There are few data on the clinical characteristics of COVID-19 patients who require blood transfusion. We aimed to investigate the clinical characteristics and indication for transfusion in COVID-19 patients seen during the epidemic's first wave.
Material and methodsCross-sectional study that included all consecutive COVID-19 patients admitted to the Hospital Clínic of Barcelona, Spain, from mid-March to mid-May 2020.
ResultsA total of 80 patients received 354 RBC units, 116 plasma units, and 48 platelet units. Median age was 71 years (IQR: 62–76), and 59 (74%) were males. In total, 138 of the 261 transfusion episodes that involved RBCs (59%) were related to spontaneous (n=94) or procedure-related (n=44) bleeding. Spontaneous bleeding was more frequent in the retroperitoneal space and the gastrointestinal apparatus. Tracheostomy with endotracheal intubation, surgical interventions, and cannulation of femoral vessels were the main procedures behind non-spontaneous bleeding. Most patients (91%) were on anticoagulants, mostly intermediate- or full-dose heparin.
ConclusionAnticoagulation-related bleeding was a leading cause of blood transfusion in COVID-19 patients during the epidemic's first-wave.
Las características de los pacientes con COVID-19 transfundidos son poco conocidas. Nuestro objetivo fue investigar el perfil clínico y el motivo de la transfusión en los pacientes con COVID-19 vistos durante la primera ola de la epidemia.
Material y métodosEstudio transversal que incluyó a todos los pacientes con COVID-19 transfundidos en el Hospital Clínic de Barcelona entre marzo y mayo de 2020.
ResultadosOchenta pacientes recibieron 354 unidades de hematíes, 116 de plasma y 48 de plaquetas. La edad mediana fue de 71 años y 59 (74%) eran hombres. En total, 138 de los 261 episodios de transfusión de hematíes (59%) estaban relacionados con hemorragia espontánea (n=94: principalmente retroperitoneal y gastrointestinal) o con procedimientos invasivos (n=44: principalmente traqueostomía, cirugía, y canulación de vasos femorales). El 91% de los pacientes recibía tratamiento anticoagulante el día de la transfusión o los dos días previos, sobre todo heparina a dosis intermedia o completa.
ConclusiónEl sangrado relacionado con la anticoagulación fue el motivo principal de transfusión en los pacientes con COVID-19.
The ongoing pandemic of COVID-19 is severely challenging healthcare systems all around the world. With regard to blood transfusion, studies have documented a decrease in blood collection because of fear of infection and social distancing policies, and a concomitant reduction in transfusion driven by the brutal change in the case-mix of admitted patients.1–3 Notably, little has been published about the clinical characteristics of COVID-19 patients who require blood transfusion.
The present study aimed to describe blood usage by COVID-19 patients during the first epidemic wave, with a particular emphasis on the clinical features of transfused patients and the indication for transfusion.
Patients and methodsFor this cross-sectional study, we reviewed the blood bank and electronic clinical records of 80 consecutive patients diagnosed with COVID-19, who required red blood cells (RBC) transfusion at the Hospital Clínic of Barcelona over 60 days, from mid-March to mid-May 2020. The period on study ranged from the date the first patient was transfused to the date when a week had elapsed without new transfusions to COVID-19 patients. COVID-19 was confirmed by at least two PCR test in nasopharyngeal swaps. Categorical data were described as frequencies and percentages, and continuous variables were summarized as the median and interquartile range (IQR). Written informed consent was obtained from each patient, and the study protocol conforms to the ethical guidelines of the 1975 Declaration of Helsinki, as reflected in a priori approval by the Ethics Committee of our institution (code: HCB.2020.0541).
ResultsIn total, 80 patients received 354 RBC units in 261 independent transfusion episodes. The number of days on transfusion support ranged from 1 to 44 (median: 5). In addition, 116 units of fresh-frozen plasma (FFP) were transfused to 14 of these 80 patients (including two patients on therapeutic plasma exchange who received 32 and 35 units, respectively), and 48 platelet units, to 11 patients. Among these later 11 patients, nine receive platelets because of thrombocytopenia and spontaneous or procedure-related haemorrhage, two were on extracorporeal membrane oxygenation (ECMO), and 2 were on prophylactic regime because of concomitant hematologic malignancies and chemotherapy.
Median age of the 80 patients was 71 years (IQR: 62–76), and 59 (74%) were male. Table 1 summarizes the patients’ main clinical characteristics and the indications for transfusion. Distribution of ABO group was not significantly different from that observed in transfused non-COVID-19 patients during the same period (Table 2).
Characteristics of 80 patients with COVID-19 who required red blood cell transfusion. Laboratory data were obtained at the time of first transfusion.
| Age, yrsa | 71 (62–76) |
| Sex, males/females | 59 (74%)/21 (26%) |
| Prior transfusion | 12 (15%) |
| Reason for admission | |
| Pneumonia | 75 (94%) |
| Otherb | 5 (6%) |
| No. blood units transfused per patient, median (range) | 5 (1–30) |
| Laboratory data at first transfusion | |
| Hb, mg/dla | 7.6 (7.2–8.3) |
| Ferritin, μg/mla | 938 (567–1534) |
| D-dimer, cg/mla | 2800 (1200–4800) |
| Indication for transfusionc | |
| Large haematoma | 22 (27%) |
| Retroperitoneal | 11 |
| Femoral | 4 |
| Cerebral | 1 |
| Thoracic and abdominal wall | 2 |
| Posterior calf | 2 |
| Other locations | 2 |
| Haemorrhage | 31 (39%) |
| Gastrointestinal | 11 |
| Related to tracheostomy/endotracheal intubation | 8 |
| Pulmonary | 3 |
| Surgery-related | 4 |
| Epistaxis or gingivorrhagia | 3 |
| Other anatomical locations | 2 |
| Anaemia of critical illness | 22 (27%) |
| Anaemia of neoplasia | 5 |
| ECMOd | 2 |
| Other causes of anaemia | 10 |
| Anticoagulatione | |
| None | 7 (9%) |
| Low- or intermediate dose¶ | 31 (39) |
| Full anticoagulant dosef | 42 (52%) |
Blood group distribution in COVID-19 patients transfused at the Hospital Clínic of Barcelona between 15 March and 15 May, 2020, as compared to non COVID-19 patients transfused during the same period.
| Blood group | COVID-19No. (%) | Non COVID-19No. (%) |
|---|---|---|
| O | 30 (37.5) | 860 (45.3) |
| A | 38 (47.5) | 827 (43.5) |
| B | 11 (13.7) | 132 (7) |
| AB | 1 (1.3) | 80 (4.2) |
p=0.11.
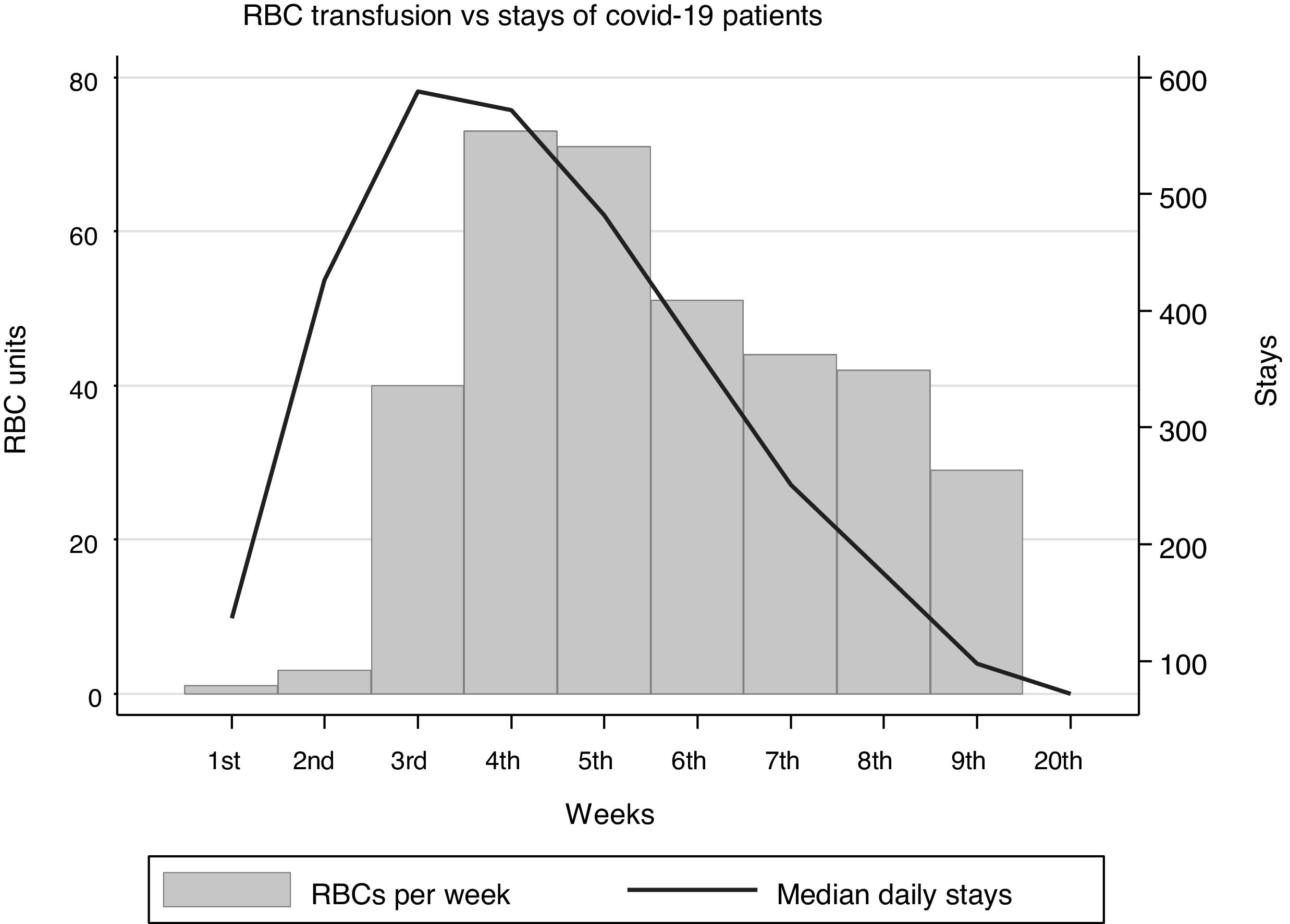
Fig. 1 shows the RBC usage per in-hospital stay of COVID-19 patients. In summary, 1.7 RBC units were transfused per 100 patient-days. As compared with the same period of 2019, RBC usage during the 60 days on study decreased from 4152 to 3006 units (30% reduction), FFP decreased from 847 to 735 units, and platelets, from 930 to 736 units.
Bleeding was the indication for transfusion in 53 patients (66%) and included either large hematomas in 22 and external haemorrhage in 31. Anaemia of critical illness was the reason for transfusion in 22 (27%) patients. Most patients were on anticoagulants at the time of transfusion or the two days before (Table 1). In total, 138 of the 261 transfusion episodes (59%) were related to spontaneous (n=94) or procedure-related (n=44) bleeding. Spontaneous bleeding was more frequent in the retroperitoneal space and the gastrointestinal apparatus. Tracheostomy with endotracheal intubation, surgical interventions, and cannulation of femoral vessels were the main procedures behind non-spontaneous bleeding. Frequency of blood group O was similar in patients transfused because of bleeding or other reasons (20 of 53 [38%] and 10 of 27 [37%], respectively).
Seventeen patients died during the study period, and eight additional patients died in hospital after the study's closing date on May 15th. None of the deaths was ascribed to haemorrhage or blood transfusion. All the surviving patients were eventually discharged home or transferred to rehabilitation centres.
DiscussionThe present study shows that bleeding, mostly related to anticoagulants, was the main indication for RBC transfusion in patients with COVID-19. Few previous reports are available to contrast this finding. In a small series from South Chorea at the beginning of the epidemics, only two of nine transfused patients were on anticoagulants.3 In the report by Pagano et al.,4 on 13 COVID-19 patients transfused in Seattle between late February and early April, indications consisted of pre-existing comorbidities and anaemia of chronic disease, without any specific mention to haemorrhage or anticoagulants. Later studies found that RBC transfusion was more prevalent in patients on anticoagulants but did not provide clinical details about transfusion indications.5
The poor prognostic significance of hypercoagulability markers in COVID-19, and the beneficial effect of heparin treatment, often guided by serum D-dimer levels, were progressively recognized over the first months of the SARS-CoV-2 epidemic.6,7 Therefore, it is not rare that early reports did not find bleeding associated with anticoagulants as an indication for blood transfusion in COVID-19 patients.
Changes in the indications for blood transfusion throughout the epidemic, and differences in the crowding-out of the usual inpatient case-mix by the massive admission of COVID-19 patients, preclude any sound comparison of blood usage among hospitals. Variability among centres in the use of ECMO can also contribute to differences in blood usage because ECMO has been associated with increased need for RBC transfusion.8 Despite this difficulty, our results are consistent with previous studies reporting a reduced overall demand for transfusion during the SARS-CoV-2 epidemic.5,8,9 We relied on patient stays instead of admissions as a yardstick to measure transfusion intensity in COVID-19 patients because it was more appropriate to the bounded period on study.
We were astonished by the high prevalence of retroperitoneal haematoma as a cause for RBC transfusion in our patients, a complication that was often difficult to diagnose, as revealed by the medical records. In a series of 89 patients with spontaneous retroperitoneal haematoma, 85% were on anticoagulant or antiplatelet medications, and pain referred to the abdomen, hip or flank was the leading complaint.10
In our series, haemorrhage was often protracted and difficult to control, and transfusion support extended for several days. Not rarely, haemorrhage recurred when the patient was restarted on anticoagulants, and it was not unusual for bleeding from an anatomical location to be followed by and overlapped with bleeding from a different location.
Our study has some limitations. First, results derived from a single centre during the learning curve of how to manage the severe complications of COVID-19, so that they may not apply to other centres or situations. Second, we did not investigate whether transfusion was a surrogate for worse prognosis in COVID-19, as we did not compare transfused and non-transfused patients. Third, the study was focused on transfused patients and did not allow to draw any quantitative conclusion on the risk of bleeding associated with the use of anticoagulants in COVID-19, which would require a different study design. Third, despite the above limitations, our results point at anticoagulation-related bleeding as a leading cause for blood transfusion in COVID-19 patients.
ConclusionBleeding, mostly related to the use of anticoagulants, was the main indication for RBC transfusion in patients with COVID-19.
Authors’ contributionsAll authors have made substantial contributions to all of the following: (1) the conception and design of the study, or acquisition of data, or analysis and interpretation of data, (2) drafting the article or revising it critically for important intellectual content, and (3) final approval of the version to be submitted.
Conflicts of interestNone declared.