Sodium-glucose cotransporter type 2 inhibitors (SGLT2i) are a group of drugs that reduce hyperglycaemia by increasing urinary glucose excretion. In addition to improving glycaemic control, they contribute to a decrease in weight and have beneficial effects on blood pressure.1 The results of the Empagliflozin Cardiovascular Outcome—EMPA-REG-OUTCOME2—study have shown a decrease in cardiovascular events with empagliflozin in diabetic patients with established cardiovascular disease. However, in 2015, the US Food and Drug Administration issued a warning about SGLT2i, evidencing that they could increase the risk of diabetic ketoacidosis (DKA).3 The progressive increase in the use of these drugs and the diagnosis of several cases of euglycemic DKA in our hospital led us to propose a study in which all DKA episodes were collected in patients with diabetes mellitus (DM) 2, with special attention to those treated with SGLT2i.
We performed a retrospective study using our hospital database (MBDS). A total of 119,168 episodes of hospitalization were analyzed between 2010 and the first half of 2016. We identified 151 DKA episodes in a total of 130 patients: 91 with DM1 and 39 with DM2. Six patients were excluded because of lack of key data. Of the 33 patients with DM2 that were finally analyzed, the main characteristics of DKA episodes were collected in the database (SPSS® 22). Of the 33 patients, 20 were men (60.7%) and 13 women (39.3%), with a mean age of 63±11.27 years. The episode ended in death in 8 of the patients (24.2%). The main causes of ketoacidosis were, in order of frequency: infectious (10 cases, 30%), cardiovascular (6 cases, 18%) and others with a wide variety.
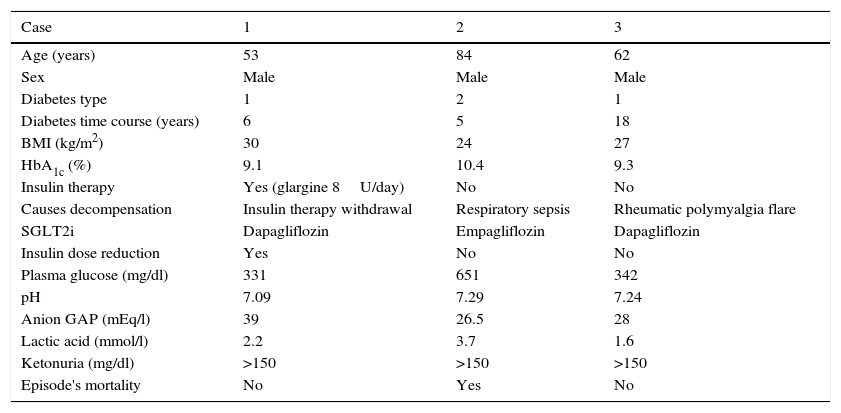
Table 1 summarizes and shows the main characteristics of the 3 patients who developed DKA in treatment with SGLT2i. None of them had previously suffered episodes of DKA or metabolic acidosis. Only one of these patients was included as an episode of DKA in DM2.
Characteristics of diabetic ketoacidosis episodes in patients treated with sodium-glucose cotransporter type 2 inhibitors.
| Case | 1 | 2 | 3 |
|---|---|---|---|
| Age (years) | 53 | 84 | 62 |
| Sex | Male | Male | Male |
| Diabetes type | 1 | 2 | 1 |
| Diabetes time course (years) | 6 | 5 | 18 |
| BMI (kg/m2) | 30 | 24 | 27 |
| HbA1c (%) | 9.1 | 10.4 | 9.3 |
| Insulin therapy | Yes (glargine 8U/day) | No | No |
| Causes decompensation | Insulin therapy withdrawal | Respiratory sepsis | Rheumatic polymyalgia flare |
| SGLT2i | Dapagliflozin | Empagliflozin | Dapagliflozin |
| Insulin dose reduction | Yes | No | No |
| Plasma glucose (mg/dl) | 331 | 651 | 342 |
| pH | 7.09 | 7.29 | 7.24 |
| Anion GAP (mEq/l) | 39 | 26.5 | 28 |
| Lactic acid (mmol/l) | 2.2 | 3.7 | 1.6 |
| Ketonuria (mg/dl) | >150 | >150 | >150 |
| Episode's mortality | No | Yes | No |
DKA is a serious complication of diabetes. Typically, it has been related to DM1; however, it is also present in patients with DM2. Ketosis-prone type 2 diabetes is the name given to DM2 with a propensity to ketosis.4 In our series, we would like to highlight the low mean age of the patients and a high mortality rate, 24.2%. This high mortality should make us reflect on the importance of this disease.
Due to their cardiovascular efficacy and benefits, SGLT2i are used as a second therapeutic step, for example, after metformin, among others. However, the risk of DKA associated with the use of SGLT2i became known in 2015.3 Several pathophysiological mechanisms explain the pathogenesis of DKA. First, the presence of SGLT2 receptors in pancreatic alpha cells has been demonstrated; dapagliflozin induces an increase in the secretion of glucagon in the pancreas. Second, in animal studies, SGLT2i produce an increased renal tubular reabsorption of ketone bodies. Finally, SGLT2i increase fat oxidation and the production of ketone bodies in patients with DM2. These and other mechanisms under study seem to assert that SGLT2i predispose patients to DKA.5 In the clinical cases reported, it is worth highlighting aspects that could favour DKA and its severity: the difficulty of confirming this diagnosis because some patients present borderline blood glucose levels (euglycemic DKA); the presence of stressors or triggers (withdrawal of insulin therapy, infection, inflammation), and finally, DM1 was confirmed in 2 of the cases reported.
It is important to establish which patients with DM2 are most likely to benefit from SGLT2i and to establish which patients are at increased risk of developing DKA. The risk of DKA appears to be increased in the following groups: very elderly, low body mass index, high levels of HbA1c, renal failure or long-term DM2. Likewise, these drugs should be temporarily discontinued in any risk situation that may increase metabolic acidosis. Further research is needed to clarify all these aspects and to properly inform patients.5
Please cite this article as: López Medina JA, Hernández García C, Espíldora Hernández J. Cetoacidosis diabética en pacientes en tratamiento con inhibidores del cotransportador de sodio-glucosa 2. Med Clin (Barc). 2017;149:311–312.