due to experiencing dysphagia, odynophagia, and retrosternal pain for 5 days, but no associated heartburn. In addition, he had a fever of up to 39 °C and reported complete inability to ingest food orally. He had received the first dose of the cited vaccine two days prior to the onset of these symptoms.
The blood work performed revealed normal findings and a COVID-19 detection polymerase chain reaction (PCR) test was negative.
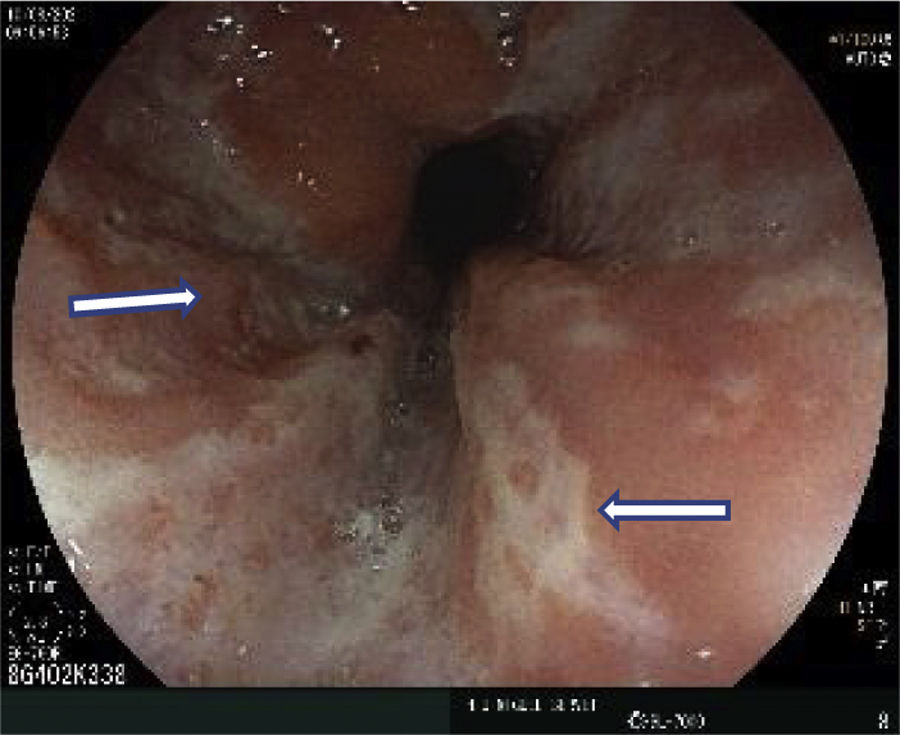
An urgent gastroscopy was consequently carried out, detecting multiple superficial, small, and punctiform ulcerations in the middle third of his esophagus suggestive of infectious esophagitis. Initial endoscopic diagnosis: infectious esophagitis of probable herpetic origin (Fig. 1).
During his stay at the clinic, he had serology tests performed against human immunodeficiency viruses (HIV) 1 and 2, cytomegalovirus (CMV), and immunoglobulin G (IgG) of the herpes simplex virus (HSV), all of which were negative.
A pathology study yielded a diagnosis of severe, acute, ulcerative esophagitis without viral cytopathic changes nor fungal structures permeating the epithelium. An immunohistochemistry study was also negative for HSV-1 and CMV. The examined sample was found to contain lymphocytes, neutrophils, and squamous cells that were either dispersed or forming small plaques, without overlapping nuclei nor cytologic atypia.
During his stay at the clinic, the patient required total parenteral nutrition for 6 days, as well as intravenous antiviral therapy due to the initial suspected diagnosis of herpetic esophagitis, exhibiting a gradual clinical improvement until achieving the reintroduction of an oral diet. Given the above reaction, the patient refused to receive the second dose of the vaccine. In the absence of a clear cause of the esophagitis, the case was notified to the Spanish Pharmacovigilance System for Medicines for Human Use due to its potential relationship with the vaccination.
Different authors have described the existence of a possible relationship between infection by the severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) and the onset of autoimmune conditions mediated by a mechanism of molecular mimicry and cross-reactivity.1 These reactions might also be triggered by vaccination, particularly in genetically predisposed individuals.2
Vaccine-associated autoimmunity is a well-known phenomenon attributed to cross-reactivity between antigens or to an effect of the adjuvant (substance that increases the immunogenicity of antigens).3 With the appearance of the COVID-19 vaccine, this issue was further complicated by the nucleic acid formulation and the accelerated development process enforced by the emergency situation resulting from the pandemic.4 Because mRNA vaccines have shown the highest level of evidence based on the efficacy and safety profiles observed in clinical trials, their use is currently both authorized and recommended.
Thus far, mRNA vaccines were primarily designed for the treatment of cancer and infectious diseases. They are based on the synthesis of ribonucleic acid (RNA) strands encoding the desired antigenic proteins and take advantage of the intrinsic immunogenicity of nucleic acids.
It is important to note that the regulation of these immune pathways is widely considered to be the basis of several immune-mediated diseases, especially in genetically predisposed subjects.
In this particular case of a patient with a personal history of atopic dermatitis, allergic rhinitis, and a childhood vaccine reaction, we believe that the vaccine may have been the trigger of the manifested autoimmune reaction. The time elapsed between the administration of the first vaccine and the onset of the clinical picture in our patient yielded a score of 6 in the Naranjo causality algorithm (possible causal reaction).
Please cite this article as: Moliner JV, Palacio JG, Bernardos AB. Esofagitis aguda tras la administración de vacuna ARNm-1273 contra el SARS-COV-2. Med Clin (Barc). 2022;159:e13–e14.