During the first months of the SARS-CoV-2 pandemic, several studies cautioned about the high prevalence of hypertension among patients admitted for COVID-19 and associated it with a worse clinical course.1 Some research speculated that drugs inhibiting the renin-angiotensin-aldosterone system might increase susceptibility to infection, suggesting that they might up-regulate SARS-CoV-2 cell receptors, thereby aiding viral replication.2 This raised concerns and led initially to a heterogeneous management of this pathology, as well as frequent changes in standard drug treatment, which forced the main scientific societies to position themselves.3
The present study was conducted to adequately quantify the prescribing and deprescribing rate of the different antihypertensive drugs and their long-term cardiovascular impact, in which total mortality and the incidence of the combined endpoint of major cardiovascular events was defined as the outcome variable, defined as acute coronary syndrome (ACS), cerebrovascular accident (CVA), venous thromboembolic events (VTE), development of heart failure (HF) and cardiovascular mortality.
This is an observational and prospective study in which consecutive patients admitted for respiratory infection and positive polymerase chain reaction (PCR) between 1 March and 30 April 2020 at the Hospital General Universitario de Ciudad Real were analysed. In the period under analysis, 921 patients were registered, of whom 673 patients were discharged; among them 359 were patients with a diagnosis of hypertension and drug therapy. They were monitored over a period of time from discharge to data analysis, with an average of 352±70.4 days.
50.7% were male, the mean age was 74.4±12.9 years. 28.7% were diabetic patients, 49% were dyslipidemic, 17.8% were smokers, and 19.8% were obese. 13.4% of the patients analysed had a previous diagnosis of ischemic heart disease, a similar percentage, 13.1% heart failure, and 13.6% atrial fibrillation.
ACEIs (angiotensin converting enzyme inhibitors), ARBs (angiotensin II receptor blockers), calcium channel blockers, thiazide diuretics, loop diuretics, aldosterone antagonists, beta-blockers, and alpha-blockers were analysed as antihypertensive drugs. At discharge, 75.8% of the patients maintained the antihypertensive treatment, being modified in the remaining 24.2%. Prior to admission, 77.2% were taking ACEIs or ARBs; however, in 16.4% of the patients they were discontinued after admission. In contrast, treatment with calcium channel blockers increased from 27.6% to 34.1% after hospitalization. In both cases, there were statistically significant differences in the bivariate analysis in the McNemar test (p < 0.05 in both cases), with no differences being observed in the rest of the antihypertensives analysed.
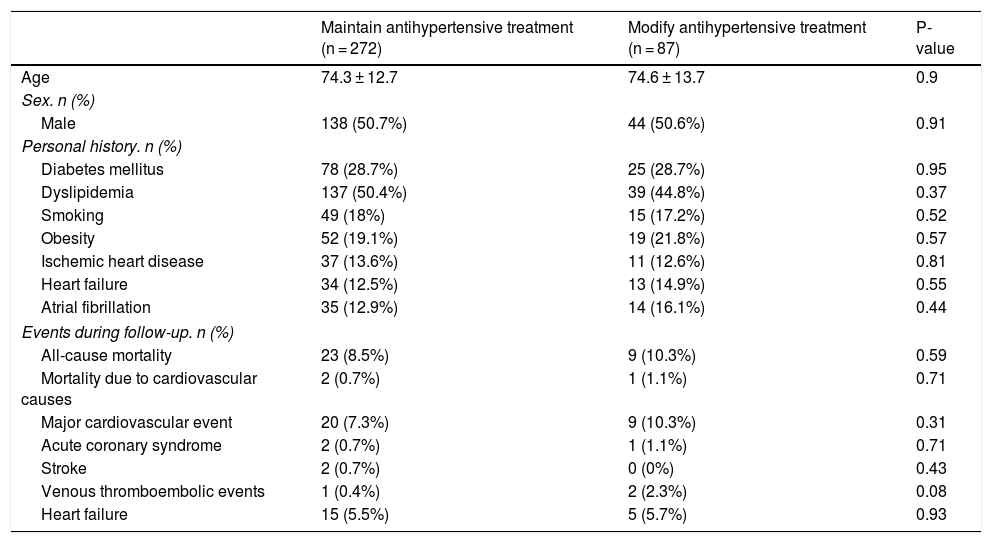
After follow-up, the combined event occurred in 28 patients, with the development of HF being the most common event, while only 0.8% developed ACS. Overall mortality was 8.9%. Table 1 shows the events recorded according to the change of antihypertensive treatment and the maintenance or discontinuation of ACEIs/ARBs in those who were already taking it on admission. Similarly, a survival analysis was performed in which no differences were observed in terms of all-cause mortality or major cardiovascular events between patients who maintained their antihypertensive treatment versus those who modified it. Likewise, maintaining or discontinuing ACEIs/ARBs treatment did not influence mortality or the occurrence of major cardiovascular events.
Comparison of baseline clinical characteristics, mortality and major cardiovascular events according to changes in antihypertensive treatment.
| Maintain antihypertensive treatment (n = 272) | Modify antihypertensive treatment (n = 87) | P-value | |
|---|---|---|---|
| Age | 74.3 ± 12.7 | 74.6 ± 13.7 | 0.9 |
| Sex. n (%) | |||
| Male | 138 (50.7%) | 44 (50.6%) | 0.91 |
| Personal history. n (%) | |||
| Diabetes mellitus | 78 (28.7%) | 25 (28.7%) | 0.95 |
| Dyslipidemia | 137 (50.4%) | 39 (44.8%) | 0.37 |
| Smoking | 49 (18%) | 15 (17.2%) | 0.52 |
| Obesity | 52 (19.1%) | 19 (21.8%) | 0.57 |
| Ischemic heart disease | 37 (13.6%) | 11 (12.6%) | 0.81 |
| Heart failure | 34 (12.5%) | 13 (14.9%) | 0.55 |
| Atrial fibrillation | 35 (12.9%) | 14 (16.1%) | 0.44 |
| Events during follow-up. n (%) | |||
| All-cause mortality | 23 (8.5%) | 9 (10.3%) | 0.59 |
| Mortality due to cardiovascular causes | 2 (0.7%) | 1 (1.1%) | 0.71 |
| Major cardiovascular event | 20 (7.3%) | 9 (10.3%) | 0.31 |
| Acute coronary syndrome | 2 (0.7%) | 1 (1.1%) | 0.71 |
| Stroke | 2 (0.7%) | 0 (0%) | 0.43 |
| Venous thromboembolic events | 1 (0.4%) | 2 (2.3%) | 0.08 |
| Heart failure | 15 (5.5%) | 5 (5.7%) | 0.93 |
| Maintain ACEIs/ARBs (n = 221) | Discontinue ACEIs/ARBs (n = 56) | P-value | |
|---|---|---|---|
| Age | 74.2 ± 11.9 | 72.4 ± 13.5 | 0.13 |
| Sex. n (%) | |||
| Male | 109 (49.3%) | 31 (55.4%) | 0.4 |
| Personal history. n (%) | |||
| Diabetes mellitus | 72 (36.6%) | 15 (26.8%) | 0.4 |
| Dyslipidemia | 114 (51.6%) | 21 (37.5%) | 0.06 |
| Smoking | 38 (17.1%) | 8 (14.3%) | 0.52 |
| Obesity | 44 (19.9%) | 14 (25%) | 0.4 |
| Ischemic heart disease | 34 (15.4%) | 4 (7.1%) | 0.11 |
| Heart failure | 29 (13.1%) | 2 (3.6%) | 0.04 |
| Atrial fibrillation | 28 (12.7%) | 6 (10.7%) | 0.33 |
| Events during follow-up. n (%) | |||
| All-cause mortality | 14 (6.3%) | 7 (4.1%) | 0.8 |
| Mortality due to cardiovascular causes | 2 (0.9%) | 0 (0%) | 0.47 |
| Major cardiovascular event | 13 (5.4%) | 4 (7.1%) | 0.62 |
| Acute coronary syndrome | 1 (0.5%) | 1 (1.8%) | 0.29 |
| Stroke | 0 (0%) | 0 (0%) | |
| Venous thromboembolic events | 1 (0.5%) | 2 (3.6%) | 0.04 |
| Heart failure | 9 (4.1%) | 1 (1.8%) | 0.41 |
Mortality and major cardiovascular events during follow-up according to changes in antihypertensive treatment.
Qualitative bivariate Chi-square test. In bold, statistically significant results.
There is now consistent evidence that the use of antihypertensive drugs is not associated with the risk and severity of COVID-19. Similarly, the current available literature does not recommend abstaining from the use of these drugs.4,5 Our study shows how the initial uncertainty about the role of hypertension and its treatment led to a major change in antihypertensive treatment, mainly at the cost of discontinuation of ACEIs or ARBs. Although it shows a neutral effect on the development of major cardiovascular events and mortality during follow-up, the observational and single-centre nature of the study, together with limitations such as the small sample size, may make its interpretation difficult and may mask the true impact of the erratic initial management of a condition as common as hypertension.
FundingNo funding has been received for this study.
Conflict of interestsThe authors of this document declare the absence of any conflict of interest related to the publication of this paper.
Please cite this article as: Águila Gordo D, Martínez del Rio J, Piqueras Flores J. Cambios en el tratamiento antihipertensivo de pacientes supervivientes a infección respiratoria por SARS-CoV-2 y su repercusión cardiovascular tras un año de seguimiento. Med Clin (Barc). 2022;158:196–197.