Patients with systemic lupus erythematosus (SLE) are more vulnerable to higher levels of stress and psychopathological symptoms than the general healthy population. Therefore, the COVID-19 outbreak could alter their psychological state. The objective was to analyze the psychological impact of the pandemic and confinement on stress levels and psychopathological symptoms in patients with SLE.
Patients and methodIn this cross-sectional study, stress levels were compared with the Perceived Stress Scale, the Stress Vulnerability Inventory and psychopathological symptoms of the SCL-90-R Symptom Inventory in patients with SLE during the period of confinement (group 1; n = 276) in comparison to patients with SLE evaluated in a period before the pandemic (group 2; n = 152).
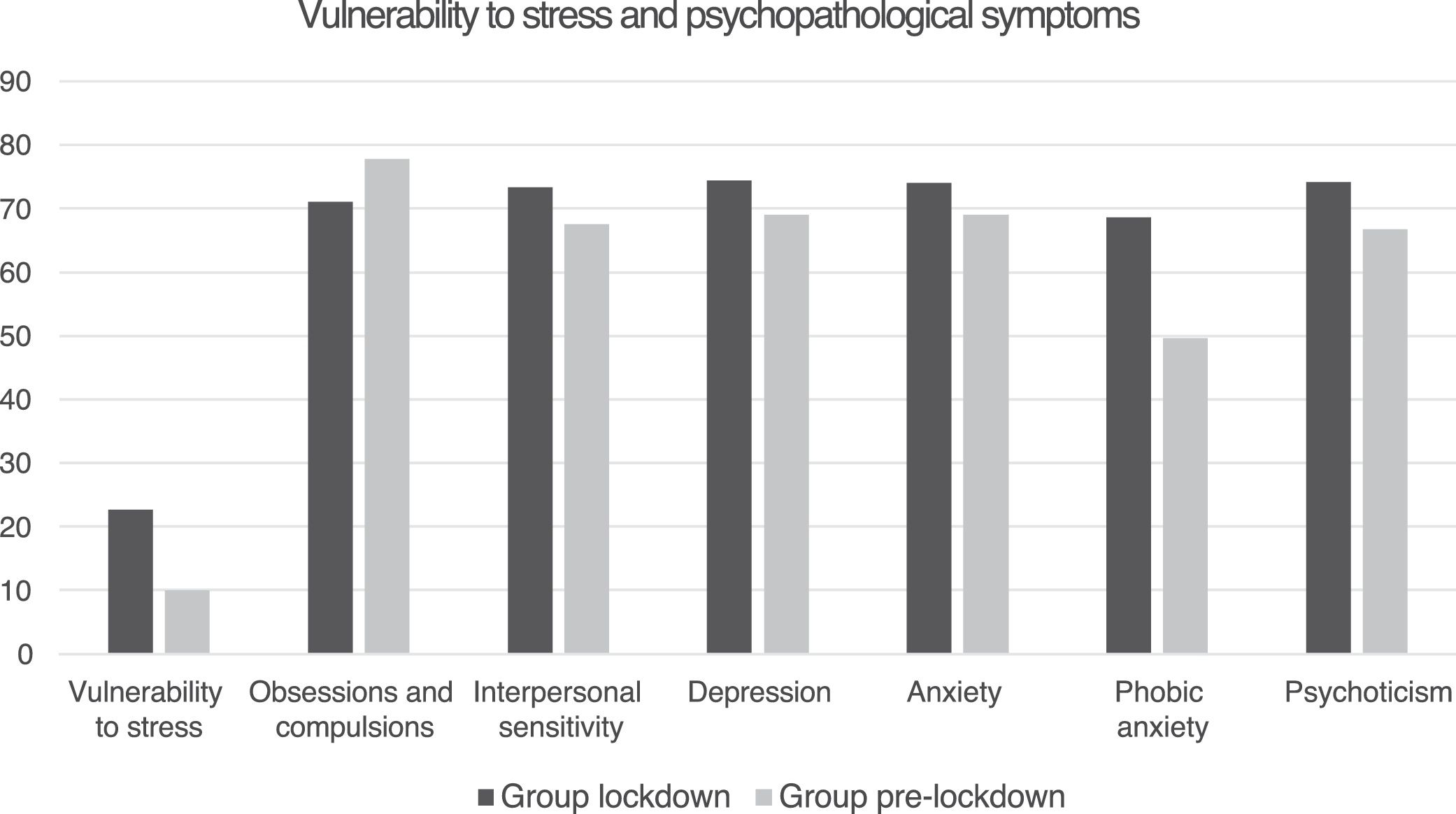
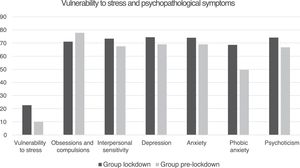
ResultsThe comparison between both groups showed there were statistically significant differences in vulnerability to stress (p < 0.0001), depression (p ≤ 0.05), anxiety (p ≤ 0.05), phobic anxiety (p < 0.0001), interpersonal sensitivity (p ≤ 0.043), and psychoticism (p ≤ 0.023). In these variables, the group of patients with lupus in confinement obtained higher scores.
ConclusionsThe confinement and threat of the COVID-19 outbreak had important repercussions on the psychological state of patients with SLE with high levels of stress, anxiety, and depression. These findings show their vulnerability to a public health alert and indicate the need to carry out a psychological approach to these patients while the state of health emergency lasts as well as to possible outbreaks of the virus.
Las pacientes con lupus eritematoso sistémico (LES) son más vulnerables a presentar mayores niveles de estrés y síntomas psicopatológicos que la población general sana, por lo que el brote de la COVID-19 podría alterar su estado psicológico. El objetivo fue analizar el impacto psicológico de la pandemia y del confinamiento sobre los niveles de estrés y sintomatología psicopatológica en pacientes con LES.
Pacientes y métodoEn este estudio transversal se compararon niveles de estrés mediante la Escala de Estrés Percibido y el Inventario de Vulnerabilidad al Estrés, y síntomas psicopatológicos mediante el Inventario de síntomas SCL-90-R, en pacientes con LES durante el período de confinamiento (grupo 1; n = 276) con respecto a pacientes con LES evaluadas en un período anterior a la pandemia (grupo 2; n = 152).
ResultadosLa comparación entre ambos grupos mostró que existían diferencias estadísticamente significativas en vulnerabilidad al estrés (p < 0,0001), depresión (p ≤ 0,05), ansiedad (p ≤ 0,05), ansiedad fóbica (p < 0,0001), sensibilidad interpersonal (p ≤ 0,043), y psicoticismo (p ≤ 0,023). En estas variables el grupo de pacientes con lupus en confinamiento obtuvo puntuaciones superiores.
ConclusionesEl confinamiento y la amenaza del brote por COVID-19 ha tenido importantes repercusiones en el estado psicológico de las pacientes con LES, mostrando altos niveles de estrés, ansiedad y depresión. Estos hallazgos muestran su vulnerabilidad ante una alerta de salud pública, y señala la necesidad de realizar un abordaje psicológico de estas pacientes mientras dure el estado de emergencia sanitaria, así como ante posibles rebrotes del virus.
Coronavirus disease (COVID-19) was first reported in Wuhan City, China, in December 20191, leading to a lockdown situation in most of the affected countries.
This disease has also been shown to primarily affect older people and people with underlying diseases such as hypertension, cardiovascular disease, diabetes mellitus, chronic obstructive pulmonary disease, malignancies, and chronic kidney disease2. Although everyone is vulnerable to this virus, special attention should be paid to older people and people with underlying and immunosuppressed diseases such as people with autoimmune disease who have been shown to be vulnerable to COVID-193. Patients with systemic autoimmunity show a higher probability of hospitalization, while people with inflammatory arthritis or systemic lupus erythematosus (SLE) do not show the same risk4. However, people with SLE are also susceptible to serious health complications from COVID-19 infection, mainly those with kidney failure or obesity5.
A study with a healthy population at the beginning of the pandemic in China showed that 53.8% rated the psychological impact of COVID-19 as moderate to severe. Their symptoms of depression (16.5%), anxiety (28.8%) and stress (8.1%) were also moderate to severe6. On the other hand, being female, a student, having specific physical symptoms (e.g., myalgia or dizziness), and poor self-reported health status were significantly associated with greater psychological impact of the pandemic and higher levels of stress, anxiety, and depression.
In addition to these factors, other reactions to COVID-19 such as the presence of specific and uncontrolled fears related to becoming infected, generalized anxiety, loneliness, frustration, and boredom seem to be related to a reduction in subjective psychological well-being and quality of life. In contrast, resilience and social support are shown to be protective factors that facilitate the development of mechanisms for readaptation to the health emergency situation7.
In the case of patients with SLE, they show higher levels of perceived stress, as well as psychopathological symptoms compared to the healthy population8. Specifically, they score higher on somatizations, obsessions/compulsions, interpersonal sensitivity, depression, anxiety, hostility, phobic anxiety, and psychoticism. Furthermore, these variables are largely related to the levels of stress experienced. In particular, it has been shown that everyday stress, rather than stressful life events, is associated with a worsening of SLE9. Also, there is a higher prevalence of anxiety and depression in patients with SLE10. These findings could indicate an increased vulnerability of these patients to psychological disorders during the health emergency situation with consequences on their disease, as the state of alarm decree together with the lockdown measures adopted could increase stress levels and negatively affect the psychological and physical well-being of these patients.
In addition, the perception of increased vulnerability to the consequences of this new disease, as well as the lockdown measures adopted, can lead to stress and psychological distress.
Therefore, the objective of this study was to analyse the psychological impact of COVID-19 and the lockdown situation associated with the pandemic on stress levels and psychopathological symptoms in patients with SLE.
Patients and methodsParticipantsThe sample consisted of 428 women with SLE, with a mean age of 41.83 (SD = 11,29) divided into 2 groups: a group evaluated during the lockdown period for COVID-19 (lockdown group) and a group evaluated before lockdown (pre-lockdown group).
The lockdown group consisted of 276 women with SLE (64.5%) who completed the online form using Google Forms. Participants were contacted by their medical staff and through social networks (Facebook, Twitter, etc.) of the associations to which they belong in relation to their disease such as the Spanish Lupus Federation (FELUPUS). On the other hand, the pre-lockdown group consisted of 152 patients with SLE (35.5%) from the “San Cecilio Clinical University Hospital” in Granada (Spain). All met at least 4 criteria of the American Association of Rheumatology for the diagnosis of SLE. The inclusion criteria for both groups were: of legal age, having a diagnosis of SLE, and knowing how to read/write in Spanish.
The patient information leaflet, the revocation document and the informed consent were provided to all participants. The study was approved by the Clinical Research Ethics Committee of the University of Jaén (JUN.20/2.PRY) and was carried out in accordance with the principles of the Declaration of Helsinki11 and the Directive on Good Clinical Practices (Directive 2005/28/CE) of the European Union.
Variables and toolsThe main sociodemographic, clinical and lockdown variables were collected using the questionnaire designed for the study. In addition, the following psychological evaluation tools validated in Spanish were used.
Clinical variablesThe progression time of the disease, current pharmacological treatment and possible diagnosis of psychological disorders were recorded. Likewise, in relation to the course of the disease during lockdown, questions about disease worsening or possible exacerbations and about the continuation of medical follow-up despite the exceptional healthcare alert situation were included.
Lupus symptom inventory12It assesses lupus symptoms experienced by patients on a given day. It consists of 7 items in which the perception of each symptom must be scored from 0 to 10. Symptoms included are: loss of appetite, general malaise, joint pain, tiredness or fatigue, skin rashes, abdominal pain, and shortness of breath. This tool has a high internal consistency with a Cronbach’s α of 0.86; furthermore, the inter-rater reliability analysis shows a high agreement between the medical report and the test scores.
Psychological variables- -
Perceived stress scale13. The Spanish version of Remor and Carrobles was used14. It is a self-report tool that assesses the level of perceived stress and the degree to which people find their life to be unpredictable, uncontrollable, or overloaded. It consists of 14 items with 5 possible answers, the highest score corresponds to the highest perceived stress. The Spanish version of the Perceived Stress Scale (14 items) demonstrated adequate reliability (internal consistency 0.81 and test-retest 0.73), concurrent validity and sensitivity15.
- -
Stress vulnerability inventory16 in the Spanish version17. It is composed of 22 items with 2 possible answers (yes = 1; no = 0) and assesses the individual's predisposition to be influenced by stress symptoms. It has a Cronbach's α of 0.87 and adequate convergent validity, showing a statistically positive correlation (p < 0.01) with other assessment tools: State-Trait Anxiety Inventory STAI, Beck Depression Inventory and Somatic Symptom Scale.
- -
Inventory of psychopathological symptoms SCL-90-R18. Used to evaluate psychopathological symptoms. It is a self-report scale made up of 90 items, with 5 possible answers (0–4). The person must respond based on how they have felt during the last 7 days, including the day when the inventory was administered. It evaluates 9 primary dimensions (somatizations, obsessions and compulsions, interpersonal sensitivity, depression, anxiety, hostility, phobic anxiety, paranoid ideation, and psychoticism), and 3 global indices of psychological distress (Global Severity Index [GSI], total of positive symptoms [PS] and positive symptomatic distress index [PSDI]). For statistical analyses, the percentile of the results of each participant in this inventory was calculated.
The lockdown experience of the lockdown group was assessed through a series of criterion questions related to housing characteristics, living with other people and the quality of relationships, their work situation during lockdown, the amount of time they had spent without leaving home (lockdown time), the diagnosis of COVID-19 or the existence of symptoms, the recent loss of close people, possible sleep problems, fear of contagion, perceived social support, psychological assistance (telephone or online), follow the news about COVID-19, routines and hobbies practiced during this period, healthy eating habits or increase in smoking.
ProcedureThe participants in the pre-lockdown group were recruited and informed before the pandemic by their autoimmune disease specialist doctors at the hospital regarding participation in a study on psychopathological symptoms and stress in patients with SLE. Once they agreed to participate in the research, they were provided with the form containing the previously mentioned evaluation tools. On the other hand, the lockdown group participants were recruited and assessed in May 2020, during the state of health emergency and lockdown due to COVID-19 in Spain, by their specialist doctors and through social networks of SLE-related associations. This group, in addition to completing the questionnaires related to the psychological and clinical variables, also answered the questions related to lockdown.
Statistical analysisThe statistical analysis of the results was carried out using the IBM® SPSS® Statistics v.26 software (IBM Corporation, Armonk, New York, USA).
First, to test for significant differences between the two groups in the main socio-demographic and disease variables, the Student’s t test was used for continuous variables and the Chi-square test (χ2) for categorical variables.
Second, in order to check whether there were differences in the variables of stress and psychopathological symptoms between the lockdown group and the pre-lockdown group, different Student’s t tests were carried out with the independent variable being the 2-level group (lockdown group versus pre-lockdown group) and the dependent variables being the scores obtained on the subscales of the SCL-90-R, perceived stress and vulnerability to stress. Beforehand, the psychological variables were tested for normality using the Kolmogorov–Smirnov test and for homoscedasticity using Levene’s test, meeting the assumptions of normality.
The level of statistical significance used was 5% bilateral. For variables where significant differences were found, effect sizes were then calculated using Cohen’s d, using the following values for interpretation: small effect size > 0.20, medium effect size > 0.50 and large effect size > 0.8019.
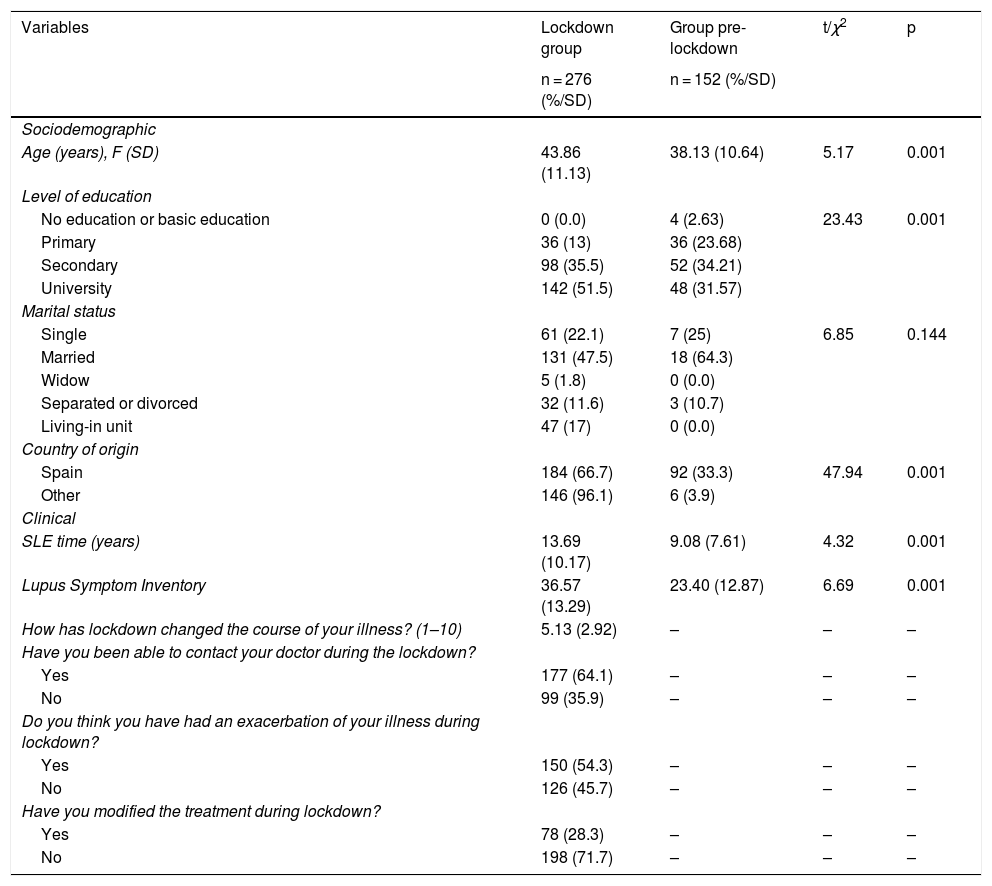
ResultsSample descriptionThe results showed differences between groups in some of the sociodemographic variables such as age, educational level, or country of origin (Table 1). In addition, the time of disease progression and the perception of lupus symptoms were found to be significantly greater in the lockdown group.
Descriptive analysis of the groups in the sociodemographic and clinical variables, using the Student's t and Chi-square comparison tests.
| Variables | Lockdown group | Group pre-lockdown | t/χ2 | p |
|---|---|---|---|---|
| n = 276 (%/SD) | n = 152 (%/SD) | |||
| Sociodemographic | ||||
| Age (years), F (SD) | 43.86 (11.13) | 38.13 (10.64) | 5.17 | 0.001 |
| Level of education | ||||
| No education or basic education | 0 (0.0) | 4 (2.63) | 23.43 | 0.001 |
| Primary | 36 (13) | 36 (23.68) | ||
| Secondary | 98 (35.5) | 52 (34.21) | ||
| University | 142 (51.5) | 48 (31.57) | ||
| Marital status | ||||
| Single | 61 (22.1) | 7 (25) | 6.85 | 0.144 |
| Married | 131 (47.5) | 18 (64.3) | ||
| Widow | 5 (1.8) | 0 (0.0) | ||
| Separated or divorced | 32 (11.6) | 3 (10.7) | ||
| Living-in unit | 47 (17) | 0 (0.0) | ||
| Country of origin | ||||
| Spain | 184 (66.7) | 92 (33.3) | 47.94 | 0.001 |
| Other | 146 (96.1) | 6 (3.9) | ||
| Clinical | ||||
| SLE time (years) | 13.69 (10.17) | 9.08 (7.61) | 4.32 | 0.001 |
| Lupus Symptom Inventory | 36.57 (13.29) | 23.40 (12.87) | 6.69 | 0.001 |
| How has lockdown changed the course of your illness? (1–10) | 5.13 (2.92) | – | – | – |
| Have you been able to contact your doctor during the lockdown? | ||||
| Yes | 177 (64.1) | – | – | – |
| No | 99 (35.9) | – | – | – |
| Do you think you have had an exacerbation of your illness during lockdown? | ||||
| Yes | 150 (54.3) | – | – | – |
| No | 126 (45.7) | – | – | – |
| Have you modified the treatment during lockdown? | ||||
| Yes | 78 (28.3) | – | – | – |
| No | 198 (71.7) | – | – | – |
Regarding the lockdown variables, half of the lockdown group reported having experienced an exacerbation of the disease during the health emergency situation. In addition, 64.1% claimed to have contacted their doctor during lockdown and in 71.7% of the cases they maintained their treatment without changes. On the other hand, both groups were equal in terms of drug treatment with antimalarials, corticosteroids and immunosuppressants.
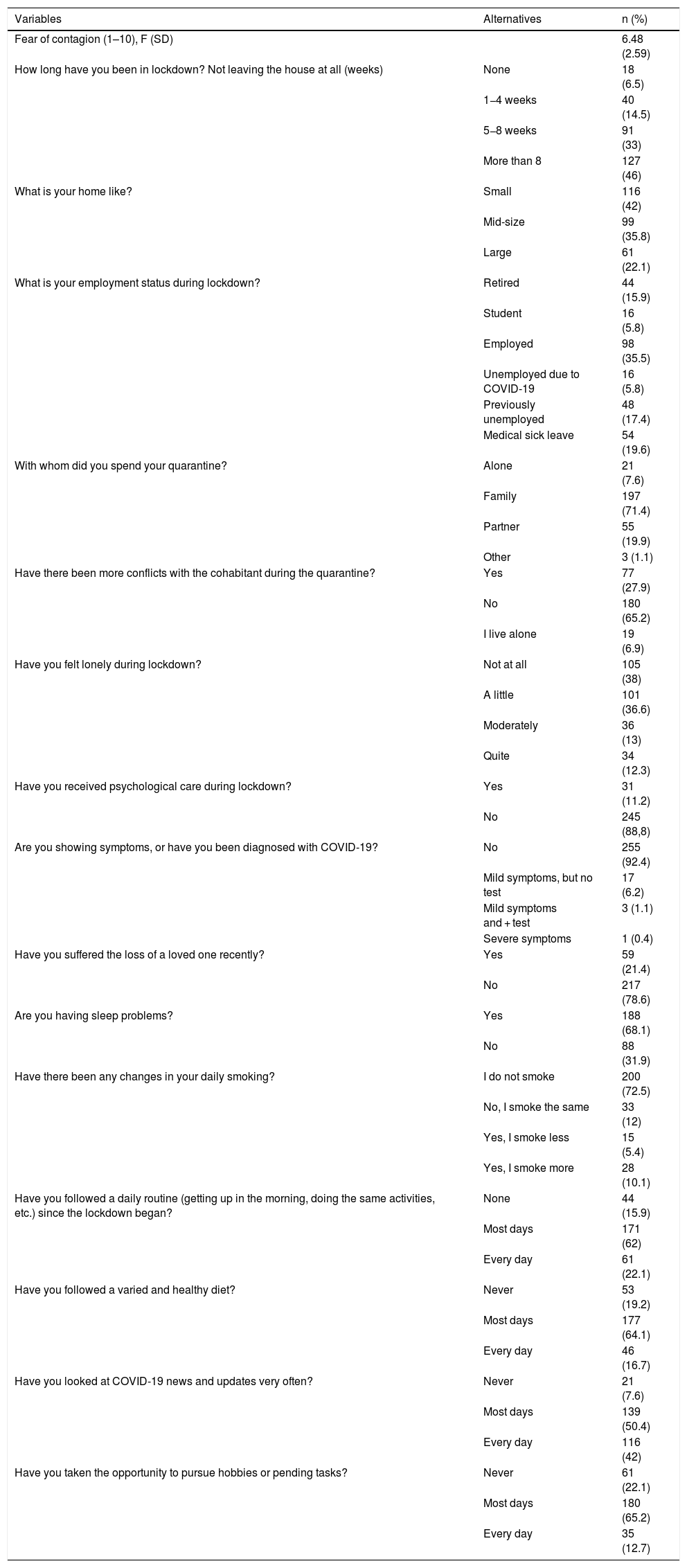
Regarding the variables associated with lockdown, the lockdown group reported that their work situation during this period was characterized by 35% having work activity, while 5.8% had lost their job due to COVID- 19 and 17.4% were unemployed prior to the pandemic (Table 2).
Description of the lockdown-related variables in the lockdown group.
| Variables | Alternatives | n (%) |
|---|---|---|
| Fear of contagion (1–10), F (SD) | 6.48 (2.59) | |
| How long have you been in lockdown? Not leaving the house at all (weeks) | None | 18 (6.5) |
| 1−4 weeks | 40 (14.5) | |
| 5−8 weeks | 91 (33) | |
| More than 8 | 127 (46) | |
| What is your home like? | Small | 116 (42) |
| Mid-size | 99 (35.8) | |
| Large | 61 (22.1) | |
| What is your employment status during lockdown? | Retired | 44 (15.9) |
| Student | 16 (5.8) | |
| Employed | 98 (35.5) | |
| Unemployed due to COVID-19 | 16 (5.8) | |
| Previously unemployed | 48 (17.4) | |
| Medical sick leave | 54 (19.6) | |
| With whom did you spend your quarantine? | Alone | 21 (7.6) |
| Family | 197 (71.4) | |
| Partner | 55 (19.9) | |
| Other | 3 (1.1) | |
| Have there been more conflicts with the cohabitant during the quarantine? | Yes | 77 (27.9) |
| No | 180 (65.2) | |
| I live alone | 19 (6.9) | |
| Have you felt lonely during lockdown? | Not at all | 105 (38) |
| A little | 101 (36.6) | |
| Moderately | 36 (13) | |
| Quite | 34 (12.3) | |
| Have you received psychological care during lockdown? | Yes | 31 (11.2) |
| No | 245 (88,8) | |
| Are you showing symptoms, or have you been diagnosed with COVID-19? | No | 255 (92.4) |
| Mild symptoms, but no test | 17 (6.2) | |
| Mild symptoms and + test | 3 (1.1) | |
| Severe symptoms | 1 (0.4) | |
| Have you suffered the loss of a loved one recently? | Yes | 59 (21.4) |
| No | 217 (78.6) | |
| Are you having sleep problems? | Yes | 188 (68.1) |
| No | 88 (31.9) | |
| Have there been any changes in your daily smoking? | I do not smoke | 200 (72.5) |
| No, I smoke the same | 33 (12) | |
| Yes, I smoke less | 15 (5.4) | |
| Yes, I smoke more | 28 (10.1) | |
| Have you followed a daily routine (getting up in the morning, doing the same activities, etc.) since the lockdown began? | None | 44 (15.9) |
| Most days | 171 (62) | |
| Every day | 61 (22.1) | |
| Have you followed a varied and healthy diet? | Never | 53 (19.2) |
| Most days | 177 (64.1) | |
| Every day | 46 (16.7) | |
| Have you looked at COVID-19 news and updates very often? | Never | 21 (7.6) |
| Most days | 139 (50.4) | |
| Every day | 116 (42) | |
| Have you taken the opportunity to pursue hobbies or pending tasks? | Never | 61 (22.1) |
| Most days | 180 (65.2) | |
| Every day | 35 (12.7) |
On the other hand, they showed a medium-high level of fear of contagion, and 46% of them stated that they had been in lockdown for more than 8 weeks. More than half of the group resided in a large dwelling with their family, with only 27.9% reporting an increase in conflict. Regarding perceived social support, more than half of the group stated that they did not feel alone during lockdown, and only 11.2% received psychological assistance (telephone or online) in this period. A positive COVID-19 diagnosis was only found in 1.1%, and 21.4% of the sample stated that they had lost a loved one due to the pandemic. In reference to lifestyle, 68.1% showed sleep problems, only 10.1% increased smoking, 64.1% maintained a balanced diet, and more than 60% followed a daily routine or pursued their hobbies during most lockdown days. Finally, pandemic news follow up was over 90% of the sample for all or most days.
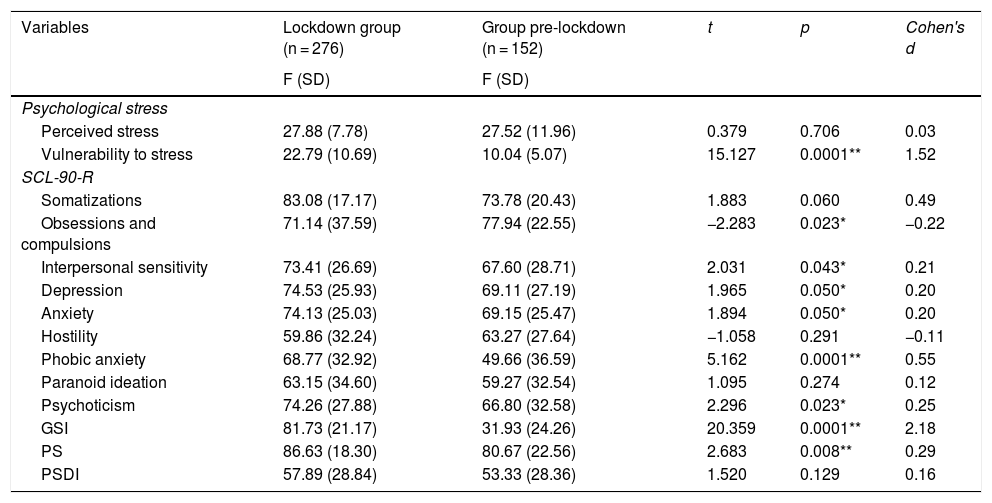
As can be seen in Table 3, the analysis of the differences in stress and psychopathological symptoms between the lockdown group and the pre-lockdown group showed that there were statistically significant differences in vulnerability to stress (p < 0.001), and in the SCL-90-R subdomains: depression (p ≤ 0.05), anxiety (p ≤ 0.05), phobic anxiety (p < 0.001), interpersonal sensitivity (p ≤ 0.043) and psychoticism (p ≤ 0.023), and in the global GSI domains (p < 0.001) and PS (p ≤ 0.008), in which the lockdown group obtained higher scores.
Intergroup differences in stress and psychopathological symptoms.
| Variables | Lockdown group (n = 276) | Group pre-lockdown (n = 152) | t | p | Cohen's d |
|---|---|---|---|---|---|
| F (SD) | F (SD) | ||||
| Psychological stress | |||||
| Perceived stress | 27.88 (7.78) | 27.52 (11.96) | 0.379 | 0.706 | 0.03 |
| Vulnerability to stress | 22.79 (10.69) | 10.04 (5.07) | 15.127 | 0.0001** | 1.52 |
| SCL-90-R | |||||
| Somatizations | 83.08 (17.17) | 73.78 (20.43) | 1.883 | 0.060 | 0.49 |
| Obsessions and compulsions | 71.14 (37.59) | 77.94 (22.55) | −2.283 | 0.023* | −0.22 |
| Interpersonal sensitivity | 73.41 (26.69) | 67.60 (28.71) | 2.031 | 0.043* | 0.21 |
| Depression | 74.53 (25.93) | 69.11 (27.19) | 1.965 | 0.050* | 0.20 |
| Anxiety | 74.13 (25.03) | 69.15 (25.47) | 1.894 | 0.050* | 0.20 |
| Hostility | 59.86 (32.24) | 63.27 (27.64) | −1.058 | 0.291 | −0.11 |
| Phobic anxiety | 68.77 (32.92) | 49.66 (36.59) | 5.162 | 0.0001** | 0.55 |
| Paranoid ideation | 63.15 (34.60) | 59.27 (32.54) | 1.095 | 0.274 | 0.12 |
| Psychoticism | 74.26 (27.88) | 66.80 (32.58) | 2.296 | 0.023* | 0.25 |
| GSI | 81.73 (21.17) | 31.93 (24.26) | 20.359 | 0.0001** | 2.18 |
| PS | 86.63 (18.30) | 80.67 (22.56) | 2.683 | 0.008** | 0.29 |
| PSDI | 57.89 (28.84) | 53.33 (28.36) | 1.520 | 0.129 | 0.16 |
GSI: Global Severity Index; PSDI: positive symptomatic distress index; SCL-90-R: SCL-90-R symptom inventory; PS: total positive symptoms.
In addition, a marginal significance was obtained in the comparison of the somatization’s subdomain (p ≤ 0.06). On the other hand, group 2 showed significantly higher scores in the obsessions/compulsion’s subdomain (p ≤ 0.023).
No statistically significant differences were found for the levels of perceived stress, although these were shown to be high in both groups, exceeding the cut-off point 22.
In Fig. 1 the scores of vulnerability to stress and of the subdomains of the SCL-90-R are presented, where significant differences were found between the 2 groups.
DiscussionThe objective of this study was to analyse the psychological impact of COVID-19 and the lockdown situation on stress levels and psychopathological symptoms of patients with SLE compared to patients with SLE evaluated prior to the pandemic.
The results showed that SLE patients assessed during lockdown had higher levels of psychopathological symptomatology than patients assessed earlier. Specifically, greater depressive symptoms, anxiety, phobic anxiety, interpersonal sensitivity, psychoticism, and somatizations were found, as well as greater vulnerability to stress. However, it is noteworthy that no differences were found in the level of perceived stress during the last month, with both groups being clinically significant.
Previous studies have looked at the psychological consequences of viral outbreaks such as SARS in 2003. The results showed that between 10% and 18% of the sample had psychopathology related to post-traumatic stress disorder, anxiety, and depression. Furthermore, the severity of this psychopathology is associated with a high perception of threat to life and low emotional support20. In this sense, the presence of protective factors against these symptoms of anxiety, stress, or depression, such as stress control and coping tools, would be of high adaptive value to guarantee both physical and psychological quality of life and the prevention of possible exacerbations or worsening of the course of the disease21.
These findings are in line with those of the present study since, during the health emergency period, SLE patients showed higher levels of anxiety and depression than those previously assessed. This increase together with the high levels of interpersonal sensitivity also coincide with the results of studies carried out on the psychological impact of the coronavirus pandemic in a healthy Spanish population22,23.
Therefore, dysphoric mood, nervousness, fears, as well as personal feelings of inadequacy when compared to others, are present during a pandemic situation, in addition to the presence of symptoms of somatisation, phobic anxiety and psychoticism in SLE patients, which have been shown to be higher than in the pre-pandemic group and in the healthy population8. Furthermore, they seem to show greater vulnerability to stress and to suffer psychopathological disorders and, together with the situation of social isolation, could contribute to a decrease in their psychological well-being, as well as a possible worsening of symptoms. In our study, more than half of the patients reported having suffered an exacerbation of the disease during lockdown, an aspect that could be explained by the high levels of stress experienced.
Although the data do not allow these causal relationships to be established, it should be noted that the perception of threat, uncertainty and lack of control associated with the alarm state are factors that trigger the stress response, which has been shown to worsen SLE9. In addition, social isolation due to lockdown may represent another risk factor for patients with SLE, due to its association with systemic inflammation (high levels of C-reactive protein)24.
Lockdown generates increased anxiety in the population25 due to over-information together with fear of contagion and could therefore be influential factors in increasing vulnerability to stress, anxiety, and phobic anxiety, with the phobic object being the virus.
Another factor that could lead to psychological distress during the pandemic would be obstacles to receiving medical care. In our study, however, access to medical care during the pandemic was optimal for 64.1% of the patients.
On the other hand, protective factors for psychological well-being during the pandemic include resilience and emotional support as facilitators of the development of coping mechanisms9. In addition, adherence to recommended isolation policies has also been shown to reduce anxiety caused by the coronavirus26.
Finally, the following limitations must be taken into account. Firstly, the evaluation was carried out during the last month of lockdown, which does not allow us to know the psychological state of the participants at the beginning of the lockdown. Likewise, obtaining other complementary measurements such as cortisol, quality of life index or disease activity would have been of interest. However, access to these variables was not possible due to the health care collapse.
In conclusion, SLE patients have experienced a considerable increase in stress levels and psychopathological symptoms during lockdown, which were already higher than those of the general population. This study has important research and clinical implications, since the results of this study suggest that future research should be directed towards the study of protective factors to reduce these variables. Clinically speaking, it would be essential to design and implement psychological training interventions for effective coping strategies to cushion the psychological impact associated with these situations.
Conflict of interestsNone.
Please cite this article as: Santos-Ruiz A, Montero-López E, Ortego-Centeno N, Peralta-Ramírez MI. Efecto del confinamiento por COVID-19 en el estado mental de pacientes con lupus eritematoso sistémico. Med Clin (Barc). 2021;156:379–385.