The first wave of the SARS-CoV-2 pandemic exerted enormous stress on the healthcare system. Community of Madrid hospitals responded by restructuring and scaling their capacity to adapt to the high demand for care.
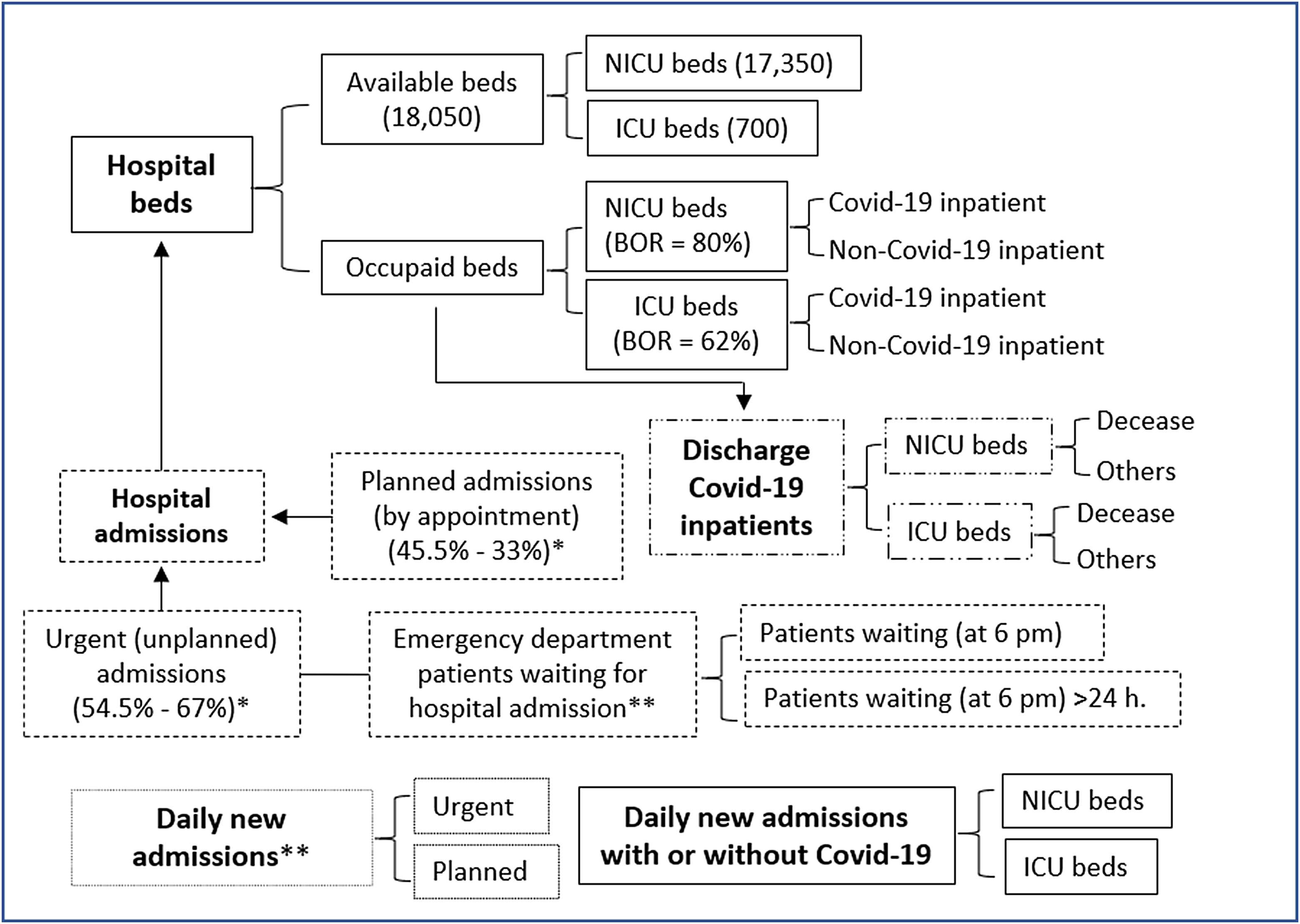
MethodsThis was a retrospective observational study conducted between 18 March and 21 June 2020 with data from public and private hospitals in CoM, Spain. Absolute and relative frequencies were calculated for inpatients with and without COVID-19, available and occupied beds in intensive care unit (ICU) and non-ICU wards, daily new admissions (NA), individuals awaiting hospitalisation in the emergency department (ED), and discharges.
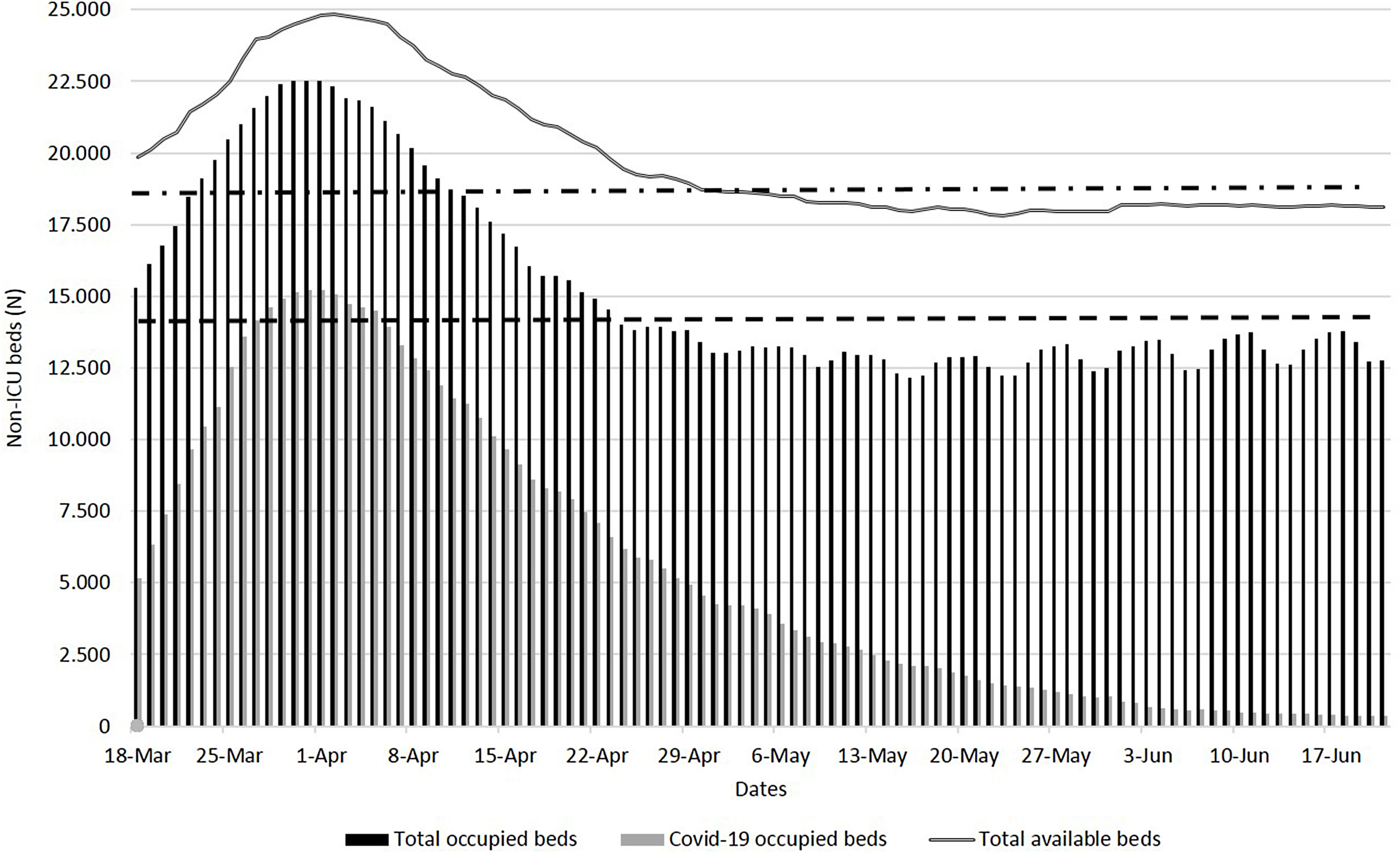
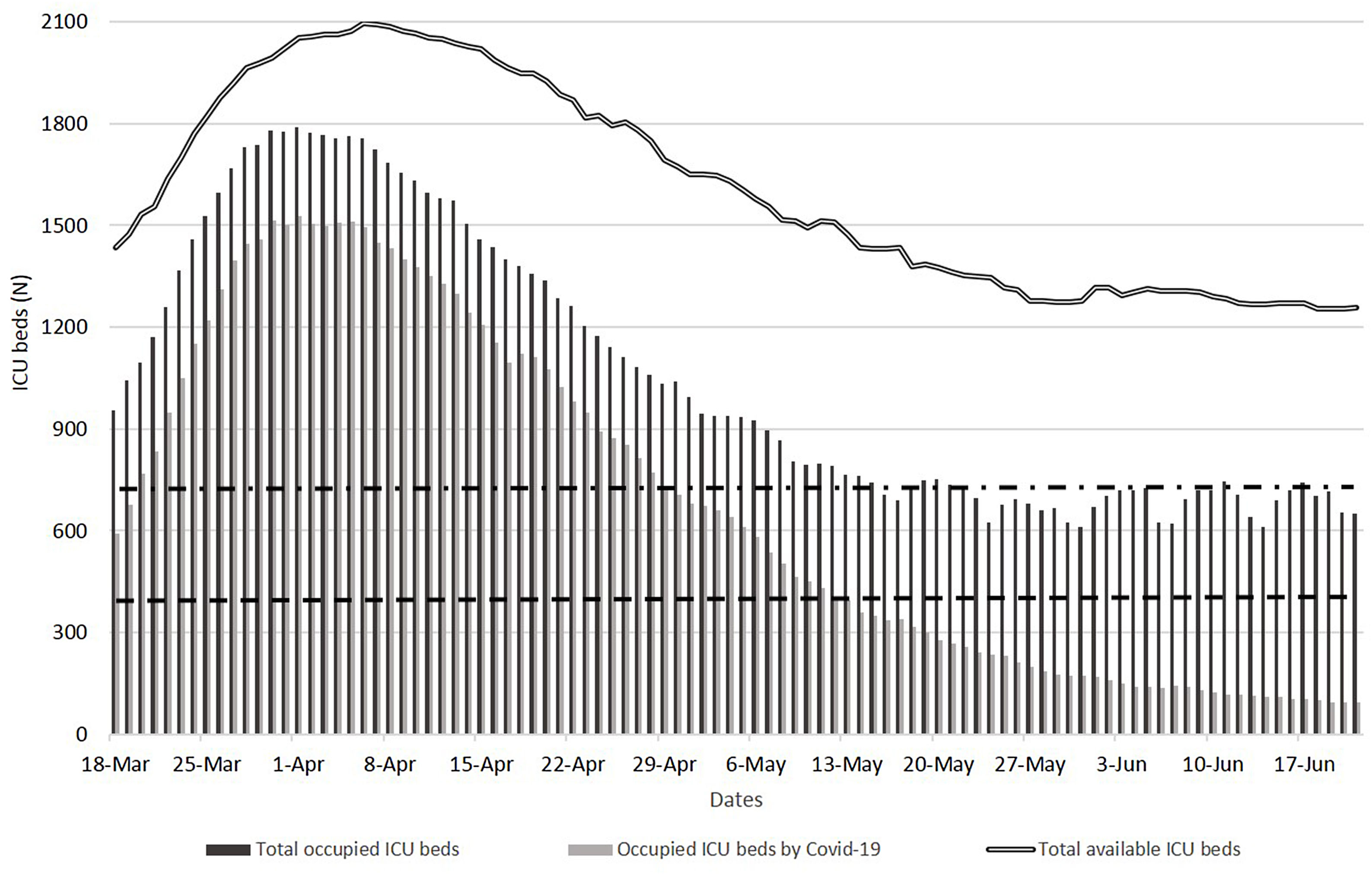
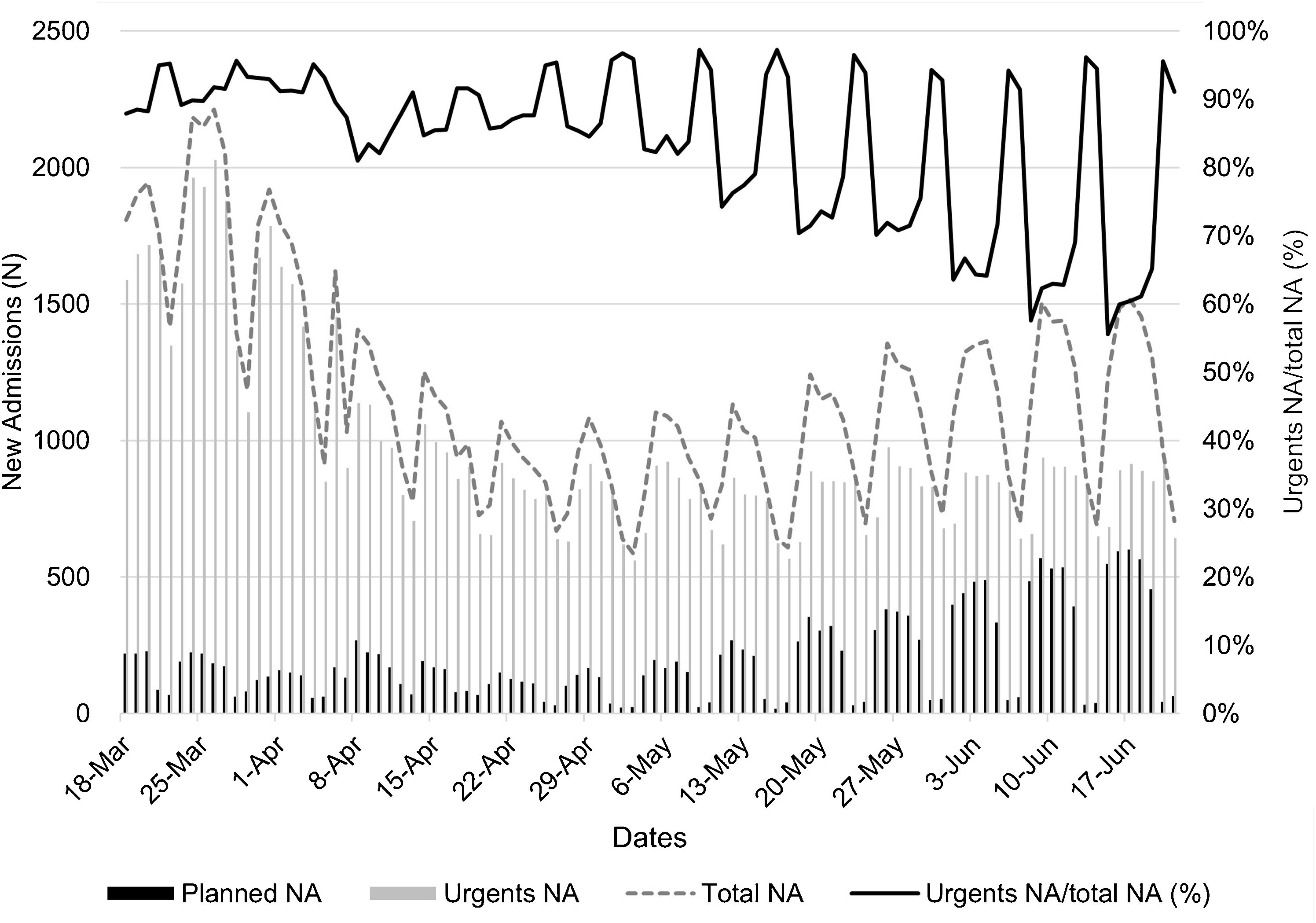
ResultsCompared to pre-pandemic years, during the maximum care pressure period (18 March–17 April 2020), the average number of total available and occupied beds increased by 27% and 36%, respectively. Also, the average number of available and occupied ICU beds increased by 174% and 257% respectively, and average occupancy was 81%. The average daily NAs were 1,503 (90% from the ED) and 949 (63% due to COVID-19), and of these, 61 (6.4%) were admitted to the ICU. On average, at 6:00p.m., 1112 patients were waiting in the ED to be admitted and 299 (26.8%) patients waited for more than 24h. Discharges due to death for COVID-19 inpatients in the non-ICU and ICU wards were 16% and 36%, respectively.
ConclusionsThis study confirmed the critical role of the ICU and ED, especially in the care of patients before being hospitalizated, in pandemic or health crisis scenarios.
La primera ola producida por SARS-CoV-2 ejerció mucha presión sobre el sistema sanitario. Los hospitales de la Comunidad de Madrid reestructuraron sus espacios y aumentaron su capacidad para atender la alta demanda asistencial.
MétodosEstudio observacional retrospectivo realizado entre el 18 de marzo y el 21 de junio de 2020, con datos de hospitales públicos y privados. Se calculan las frecuencias absolutas y relativas de pacientes hospitalizados con y sin COVID-19, camas disponibles y ocupadas en la unidad de cuidados intensivos (UCI) y no UCI (NUCI), de nuevos ingresos (NI) diarios, de pacientes en espera de ingreso en el servicio de urgencias (SU) y de las altas.
ResultadosCon respecto al período prepandemia, entre el 18 de marzo y 17 de abril de 2020 (período de máxima presión hospitalaria), el promedio de camas disponibles y ocupadas aumentó un 27% y 36%, respectivamente. Así mismo, las camas UCI crecieron un 174% y un 257%, respectivamente, con una ocupación media del 81%. La media diaria de NI fue de 1.503 (90% desde SU), y 949 (63%) por COVID-19, de los cuales 61 (6,4%) ingresaron en UCI. De media, a las 18:00 horas, 1.112 pacientes esperaban en SU para ingresar y 299 (26,8%) superaban las 24 horas de espera. Los fallecimientos en hospitalizados por COVID-19 en NUCI y UCI fueron del 16% y del 36%.
ConclusionesEste estudio reafirma el papel crítico de las UCI y los SU, especialmente atendiendo a los pacientes hasta su hospitalización, en situaciones de pandemia u otras crisis sanitarias.