Has been described the loss of smell and taste as onset symptoms in SARS-CoV-2. The objective of this study was to investigate the prevalence in Spain.
MethodsProspective study of COVID-19 confirmed patients through RT-PCR in Spain. Patients completed olfactory and gustatory questionnaires.
ResultsA total of 1043 patients with mild COVID-19 disease. The mean age was 39 ± 12 years. 826 patients (79.2%) described smell disorder, 662 (63.4%) as a total loss and 164 (15.7%) partial. 718 patients (68.8%) noticed some grade of taste dysfunction. There was a significant association between both disorders (p < 0.001). The olfactory dysfunction was the first symptom in 17.1%. The sQOD-NS scores were significantly lower in patients with a total loss compare to normosmic or hyposmic individuals (p = 0.001). Female were significantly more affected by olfactory and gustatory dysfunctions (p < 0.001). The early olfactory recover in 462 clinically cured patients was 315 (68.2%), during the first 4 weeks.
ConclusionThe sudden onset smell and/or taste dysfunction should be considered highly suspicious for COVID-19 infection.
En la infección por SARS-CoV-2 la pérdida repentina del olfato y/o gusto han sido descritas como síntomas iniciales. El objetivo principal de este estudio es conocer la prevalencia de estos síntomas en España.
Materiales y métodosEstudio prospectivo de pacientes con COVID-19 confirmado mediante RT-PCR en España. Se utilizaron los cuestionarios traducidos y validados.
ResultadosUn total de 1043 pacientes COVID-19 leve. Edad media de 39 ± 12 años. 826 pacientes (79,2%) refirieron algún grado de alteración del olfato, 662 (63,4%) pérdida total y 164 (15,7%) parcial. 718 pacientes (68,8%) notaron alteración del gusto. Hubo una asociación significativa entre ambos trastornos (p < 0,001). La disfunción olfatoria fue el síntoma inicial en el 17,1%. Las puntuaciones del sQOD-NS fueron significativamente menores en pacientes con una alteración total. Ambas alteraciones fueron proporcionalmente mayores en las mujeres (p < 0,001). De 462 pacientes clínicamente curados 315 (68,2%) recuperaron el olfato dentro de las primeras 4 semanas.
ConclusionesLa alteración repentina del olfato y el gusto debería ser reconocida como un síntoma de alarma de posible infección por COVID-19.
The clinical presentation of patients affected by COVID-19 in a mild-moderate way has consisted mainly of cough (46.6-83.3%), asthenia (63.3-72.9%), headache (60-71 %), anosmia (51.5-70.2%), nasal obstruction (58.6-67.8%) and taste dysfunctions (47.1-67.8%).1–3 Furthermore, the presence of comorbidities such as arterial hypertension, advanced age and obesity have been associated with a worse progression.
The main objective of this study was to investigate the prevalence of subjective smell (SSD) and taste (STD) dysfunction in patients with mild-moderate SARS-CoV-2 infection. The secondary objectives focused on evaluating the impact on quality of life resulting from these dysfunctions and the rate of recovery of both senses.
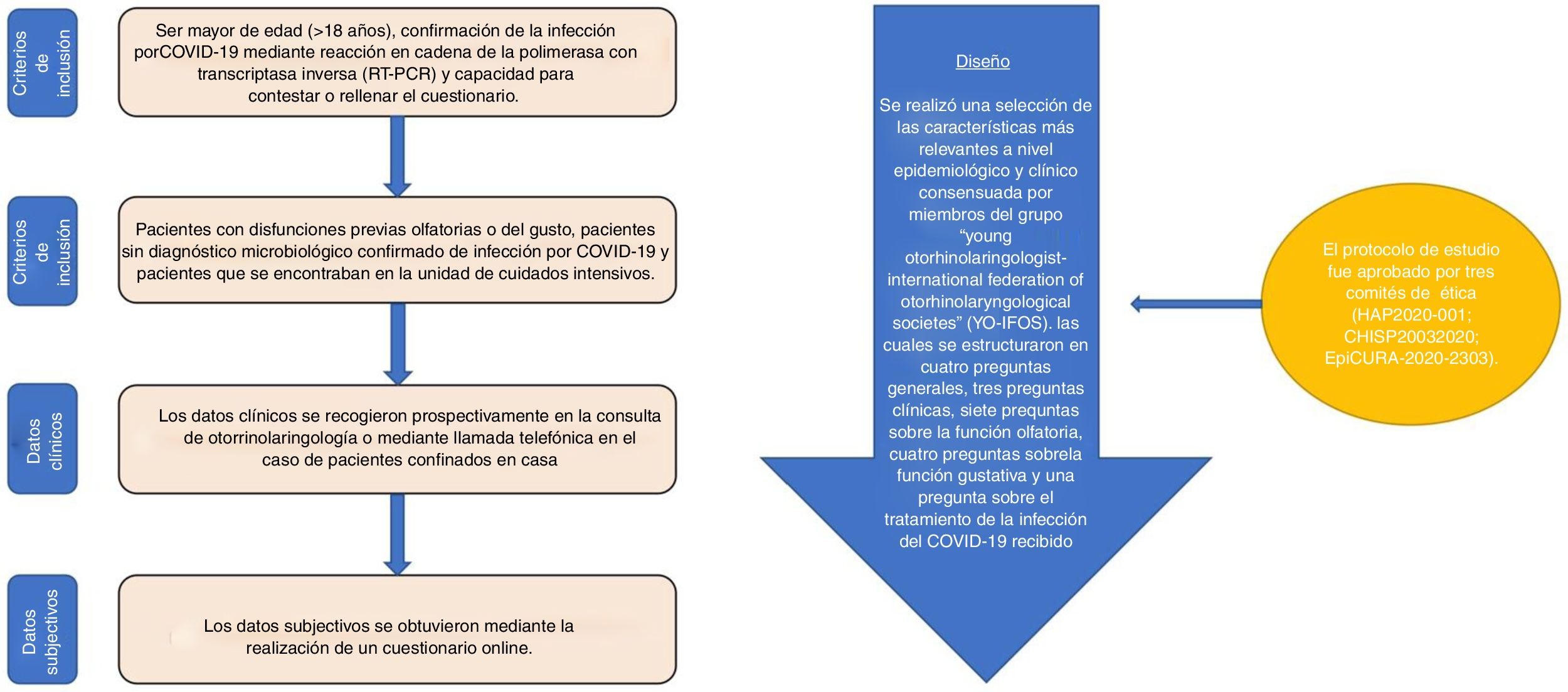
Patients and methodsThis is a prospective study in which the patients included with mild-moderate COVID-19 responded to a questionnaire designed for the analysis of smell and/or taste dysfunction.
The inclusion and exclusion criteria used, as well as the clinical and/or subjective data, were obtained by completing an on-line questionnaire. These, as well as the study design are shown in Fig. 1Fig. 1. All patients were asked to complete a short version of the olfactory dysfunction questionnaire (sQOD-NS).4 The rest of the questions about smell and taste were obtained from the North American National Health and Nutrition questionnaire.5
The mean recovery of the sense of smell was evaluated between the days: 1–4; 5–8; 9–14 and >15. Referring to the studies that have shown that viral load drops significantly 14 days after the onset of symptoms.6
The Statistical Package for the Social Sciences (SPSS version 21.0; IBM Corp, Armonk, NY, USA) software was used to perform the statistical analyses. The normality contrast between the continuous variables was performed using the Shapiro-Wilk test. Potential associations between epidemiological, clinical, olfactory, and taste outcomes were evaluated by cross-tabulation between two variables (dichotomous or categorical variables) and the chi-square test. Incomplete responses were excluded from the analysis. Differences in the sQOD-NS in terms of olfactory dysfunctions between patients were analysed using the Kruskal-Wallis test. A multivariate logistic regression model was applied to estimate the association between smell and taste dysfunction with a group of independent variables (age, sex, symptoms, comorbidities). A value of p< 0.05 was determined to be statistically significant.
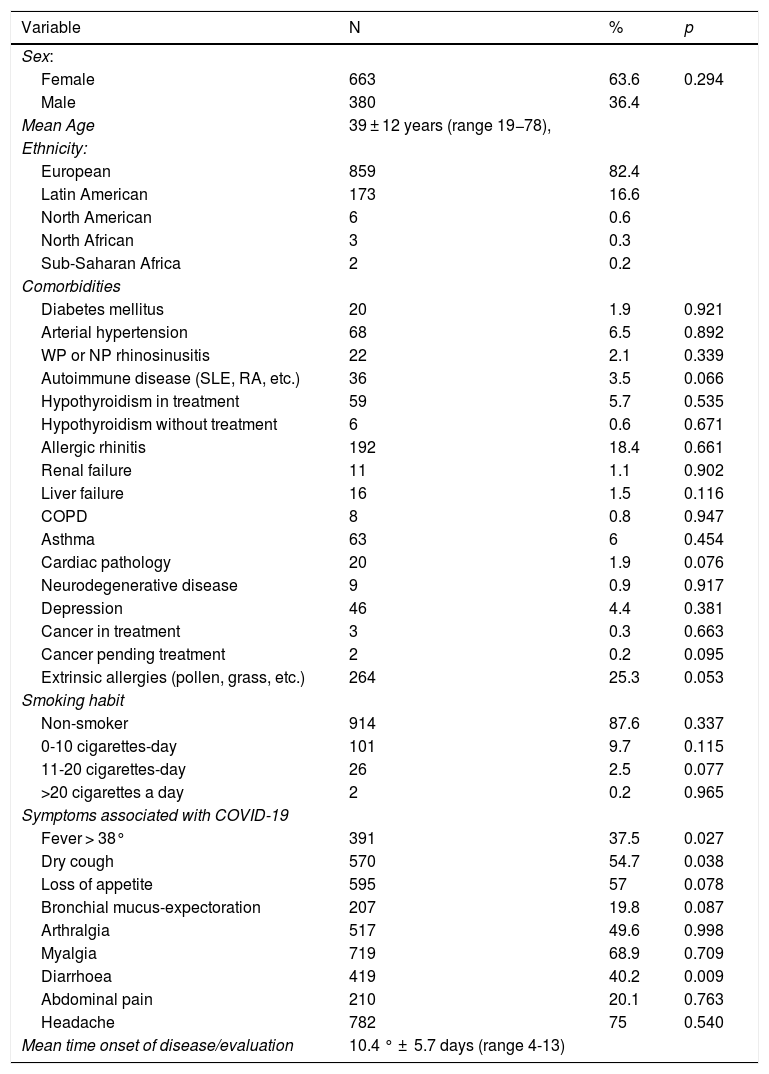
ResultsOf the total 1411 patients with positive RT-PCR for COVID-19 infection, 1043 patients completed the study. Regarding sex, 663 (63.6%) were women and 380 (36.4%) were men. The mean age was 39 ± 12 years (range 19−78). The most common comorbidities are listed in Table 1, Table 1. 42% of the patients were in the acute phase of the infection.
Clinical and demographic variables.
| Variable | N | % | p |
|---|---|---|---|
| Sex: | |||
| Female | 663 | 63.6 | 0.294 |
| Male | 380 | 36.4 | |
| Mean Age | 39 ± 12 years (range 19−78), | ||
| Ethnicity: | |||
| European | 859 | 82.4 | |
| Latin American | 173 | 16.6 | |
| North American | 6 | 0.6 | |
| North African | 3 | 0.3 | |
| Sub-Saharan Africa | 2 | 0.2 | |
| Comorbidities | |||
| Diabetes mellitus | 20 | 1.9 | 0.921 |
| Arterial hypertension | 68 | 6.5 | 0.892 |
| WP or NP rhinosinusitis | 22 | 2.1 | 0.339 |
| Autoimmune disease (SLE, RA, etc.) | 36 | 3.5 | 0.066 |
| Hypothyroidism in treatment | 59 | 5.7 | 0.535 |
| Hypothyroidism without treatment | 6 | 0.6 | 0.671 |
| Allergic rhinitis | 192 | 18.4 | 0.661 |
| Renal failure | 11 | 1.1 | 0.902 |
| Liver failure | 16 | 1.5 | 0.116 |
| COPD | 8 | 0.8 | 0.947 |
| Asthma | 63 | 6 | 0.454 |
| Cardiac pathology | 20 | 1.9 | 0.076 |
| Neurodegenerative disease | 9 | 0.9 | 0.917 |
| Depression | 46 | 4.4 | 0.381 |
| Cancer in treatment | 3 | 0.3 | 0.663 |
| Cancer pending treatment | 2 | 0.2 | 0.095 |
| Extrinsic allergies (pollen, grass, etc.) | 264 | 25.3 | 0.053 |
| Smoking habit | |||
| Non-smoker | 914 | 87.6 | 0.337 |
| 0-10 cigarettes-day | 101 | 9.7 | 0.115 |
| 11-20 cigarettes-day | 26 | 2.5 | 0.077 |
| >20 cigarettes a day | 2 | 0.2 | 0.965 |
| Symptoms associated with COVID-19 | |||
| Fever > 38° | 391 | 37.5 | 0.027 |
| Dry cough | 570 | 54.7 | 0.038 |
| Loss of appetite | 595 | 57 | 0.078 |
| Bronchial mucus-expectoration | 207 | 19.8 | 0.087 |
| Arthralgia | 517 | 49.6 | 0.998 |
| Myalgia | 719 | 68.9 | 0.709 |
| Diarrhoea | 419 | 40.2 | 0.009 |
| Abdominal pain | 210 | 20.1 | 0.763 |
| Headache | 782 | 75 | 0.540 |
| Mean time onset of disease/evaluation | 10.4 ° ± 5.7 days (range 4-13) | ||
RA : rheumatoid arthritis; WP : with polyps; COPD : chronic obstructive pulmonary disease; SLE : systemic lupus erythematosus; NP : without polyps.
Regarding SSD, 826 patients (79.2%) described some type of loss related to the infection. Of these, 662 described their dysfunction as total and 164 as partial. Furthermore, 16.6% associated changes suggestive of dysosmia, and 18.2% phantosmia. SSD appeared before (17.1%), after (47.8%) or at the same time as the rest of the general and/or otolaryngological symptoms (23.9%).
The recovery rate of smell evaluated in 462 cured patients after 4 weeks revealed that 315 (68.2%) showed a partial or total recovery. 57.5% recovered olfactory function in the first 7 days after the resolution of the disease with an overall mean of 9 ± 6 days (range 5–29).
Regarding the impact of SSD on quality of life, patients who perceived a total loss of smell had a significantly lower score (sQOD-NS) compared to those individuals with a partial loss (p = 0.001) or who did not notice any dysfunction of smell (p = 0.001) (Appendix B supplementary material).
Regarding STD, 718 patients (68.8%) reported taste disorders. STD consisted of a reduced (48%) or distorted (22.9%) ability to perceive flavours. Of the 286 patients without taste dysfunction, 52 (5%) did not have olfactory dysfunction, while 194 (18.6%) had a total dysfunction of smell and 40 (3.8%) a partial one.
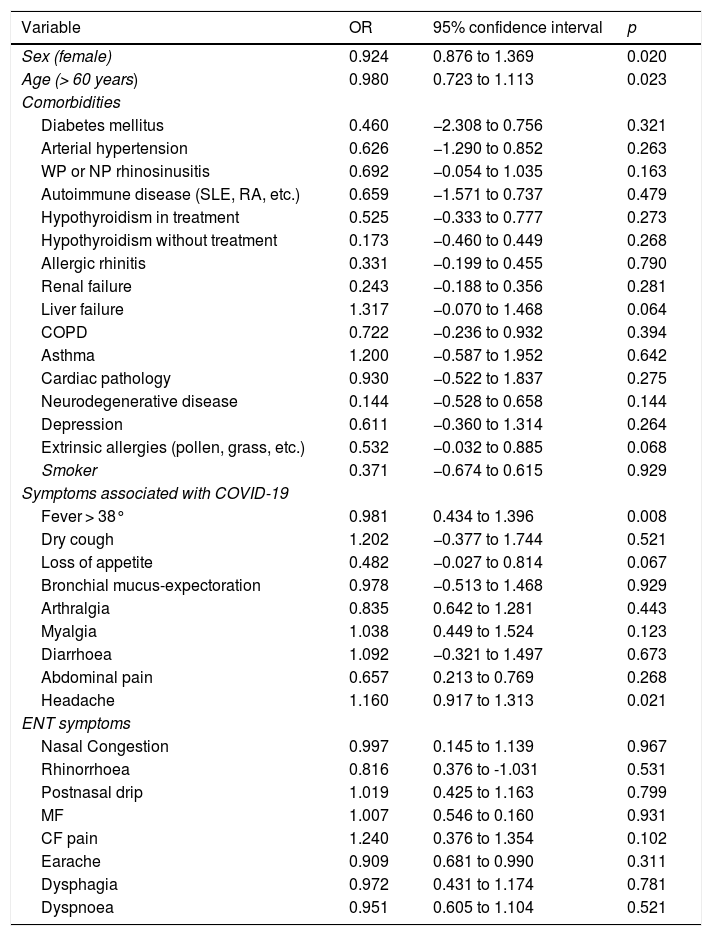
Multivariate analysis showed that women (OR = 0.924; 95% CI: 0.876–1.69) or those over 60 years of age (OR = 0.980; 95% CI: 0.723–1.113) had a higher risk of suffering from SSD or STD. In addition, a significant correlation between the presence of fever (OR = 0.981; 95% CI: 0.434–1.396) or headache (OR = 1,160; 95% CI: 0.917–1.313) and SSD or STD was observed. While we did not find a correlation between otolaryngological symptoms and the presence of comorbidities with the occurrence of sensory dysfunctions (Table 2).
Multivariate analysis of characteristics associated with loss of smell and taste in patients affected by COVID-19.
| Variable | OR | 95% confidence interval | p |
|---|---|---|---|
| Sex (female) | 0.924 | 0.876 to 1.369 | 0.020 |
| Age (> 60 years) | 0.980 | 0.723 to 1.113 | 0.023 |
| Comorbidities | |||
| Diabetes mellitus | 0.460 | −2.308 to 0.756 | 0.321 |
| Arterial hypertension | 0.626 | −1.290 to 0.852 | 0.263 |
| WP or NP rhinosinusitis | 0.692 | −0.054 to 1.035 | 0.163 |
| Autoimmune disease (SLE, RA, etc.) | 0.659 | −1.571 to 0.737 | 0.479 |
| Hypothyroidism in treatment | 0.525 | −0.333 to 0.777 | 0.273 |
| Hypothyroidism without treatment | 0.173 | −0.460 to 0.449 | 0.268 |
| Allergic rhinitis | 0.331 | −0.199 to 0.455 | 0.790 |
| Renal failure | 0.243 | −0.188 to 0.356 | 0.281 |
| Liver failure | 1.317 | −0.070 to 1.468 | 0.064 |
| COPD | 0.722 | −0.236 to 0.932 | 0.394 |
| Asthma | 1.200 | −0.587 to 1.952 | 0.642 |
| Cardiac pathology | 0.930 | −0.522 to 1.837 | 0.275 |
| Neurodegenerative disease | 0.144 | −0.528 to 0.658 | 0.144 |
| Depression | 0.611 | −0.360 to 1.314 | 0.264 |
| Extrinsic allergies (pollen, grass, etc.) | 0.532 | −0.032 to 0.885 | 0.068 |
| Smoker | 0.371 | −0.674 to 0.615 | 0.929 |
| Symptoms associated with COVID-19 | |||
| Fever > 38° | 0.981 | 0.434 to 1.396 | 0.008 |
| Dry cough | 1.202 | −0.377 to 1.744 | 0.521 |
| Loss of appetite | 0.482 | −0.027 to 0.814 | 0.067 |
| Bronchial mucus-expectoration | 0.978 | −0.513 to 1.468 | 0.929 |
| Arthralgia | 0.835 | 0.642 to 1.281 | 0.443 |
| Myalgia | 1.038 | 0.449 to 1.524 | 0.123 |
| Diarrhoea | 1.092 | −0.321 to 1.497 | 0.673 |
| Abdominal pain | 0.657 | 0.213 to 0.769 | 0.268 |
| Headache | 1.160 | 0.917 to 1.313 | 0.021 |
| ENT symptoms | |||
| Nasal Congestion | 0.997 | 0.145 to 1.139 | 0.967 |
| Rhinorrhoea | 0.816 | 0.376 to -1.031 | 0.531 |
| Postnasal drip | 1.019 | 0.425 to 1.163 | 0.799 |
| MF | 1.007 | 0.546 to 0.160 | 0.931 |
| CF pain | 1.240 | 0.376 to 1.354 | 0.102 |
| Earache | 0.909 | 0.681 to 0.990 | 0.311 |
| Dysphagia | 0.972 | 0.431 to 1.174 | 0.781 |
| Dyspnoea | 0.951 | 0.605 to 1.104 | 0.521 |
RA: rheumatoid arthritis; WP : with polyps; COPD : chronic obstructive pulmonary disease; SLE : lupus erythematosus; OR : odds ratio; NP : without polyps.
After the expansion of SARS-CoV-2 in Europe, multiple authors have described the high incidence of SSD and STD in patients with COVID-19, even as the only clinical manifestation.7
Several studies have observed a high rate of recovery of smell within 1–2 weeks after the onset of anosmia or hyposmia, and a recovery of taste between the second and third week after the onset of ageusia or hypogeusia.6 As well as a higher prevalence of SSD and STD in women, young and with mild or asymptomatic symptoms.3
Identification and isolation of patients with SARS-CoV-2 is the most important strategy to slow the spread of the disease. Given the scarcity of diagnostic tests, it is important to determine which are the most common initial symptoms for early isolation. Within our population, we have especially investigated mild-moderate cases and we have confirmed the presence of anosmia or dysgeusia in a high percentage of patients.
We highlight as strengths of this study the size of the sample and the reproducibility of the questionnaire. Despite being a study with a reduced follow-up time (maximum one month), we consider that the findings are valuable insofar as they can define early prevention attitudes while helping to define lines of work for future studies. While the main limitation of this study corresponds to the use of a questionnaire by telematic means, which we can tend to underestimate the olfactory threshold.
ConclusionAt present, multiple publications have found a relationship between SARS-CoV-2 infection (COVID-19) and smell and/or taste dysfunction. These data suggest that there is a significant association between viral infection and olfactory or gustatory dysfunction, and that this information could help in the early diagnosis of SARS-CoV-2 disease.
Conflict of interestsThe authors declare no conflict of interest.
Please cite this article as: Ninchritz-Becerra E, Soriano-Reixach MM, Mayo-Yánez M, Calvo-Henríquez C, Martínez-Ruiz de Apodaca P, Saga-Gutiérrez C, et al. Evaluación subjetiva de las alteraciones del olfato y del gusto en pacientes con afectación leve por COVID-19 en España. Med Clin (Barc). 2021;156:61–64.