A 41-year-old patient with visual disturbances after an ocular trauma in right eye three years before was carefully analyzed and discussed. No corneal or intraocular sequelae were present. Only a significant anisocoria could be observed. Right eye (RE) achieved a best spectacle-corrected visual acuity (BSCVA) of 0.05 LogMAR with a refraction of +0.50 sphere and −1.25 cylinder. Left eye (LE) achieved a BSCVA of 0.0 LogMAR with a refraction of +0.75 sphere and −1.00 cylinder. In photopic conditions pupil diameter was 4.96mm for RE and 3.02mm for LE whereas in scotopic conditions, these values were 7.45mm and 6.71mm, respectively. More significant levels of higher-order corneal and ocular aberrations were found in RE for the same pupil size. In addition, the scattering index (OSI) was 3.8 in RE and 1.0 in LE (4-mm pupil). In conclusion, anisocoria can lead to relevant visual disturbances if significant interocular differences in ocular aberrations and scattering are present.
Se analizó y discutió meticulosamente el caso de un paciente de 41 años que presentaba alteraciones visuales después de un traumatismo ocular en el ojo derecho ocurrido tres años atrás. No presentaba secuelas corneales ni intraoculares. Solamente se observó una anisocoria significativa. El ojo derecho (OD) obtuvo una agudeza visual mejor corregida con gafas (AVMCG [BSCVA en inglés]) de 0,05 LogMAR, con una refracción de +0,50 de esfera y −1,25 de cilindro. El ojo izquierdo (OI) obtuvo una AVMCG de 0,0 LogMAR, con una refracción de +0,75 de esfera y −1,00 de cilindro. En condiciones fotópicas, el diámetro de la pupila fue de 4,96mm para el OD y de 3,02mm para el OI, mientras que en condiciones escotópicas estos valores fueron de 7,45mm y 6,71mm respectivamente. En el OD se hallaron niveles más significativos de aberraciones corneales y oculares de orden superior para el mismo tamaño de pupila. Además, el índice de dispersión (OSI) fue de 3,8 en el OD y de 1,0 en el OI (pupila de 4mm). En conclusión, la anisocoria puede dar lugar a alteraciones visuales relevantes si hay diferencias interoculares significativas en dispersión y aberraciones oculares.
Visual quality degradation due to ocular aberrations is in relation with pupil diameter; ocular optical quality is pupil-dependent.1 Rays entering the eye close to the pupil centre are less affected by optical aberrations than those passing through peripheral areas where irregularity and significant power changes are present. Symmetric aberrometric patterns between eyes are normally found in the general population assuming a similar pupillary size for both eyes.2 However, anisocoria, which is the presence of unequal pupillary size in both eyes due to different causes such as ocular trauma,3 may avoid this aberrometric symmetry. To date, interocular differences in visual quality as a consequence of the presence of anisocoria have not been still reported. To the best of our knowledge, this is the first report of a case of noticeable disturbing visual quality difference between eyes in a patient with anisocoria. The clinical implications of this phenomenon are discussed.
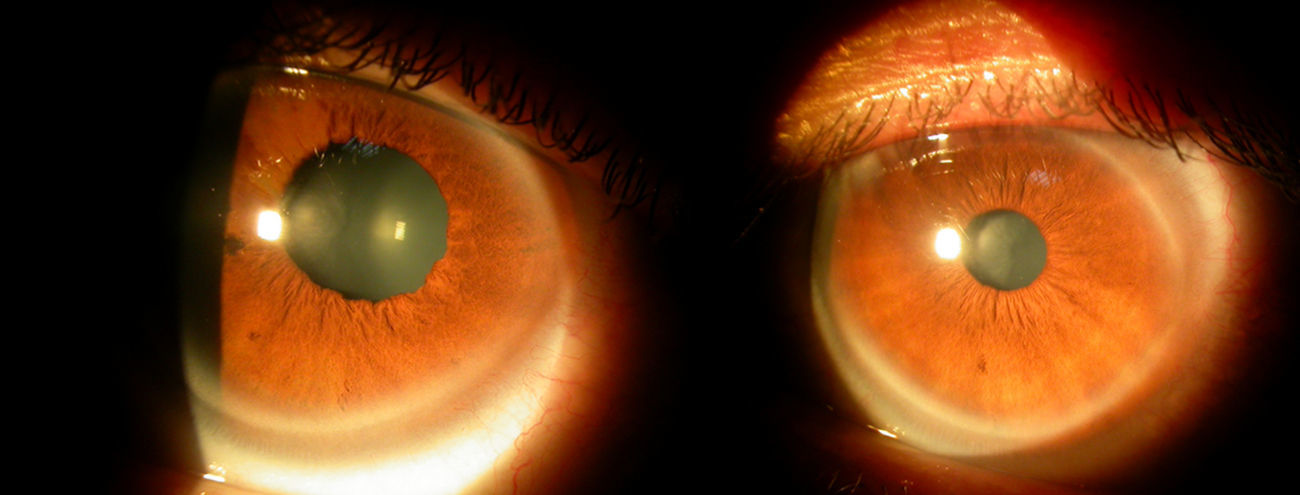
MethodsA white male of 41-year-old with post-traumatic anisocoria and significant visual disturbances was comprehensively examined in order to find a reason for his visual complaints. The patient had suffered an ocular trauma by a squash ball during a match in his right eye 3 years ago. Since then, the patient perceived significant visual quality deterioration in that eye. According to the medical reports provided by the patient, 2 days after the trauma he presented in his right eye a macular edema leading to a temporary visual acuity reduction, an associated coroidal hemorrhage, iris dislocation (nasally) producing an irregular pupil contour, iris root hemorrhage, and a traumatic uveitis. After adequate medical treatment (2 months after trauma), no corneal or intraocular sequelae were present. Only a residual anisocoria remained. However, after complete recovery of ocular trauma the patient was able to perceive a significant visual quality difference between eyes. He referred to see blurry with light distortion as well as transient “blindness” when changing from a luminous to a dark environment. In addition, he also referred significant night vision disturbances with right eye as halos and glare (VF-14 questionnaire) and the presence of a veil distorting small letters significantly when reading. This distortion disappeared when the patient turned his eye laterally to read.
A complete ocular examination was performed in order to find the possible origin of all his disturbances including: uncorrected visual acuity (UCVA), best-spectacle corrected visual acuity (BSCVA), subjective refraction, anterior (slit lamp) and posterior (indirect ophthalmoscopy) segment evaluation, dynamic pupillography (CA-100 FLUO, Topcon Corporation, Tokyo, Japan), contrast sensitivity (SWCT, Stereo Optical Co, Chicago, USA), corneal topography and aberrometry (CA-100 FLUO, Topcon Corporation, Tokyo, Japan), ocular or global aberrometry (COAS, AMO Wavefront Sciences LLC, Albuquerque, USA), and ocular optical performance characterization (point spread function PSF, modulation transfer function MTF, ocular scattering index (OSI) with a double-pass OQAS system, Visiometrics SL, Terrassa, Spain). In addition, macular morphology was also analyzed by means of optical coherence tomography (Fourier-domain OCT 3D-1000 system, Topcon, Tokyo, Japan) in order to rule out macular pathology persistence. All measurements were performed by the same experienced examiner.
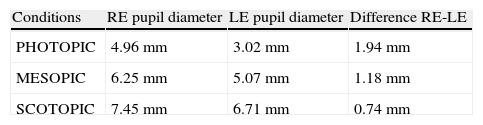
ResultsRight eye (RE) achieved the best spectacle-corrected visual acuity (BSCVA) of 0.05 LogMAR (0.9 decimal) with a refraction of +0.50 sphere and −1.25 cylinder, and left eye (LE) achieved an BSCVA of 0.0 LogMAR (1.0 decimal) with a refraction of +0.75 sphere and −1.00 cylinder. Binocular BSCVA was 0.0 LogMAR (1.0 decimal). We had no data about the refractive status prior to the ocular trauma but the patient assured that he did not need glasses. During biomicroscopic examination, a transparent cornea and a clear crystalline lens were observed. No signs of corneal scar or incipient cataract could be detected. Right pupil was slightly irregular and its response to light was sluggish when compared to left pupil. Dynamic pupillography revealed a variable anisocoria under different illumination conditions (Table 1). The highest difference in pupil diameter between eyes (1.94mm) was found in photopic conditions (Fig. 1). Pupil diameter in such conditions was 4.96mm for RE and 3.02mm for LE whereas in scotopic conditions these values were 7.45mm and 6.71mm (Table 1). Retinal exploration did not show relevant signs of pathology or former sequelae. Macular morphology was normal with a mean central thickness of 206μm for RE and 201μm for LE.
Dynamic pupillography outcomes obtained with the Topcon CA-100 FLUO system. Pupil diameter differences were evaluated for three different illumination conditions: photopic, mesopic and scotopic. As can be seen in the table, the highest difference in pupil diameter between eyes (1.94mm) was found in photopic conditions.
| Conditions | RE pupil diameter | LE pupil diameter | Difference RE-LE |
| PHOTOPIC | 4.96mm | 3.02mm | 1.94mm |
| MESOPIC | 6.25mm | 5.07mm | 1.18mm |
| SCOTOPIC | 7.45mm | 6.71mm | 0.74mm |
RE: right eye; LE: left eye.
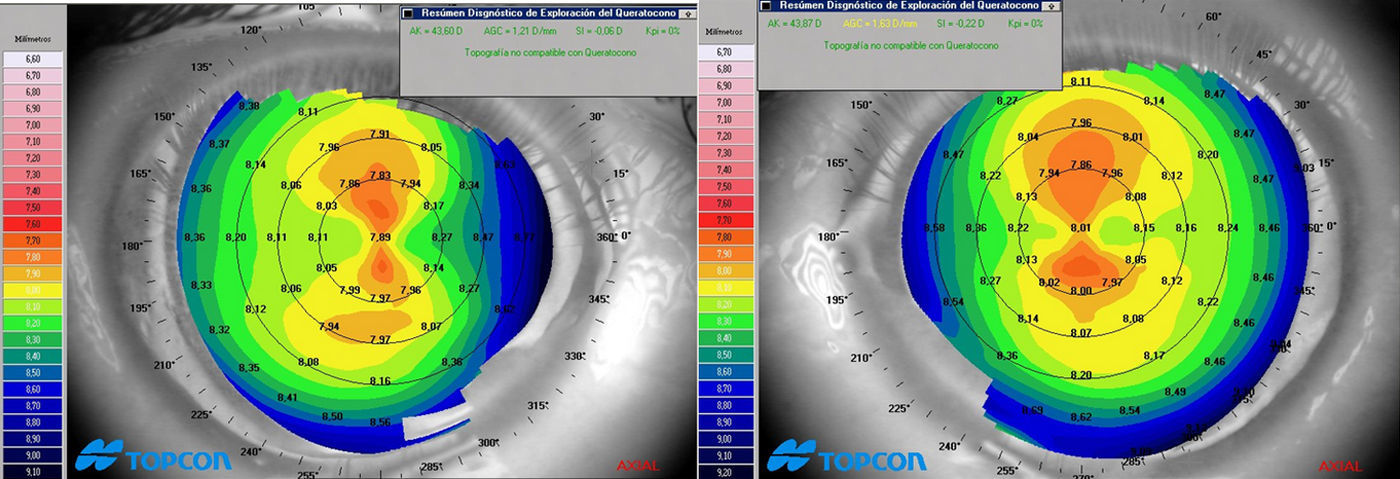
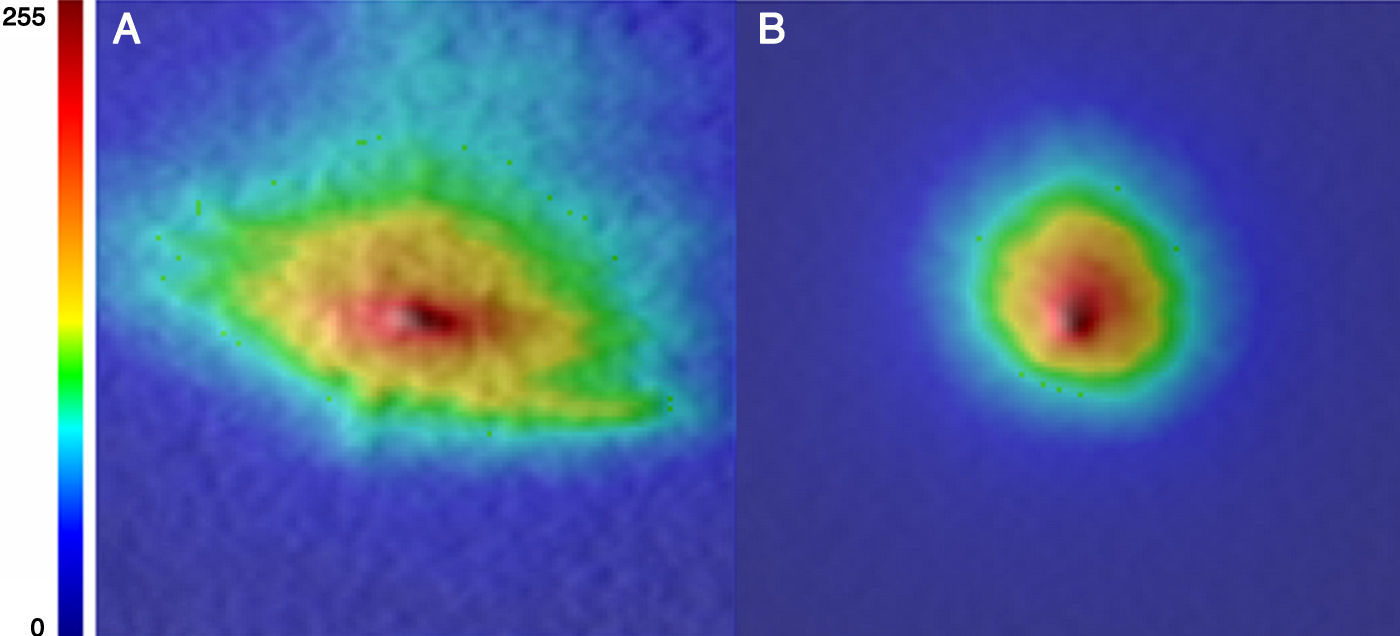
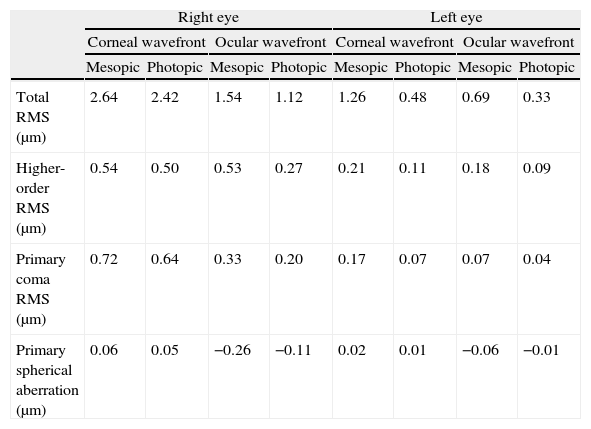
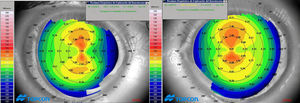
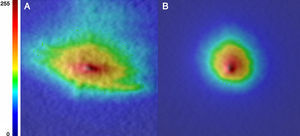
Corneal topography revealed a similar corneal bow-tie configuration in both eyes (Fig. 2). Similar mean corneal power in the 3-mm central area was found in both eyes (RE 42.23 D vs LE 42.16 D). A more significant prolate configuration was found for the left cornea (asphericity in a 4.5-mm area, RE −0.08 vs LE −0.51; asphericity in a 8.0-mm area, RE −0.39 vs LE −0.69). The pupil-vertex offset was found to be similar in both eyes: RE 0.51mm at 117° (pupil size: 5.38mm) vs. LE 0.60mm at 90° (pupil size: 2.78mm). Regarding aberrometric outcomes, Table 2 shows a comparative analysis of root mean square (RMS) values for both eyes in mesopic conditions. As can be seen in the table, all ocular RMS values were approximately doubled for the right eye when compared to left eye in mesopic conditions. Similar tendency was observed for corneal aberrometry, except for primary spherical aberrations (similar values both eyes). Finally, point spread function (PSF) analysis of both eyes showed a poorer retinal image quality for right eye (Fig. 3). Strehl ratio was 0.05 for RE and 0.13 for LE, calculated both values for a same pupil diameter of 6.0mm. Modulation transfer function (MTF) cut-off point was higher for LE, 4.651 c/° RE vs 18.606 c/° LE. In addition, the ocular scattering index (OSI) was four times higher in RE when compared to LE (3.8 RE vs 1.0 LE) (measured for the same papillary diameter, 4.0mm).
Comparative analysis of corneal aberrometry and ocular aberrometry results for both eyes in photopic (RE pupil 5.0mm; LE pupil 3.0mm) and mesopic conditions (RE pupil 6.0mm; LE pupil 5.0mm).
| Right eye | Left eye | |||||||
| Corneal wavefront | Ocular wavefront | Corneal wavefront | Ocular wavefront | |||||
| Mesopic | Photopic | Mesopic | Photopic | Mesopic | Photopic | Mesopic | Photopic | |
| Total RMS (μm) | 2.64 | 2.42 | 1.54 | 1.12 | 1.26 | 0.48 | 0.69 | 0.33 |
| Higher-order RMS (μm) | 0.54 | 0.50 | 0.53 | 0.27 | 0.21 | 0.11 | 0.18 | 0.09 |
| Primary coma RMS (μm) | 0.72 | 0.64 | 0.33 | 0.20 | 0.17 | 0.07 | 0.07 | 0.04 |
| Primary spherical aberration (μm) | 0.06 | 0.05 | −0.26 | −0.11 | 0.02 | 0.01 | −0.06 | −0.01 |
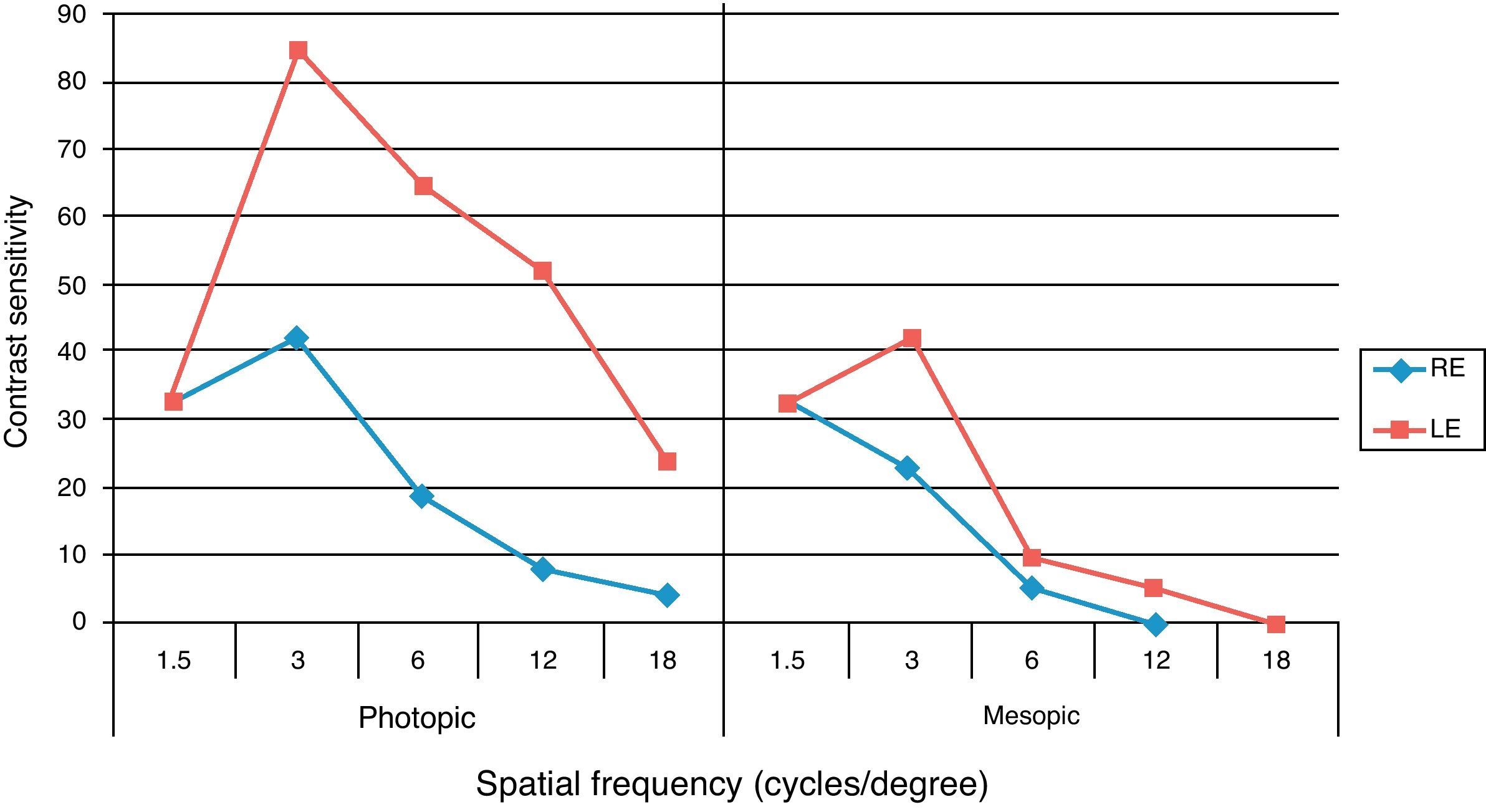
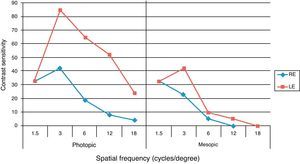
Finally, a clear and significant difference in contrast sensitivity was found between eyes in mesopic and photopic conditions, with the worst outcomes for the RE, as shown in Fig. 4.
DiscussionThe level of optical aberrations present in the eye is pupil-dependent. All type of aberrations are magnified with increasing pupil size,4,5 as it happens in scotopic conditions or under cycloplegia.6 This aberrometric magnification due to changes in pupil size induces a quantifiable decrease in visual performance.7 However, it has not been still reported the visual consequences of anisocoria where the unequal pupil size of both eyes will induce a significant difference in the level of aberrations of each eye. In the case described in this report we have observed a marked difference in the level of corneal and ocular aberrations between eyes due a post-traumatic anisocoria. This fact was in concordance with the marked difference in PSF and MTF observed between eyes. The eye that suffered the trauma (right eye) showed a worse optical performance with higher amounts of low and higher order aberrations in photopic, mesopic and scotopic conditions. This higher level of optical aberrations in the right eye compared to the left was even observed when the aberrometric coefficients were calculated using the same pupil aperture. It should be mentioned that ocular and corneal aberrations were obtained centering on pupil. Translation of the pupil center with respect to the vertex8 and changes in the pupil center position associated to modification in its diameter9 can lead to some errors in the calculations of aberrations. However, the pupil-vertex offset was found to be similar in topographic measurements obtained in both eyes and unable to account for the clinically relevant aberrometric difference among eyes. Regarding pupil center changes with natural dilation, it has been shown that they used to be limited in eyes with normal pupil function.9 In our case, pupil changes were found to be minimal (1mm as much) in the eye with constant mydriasis, and therefore with slight variations of the pupil center position. Therefore, the aberrometric data reported here are representative of the optical quality associated to each eye of this patient. However, optical aberrations were not the only factor inducing a limited optical resolution of the right eye. In this case ocular scattering was also tested and we found a scattering level in right eye double than that found in the left eye (calculated for the same pupil size). Therefore, the diminished optical resolution of the right eye can be explained by larger levels of aberrations and scattering in this eye.
Regarding subjective symptoms, we have observed that in our case they were in relation with the different pupillary dynamic behaviour of each eye and then with the different aberrometric pattern that have an asymmetric effect on contrast sensitivity. The perception of different visual quality with each eye referred by the patient is explained perfectly by the different optical resolution of both eyes. In near vision, the perception of two images with a marked difference in quality could explain the disturbances referred by the patient: presence of a veil distorting letters. One explanation for the disappearance of such distortion when the patient turned his head laterally may be the centration of the left eye in the visual field (eye with the best visual performance) with this maneuvre, avoiding the distortion from the right eye. The disparity in optical quality between eyes observed in the case described here may also have a significant effect on binocular summation. It should be noted that an excellent binocular vision requires optimum brightness of retinal images and minimal difference between retinal images.10–14 Therefore, the veil distorting small letters significantly during reading referred by the patient may be also in relation with the potential effect on binocularity of the interocular difference in optical quality, avoiding a normal and functional binocular fusion. The presence of some degrees of diplopia can appear after ophthalmologic procedures inducing differences in retinal images.15 Finally, the higher amounts of aberrations and scattering in right eye justified the night vision disturbances perceived by the patient although anisocoria in scotopic conditions was not so significant. It should be considered that patients with large scotopic pupil sizes used to have an increased aberrometric profile leading to the potential of significant induction of night vision disturbances.16,17
In conclusion, anisocoria should be also considered as a limiting entity of visual performance because it induces significant differences in the aberrometric pattern between eyes. When severe anisocoria is combined with differences in the level of scattering among eyes, visual difficulties are very probable to be referred by the patient. If patients like this are screened for refractive surgery, customized ablation profiles may be recommendable in order to minimize at least the difference in aberrations between eyes. If a non-wavefront-guided ablation profile is programmed in cases like this, the symptomatology of this kind of patients can persist or even magnified. In addition, it should be considered that anisocoria might also influence the options for a future intraocular lens implantation or contact lens fitting for presbyopic correction, because some of the available options for this type of correction are pupillary-dependent. Specifically, refractive multifocal intraocular lenses and contact lenses are pupillary-dependent and therefore the visual quality provided by them may vary significantly with pupillary changes.18–21 Therefore, this type of IOLs and contact lenses should be avoided to be used as a correction option in anisocoric patients. Pupillary examination is an indispensable test before cataract and corneal refractive surgery not only for programming the surgical procedure but also for detecting cases of anisocoria requiring a different management. In addition, this test must be always performed to evaluate the suitability of multifocal contact lens fitting.