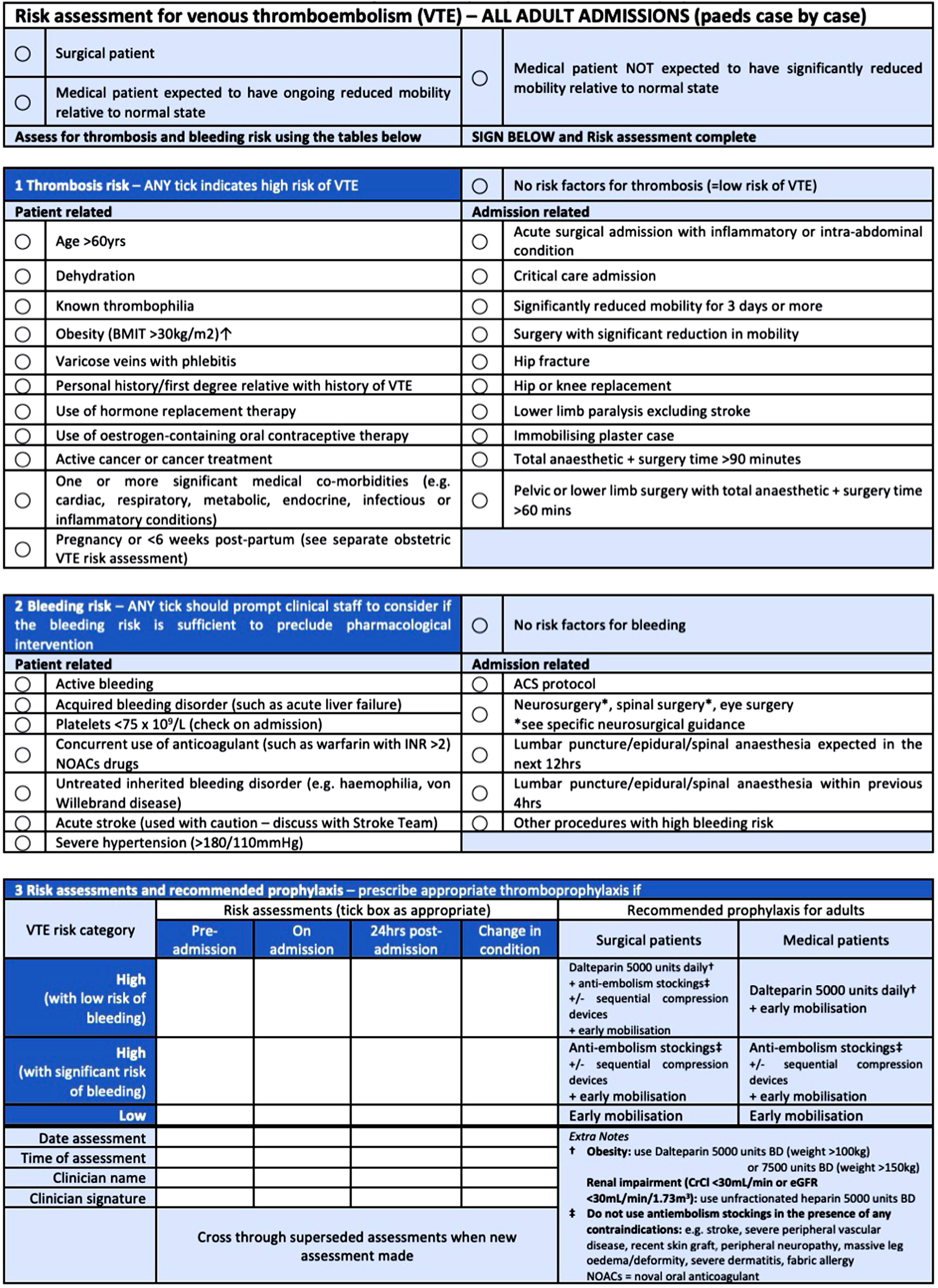
Surgical patients are at risk of hospital-acquired venous thromboembolisms (VTEs), and preventative measures such as thromboembolism deterrent stockings (TEDs) and low molecular weight heparin (LMWH) are proven to be beneficial. The National Quality Requirement in the NHS Standard Contract 2017/19 in England mandates that 95% of inpatients undergo VTE risk assessments. As hospitals transition to Electronic Patient Records (EPR), it is important to observe the impact on vital safety indicators such as VTE risk. The aim of this study is to observe the effect of implementing EPR in a tertiary centre on adherence to national guidelines, including VTE assessment rates and prophylaxis administration in surgical patients.
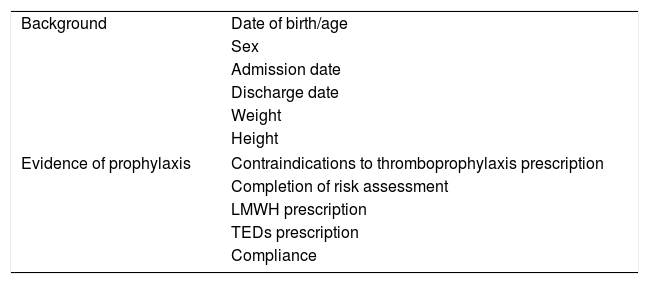
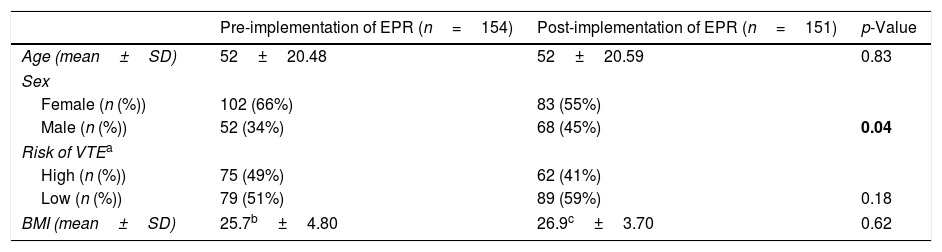
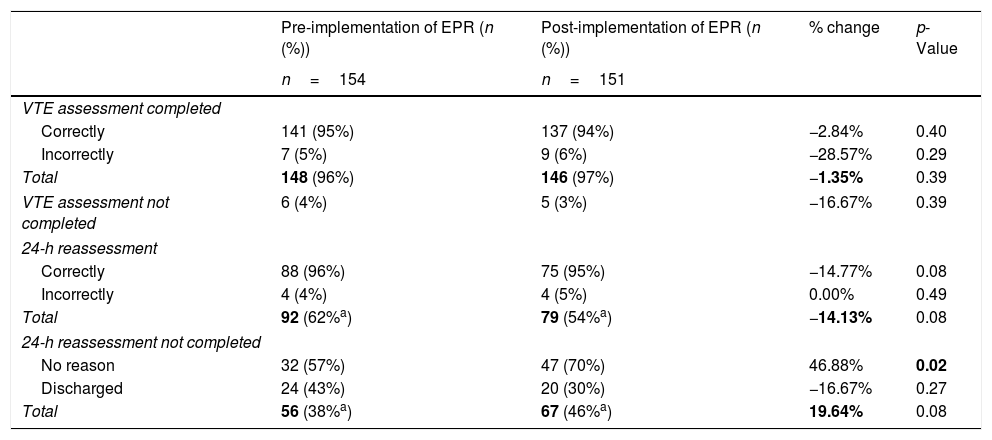
Materials and methodsUsing consecutive sampling, all acute surgical admissions at the hospital from 26/02/2018 to 18/03/2018 (n=154) pre-EPR and 31/10/2018 to 25/11/2018 (n=151) post-EPR were observed for VTE risk assessment, 24-h re-assessment, prophylaxis prescriptions, administration, and patient compliance. Data was compared using a two-tailed Z-test.
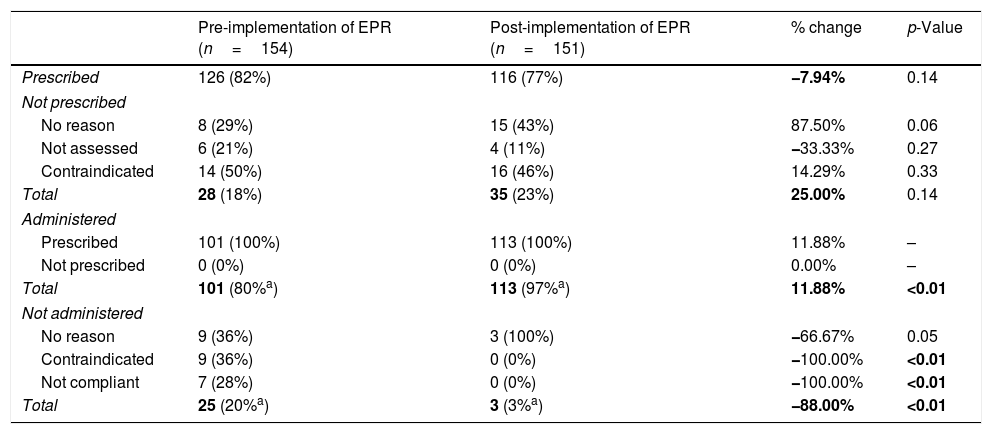
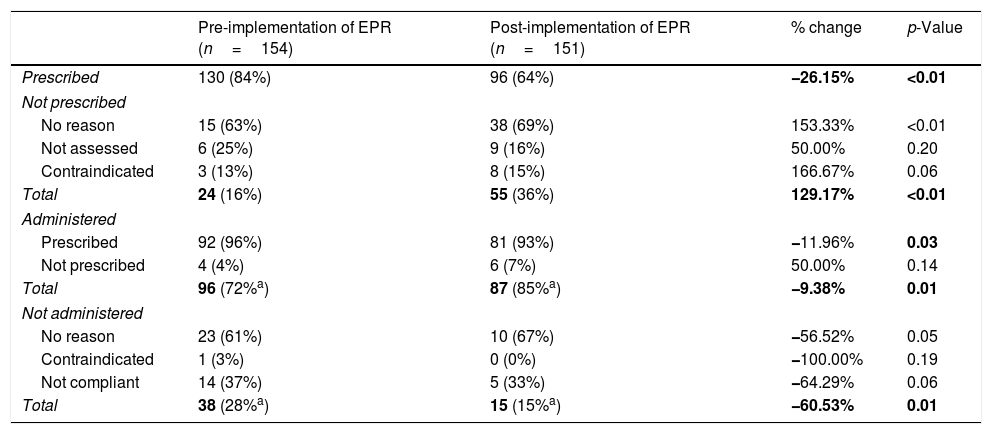
ResultsPre-EPR, 96% of patients had completed VTE assessments, which increased after EPR implementation to 97% (p=0.39). LWMH prescription rates decreased from 82% to 77% following EPR (p=0.14). Moreover, TED prescriptions decreased from 84% to 64% post-EPR (p<0.01). Administration rates of prophylaxis generally improved post-EPR. The 24-h re-assessment rate decreased from 62% to 54% of patients (p=0.08).
ConclusionThe study demonstrated that EPR is non-inferior to paper records. Transitioning to an EPR system did not interfere with the completion of VTE risk assessments, hence did not negatively impact the ability to achieve national targets.
Los pacientes quirúrgicos tienen un riesgo especial a padecer tromboembolismos venosos (TEV) y las medidas preventivas han demostrado ser beneficiosas. El Requisito Nacional en el Contrato del Servicio Nacional de Salud (NHS) 2017/19 asignó como mandato que el 95% de los pacientes tienen valoraciones de riesgo de TEV. Debido a la transición a los registros electrónicos de pacientes (EPR), es importante observar su impacto en estas evaluaciones. El objetivo de este estudio es observar el efecto de la implementación del EPR en un hospital terciario con respecto a las valoraciones de TEV y a la administración de profilaxis en pacientes quirúrgicos.
Materiales y métodosTodas las admisiones quirúrgicas agudas del hospital fueron observadas desde el 26 de febrero del 2018 al 18 de marzo del 2018 (n = 154) antes de la implementación del EPR y desde el 31 de octubre del 2018 al 25 de noviembre del 2018 (n = 151) después del EPR. El riesgo de TEV, la reevaluación de 24 horas, la prescripción de profilaxis, la administración y el cumplimiento de los pacientes fueron recolectados con el muestreo consecutivo. Comparamos estos datos con una prueba Z.
ResultadosAntes del EPR, el 96% de los pacientes tuvieron evaluaciones de TEV completas, esto aumentó después del EPR al 97% (p = 0,39). Las prescripciones de la heparina de bajo peso molecular (HBPM) disminuyeron del 82 al 77%, posterior al EPR (p = 0,14). Además, las prescripciones de calcetines de compresión de disuasión tromboembólica (TED) disminuyeron del 84 al 64% (p < 0,01) y las tasas de administración de profilaxis mejoraron. La reevaluación de 24 horas disminuyó del 62 al 54% (p = 0,08).
ConclusionesEste estudio mostró que el EPR no es inferior que los registros de papel. La transición a este no interfirió con las evaluaciones y se siguieron cumpliendo los requisitos nacionales.