The aim of this study was to retrospectively evaluate the effect of cataract surgery on visual acuity (VA) and daily living activities in participants aged over 80 years.
MethodsFor eighty-three eyes from eighty three eligible patients aged 80 or above who had undergone cataract surgery between 2000 and 2005, preoperative and postoperative best-corrected visual acuity (BCVA), satisfaction score for daily living activities, surgical complications, and retinal pathologies affecting vision were recorded from the patient's file.
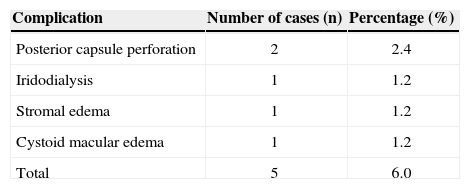
ResultsThe mean age of the patients was 86.80±5.24 years (range, 80-98). VA improved in the operated eye for patients aged 80 to 89 and for those over 90 years. Postoperative VA of 0.5 or better was more frequently observed in those aged 80 to 89 than in those aged over 90 years (90.6% and 73.4%, respectively). Mean postoperative scores for the daily living activities scale were significantly better in both groups as compared to preoperative levels, and were better in the 80 to 89-year age group than for those older than 90. Intraoperative posterior capsule perforation occurred in two participants, cystoid macular edema in one, iridodialysis in one and postoperative refractory stromal edema occurred in one case.
ConclusionsOur results showed that better VA levels for daily living activities can be obtained after cataract surgery in elderly patients aged over 80 years, thereby suggesting that cataract removal is effective removal in this population.
El objetivo de este estudio es evaluar de manera retrospectiva los efectos de la cirugía de cataratas sobre la agudeza visual (AV) y sobre las actividades de la vida diaria en pacientes mayores de 80 años.
MétodosSe incluyeron en el estudio 83 ojos de 83 pacientes mayores de 80 años que cumplían todos los criterios de inclusión y que se habían sometido a una intervención quirúrgica de cataratas entre los años 2000 y 2005. Para cada paciente, se tomó de su historia clínica la agudeza visual con la mejor corrección (o sus siglas en inglés, BCVA) tanto pre- como posquirúrgica, el índice de satisfacción relativo a las actividades de la vida diaria, las complicaciones derivadas de la intervención, y las patologías de la retina que padecía dicho paciente y que afectaban a su capacidad visual.
ResultadosLa edad media de los paciente fue de 86 años (rango: entre 80 y 98). La AV en el ojo operado mejoró, tanto para los pacientes con edades comprendidas entre los 80 y los 89 años como para los mayores de 90 años. Se obtuvieron más casos de AV posquirúrgica igual o mejor que 0.5 en el grupo de pacientes de entre 80 y 89 años que en el grupo de mayores de 90 años (90,6% de los casos frente a un 73,4%). El lo que respecta a la escala de actividades de la vida diaria, las puntuaciones promedio obtenidas tras la intervención fueron, para ambos grupos, significativamente mejores que los valores prequirúrgicos. Esta mejora observada tras la intervención fue más acusada en el grupo de pacientes de entre 80 y 89 años que en el grupo de mayores de 90. Hubo dos casos de perforación de la cápsula posterior ocurrida durante la operación, un caso de edema macular quístico, un caso de iridodiálisis, así como un caso de edema estromal posquirúrgico.
ConclusionesNuestros resultados muestran que se logra una mejor AV relacionada con las actividades de la vida diaria tras la cirugía de cataratas en personas ancianas de más de 80 años. Así pues, este resultado sugiere que la extracción de la catarata en esta población puede ser beneficioso.
Cataract is one of the most frequently occuring visual impairments among the ocular disease in the world. Cataract in very elderly patients can cause progressive painless vision loss.1 Because of the demographic shift in developed countries toward older age, the prevalence over the whole population has increased. The major indication for cataract surgery is to improve as many aspects of the visual function as possible, such as contrast sensitivity, disability glare and even visual fields. The goal is not only to improve functional vision, but also to improve performance in daily living activities. Despite this, controversy remains regarding the effectiveness of surgery in improving visual acuity (VA) in the elderly.2,3 In cataract patients over 80 years old, there is a relationship between postoperative VA and the ability to enjoy activities of daily life.4-6
In this study, we aim to evaluate the outcomes of cataract surgery in very elderly subjects. Accordingly, we analyzed retrospectively the postoperative VA, the effect of VA on the patient's ability to participate in their daily living activities, and the frequency of surgical complications.
MethodsA consecutive case series of residents of the city of Malatya, Turkey, who had undergone cataract surgery between 2000 and 2005, were recruited. Data were collected from medical record charts. This study followed the tenets of the Declaration of Helsinki with informed consents being signed by all subjects. The records from cataract patients were retrospectively evaluated and data from 83 eyes of 83 eligible patients who had had no previous ocular surgery and who had been followed-up for at least 1 month postoperatively were included.
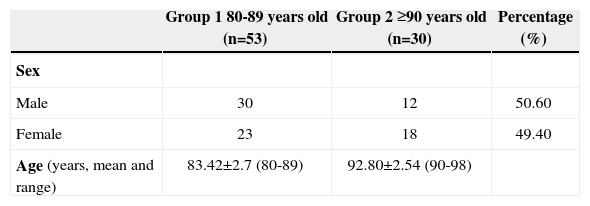
Patients were divided into two age groups: 80 to 89 years old (group 1) and older than 90 years old (group 2) (see Table 1). The primary outcome measure was VA levels for the performance of daily living activities. Patients were asked by phone to evaluate and rate the level of daily living activities after surgery (0=absent, 1=poor, 2=moderate, 3=good). A satisfaction score for daily living activities was obtained from the patients. A Snellen chart was used to evaluate preoperative and postoperative VA in all patients. Additionally, detailed data, including best-corrected VA (BCVA), intraocular pressure changes, anterior and posterior segment findings, type of cataract, surgical technique used, and any complications that may have occurred, were recorded from the patient files.
Statistical analyses were performed using SPSS software (Statistical Package for the Social Sciences, version 9.0, SPSS Inc, Chicago, IL, USA). Group comparisons of the preoperative and postoperative BCVA and daily living activities score were performed using Mann-Whitney U test. Within-group comparisons of the BCVA and daily living activities score were done with the paired-t test. The correlation between BCVA values and daily living activities scores was performed using Pearson correlation analysis test, where a P value lower than 0.05 was considered to be statistically significant.
ResultsDemographic data of the groups are shown in table 1. The overall study population consisted of 83 eyes from 83 eligible cataract-surgery patients. Group 1 included 53 patients (23 female, 30 male; mean age, 83.42±2.7 years; range, 80-89 years), and group 2 included 30 patients (18 female, 12 male; mean age of 92.80±2.54; range, 90-98). No significant difference in the distribution of male versus female was found (P>0.05).
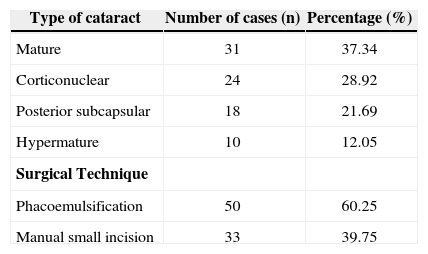
The cataracts were classified as either corticonuclear, posterior subcapsular, mature, or hypermature cataract. The surgical technique performed was either phacoemulsification (n=50 eyes) or manual-small-incision cataract surgery (n=33 eyes) (see Table 2), both with peribulbar anesthesia. Intraocular lens implantation was carried out in all eyes included in this study. The mean follow-up was 6.01±2.56 months (range, 1-12 months) after the cataract surgery.
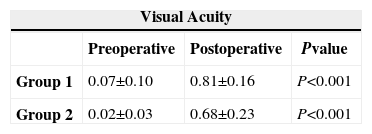
Best-corrected visual acuity improved significantly after surgery in both group 1 (0.07±0.10 vs. 0.81±0.16; P<0.001) and group 2 (0.02±0.03 vs. 0.68±0.23; P<0.001) (see Table 3). Visual acuity was much better in the operated eyes in both groups of patients (P<0.001). Overall, a BCVA ≥0.5 was obtained in 84.4% of the operated eyes. Postoperative BCVA of 0.5 or above was more common among group-1 patients than among group-2 patients (90.6% vs. 73.4%, respectively). Postoperative VA levels were better in patients that had shown good preoperative visual acuity.
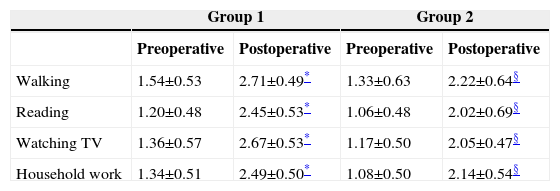
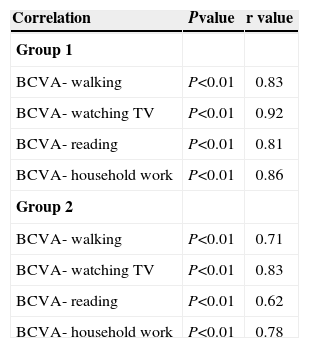
Patient satisfaction scores regarding the ability to perform daily living activities (i.e., walking, reading, watching TV, and household work) after surgery were significantly better in both groups, compared with their pre-surgery scores (P<0.001) (see Table 4). Daily living activities scores were higher among group 1 than in group 2. There was a significant correlation between postoperative BCVA and the corresponding daily living activities scores in both groups of patients (P<0.01 for both groups) (see Table 5).
Satisfaction levels as regards daily living activities for the subjects under study (Mean ± SD)
Correlation analysis between postoperative BCVA and the various scores obtained for the daily living activities scale, summarized for each patient group
| Correlation | Pvalue | r value |
| Group 1 | ||
| BCVA- walking | P<0.01 | 0.83 |
| BCVA- watching TV | P<0.01 | 0.92 |
| BCVA- reading | P<0.01 | 0.81 |
| BCVA- household work | P<0.01 | 0.86 |
| Group 2 | ||
| BCVA- walking | P<0.01 | 0.71 |
| BCVA- watching TV | P<0.01 | 0.83 |
| BCVA- reading | P<0.01 | 0.62 |
| BCVA- household work | P<0.01 | 0.78 |
Pearson correlation analysis; BCVA: best-corrected visual acuity.
Of the 83 eyes, 5 of them (representing 6.0%) had surgical complications. During surgery, iridodialysis occurred in 1 eye and posterior capsule perforation in 2 eyes, one of which had an anterior vitrectomy and cystoid macular edema was detected postoperatively. In another patient, treatment-resistant corneal stromal edema was observed (see Table 6).
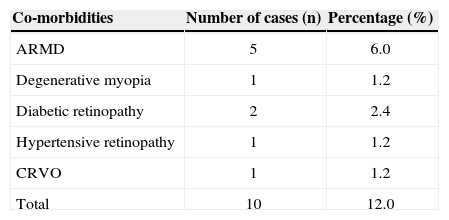
Retinal co-morbidities that decreased the level of postoperative visual acuity were age-related macular degeneration (ARMD) (5 patients), degenerative myopia (1 patient), diabetic retinopathy (2 patients), hypertensive retinopathy (1 patient), and central retinal vein occlusion (1 patient) (see Table 7). BCVA were <0.5 in these patients.
Retinal co-morbidities that decreased postoperative visual acuity
| Co-morbidities | Number of cases (n) | Percentage (%) |
| ARMD | 5 | 6.0 |
| Degenerative myopia | 1 | 1.2 |
| Diabetic retinopathy | 2 | 2.4 |
| Hypertensive retinopathy | 1 | 1.2 |
| CRVO | 1 | 1.2 |
| Total | 10 | 12.0 |
ARMD: age-related macular degeneration; CRVO: central retinal vein occlusion.
Cataract is the most frequent disease causing visual loss in elderly people worldwide.7 Age is the most important risk factor for developing a cataract,7,8 but increasing age is also known to influence the visual acuity achieved after cataract surgery.9 Natural aging and delayed surgery negatively impact postoperative visual acuity as well as surgical outcomes in elderly patients.10,11
It is difficult to recommend cataract surgery to an elderly patient, owing to additional difficulties like a higher incidence of hard nucleus, smaller pupil sizes, high rates of exfoliation syndrome, and difficult patient cooperation during surgery.5 The surgeon's experience is another factor that influences surgical outcomes. Disagreement remains as to what the benefits of surgery in elderly patients and further investigations are needed to determine the effectiveness of the surgery.
The lower percentage of postoperative BCVA ≥0.5 in group 2 compared with group 1 probably reflects the higher frequency of ocular comorbidity associated with advanced age in patients in the group 2. If visual outcome is evaluated in patients without considering ocular comorbidity, group 2 still has significantly worse outcomes. Thus, aging might have a negative influence on visual outcome.
In most patients, improvement of VA was attained following cataract surgery. The results were consistent with previous studies.5,6 We obtained better postoperative visual acuity levels in patients with higher preoperative visual acuities.
Lundstrom and colleagues5 suggest that the outcome of cataract surgery in the very elderly should be considered to be very good. Their findings indicate that visual outcomes after cataract surgery are worse in older patients compared with that achieved by younger ones, but that certain subgroups of elderly patients may attain an excellent outcome. Some studies reported that poor VA levels were obtained in elderly patients because postoperative complications are more common among this population segment.4,12 In the present study, only a few patients (6%) did not have expected VA levels because of posterior capsule perforation, postoperative cystoid macular edema and corneal stromal edema. Syam and colleagues13 reported that surgeons should not be deterred from offering cataract surgery to the very elderly, as successful visual rehabilitation is the norm. Nonetheless, they suggest that a further prospective multicentre study is required to confirm the benefits and to assess the risks of cataract surgery in this age group.
Coexisting ocular diseases, such as retinal pathologies, as well as aging can limit the effectiveness of cataract surgery and its visual outcome. We have also found ocular comorbidity in patients without satisfactory postoperative visual improvement. Given the increasing prevalence of ocular comorbidities with advancing age, it is not surprising that VA is worse for group 2 than for group 1 patients.
In the literature, ARMD is the most common comorbidity that decreases visual outcome after cataract surgery.3,12,14 Wong3 reported that a higher prevalence of pre-existing ocular diseases—for example, age-related maculopathy—may affect cataract surgery outcomes in very elderly patients. Progression of ARMD after cataract surgery has been suggested.14 Coexisting ocular abnormalities have been shown to have a negative effect on postoperative visual results.5 The increased risk of progression of diabetic retinopathy and development of macular oedema after cataract surgery in high risk patients is well known15. In our study, the ocular comorbidities that resulted in decreased VA were ARMD, degenerative myopia, diabetic retinopathy, hypertensive retinopathy, and central retinal vein occlusion.
One of the major public concerns regarding cataract surgery has been that prolonged waiting times may not only result in patients becoming increasingly symptomatic but also that worsening VA may cause functional impairment.16 Also, it may increase patient concerns.17 In the elderly, daily living activities are restricted by the effect of age. Despite this, more than 70% of elderly patients experienced improvement in their ability to cope with daily living activities.6 A reduction in VA increases this problem and reduces life expectancy.18,19 As we know, life expectancy is an important factor when judging whether or how to perform surgery. Cataract surgery has been shown to improve daily living activities in elderly patients as a result of the improvements attained in terms of VA.5,6,9 Similarly, in the present study, daily living activities scores improved for almost all patients after surgery. Thus, a patient may have a good probability of living long enough to enjoy the benefits of improved VA, without suffering from depression. In this context, Elam and colleagues20 suggested that changes in the level of function one year after cataract surgery were not explained solely by the changes in vision, but were also conditional on baseline function and baseline mental status and mediated in part by changes in mental status.
Our study must be viewed in light of some limitations. First, a Snellen chart was used to assess preoperative and postoperative VA in all patients. However, Snellen visual acuity is a poor way of measuring visual acuity in clinical research, a fact that might have affected the measured outcomes. Second, we have not used a validated questionnaires such as the ADVS or VF-14 to assess functional vision. This might have been a source of bias.
In conclusion, we found that functional outcomes of cataract surgery in very elderly patients are beneficial. Based on these findings, we believe that restoring vision with cataract surgery is helpful even in patients with advanced age, as it maintains their ability to deal with daily living activities, which may improve social ability and extend life expectancy.
Financial disclosure: We have no personal or financial relationships that could have any potential to inappropriately influence (bias) our actions or the manuscript. Moreover, no financial or other potential conflicts of interest exist regarding the manuscript, including involvement with any organization with a direct financial, intellectual, or other interest in the subject of the manuscript. There are no grants and sources of financial support related to the topic or topics of the manuscript.