Uninsured populations have poor treatment engagement and are less likely to receive evidence-based interventions for depression. The objective of the current study was to retrospectively examine depression screening, diagnosis, and treatment patterns among uninsured patients in primary care. Study sample included all patients (N=11,803) seen in nine community-based clinics. Key variables included depression screener and/or a depression diagnosis, anti-depressant initiation, behavioral health visits, and patient follow up measures. Treatment patterns from the subsample of patients diagnosed with depression were analyzed by collecting the number of behavioral health visits and antidepressant use six months (180 days) following the diagnosis. Utilization of the depression screening tool was high (67%, n=7,935) and 24% (n=2,789) of the patients had a diagnosis of depression, however, more than half of the patients with a depression diagnosis did not have a recorded treatment plan (n=1,474). The odds of anti-depressant use and behavioral visits for Hispanic patients were significantly greater than for Non-Hispanic patients. Universal screening with brief measures in primary care is improving, however, guideline-concordant depression treatment remains elusive for uninsured populations.
Poblaciones sin seguro médico tienen un compromiso deficiente con el tratamiento médico y menos probabilidad de recibir intervenciones basadas en evidencia para la depresión. El objetivo fue examinar retrospectivamente detección, diagnóstico y tratamiento de depresión entre pacientes sin seguro médico en Atención Primaria. Se incluyó a pacientes (N=11.803) atendidos en nueve clínicas comunitarias. Las variables fueron detección de depresión y/o diagnóstico de depresión, inicio del consumo de antidepresivos, visitas al proveedor de salud mental y medidas de seguimiento. Los planes de tratamiento de una submuestra de pacientes con depresión se analizaron mediante la recopilación del número de visitas a salud mental y uso de antidepresivos durante seis meses después del diagnóstico. La utilización de la herramienta de detección de depresión fue alta (67%, n=7.935) y 24% (n=2.789) en pacientes diagnosticados de depresión. Más de la mitad de los pacientes no tenían plan de tratamiento registrado (n=1.474). Las probabilidades de uso de antidepresivos y visitas a proveedores de salud mental para pacientes hispanos fueron mayores que para pacientes no hispanos. La detección universal con medidas breves en Atención Primaria está mejorando, pero el tratamiento de la depresión sigue siendo difícil de alcanzar para poblaciones sin seguro.
Depression or Major Depressive Disorder (MDD) is a chronic medical condition affecting a person’s mood, behavior, and ability to function (American Psychiatric Association, 2013). Adults with chronic medical conditions have higher rates of depression which impair the patient’s adherence to prescribed treatments. Similarly, depression increases the burden of chronic illness causing additional impairment in functioning and increasing medical cost (American Psychiatric Association, 2013; Unützer et al., 2006). Patients often seek care for depression from their primary care provider because of a trusting relationship, better communication and, ultimately, less stigma (Wang et al., 2006; Wun et al., 2011).
Diagnosis and treatment of depression is conducted in a variety of primary care and general medical settings. In spite of established guidelines, only 4.20% of patients are screened for depression in general primary care settings (Akincigil & Matthews, 2017). The most common tool used for preliminary screening for depression in primary care settings is the Patient Health Questionnaire-2 (PHQ-2) which consists of two items assessing for the anchor symptoms of depression: depressed mood and anhedonia (Kroenke et al., 2003). The American Psychiatric Association Academy of Psychosomatic Medicine recommends primary care settings use consistent disease assessment, tracking, and treatment to achieve optimal outcomes (American Psychiatric Association & Academy of Psychosomatic Medicine, 2016).
Measurement Based Care (MBC) for the treatment of depression includes the systematic measurement of symptoms, antidepressant side effects, and medication adherence to understand the burden of disease and progress of treatment (American Psychiatric Association & Academy of Psychosomatic Medicine, 2016). Ample evidence has demonstrated the effectiveness of MBC in achieving depression remission, in psychotherapy and medication intervention, through routine feedback from the patient to the clinician (Gelenberg et al., 2010). Despite evidence supporting the efficacy of MBC, data suggest that less than 20% of behavioral health providers utilize MBC to assess for treatment response in their practices (Lewis et al., 2019).
The objective of the current study was to retrospectively examine depression screening, diagnosis, and treatment patterns for patients in primary care practices that serve uninsurerd patients in a large health care system. The analysis was conducted using data extracted from the Electronic Health Record (EHR) for patients seen in the nine clinics.
MethodStudy design and participantsObservational data for this retrospective analysis included patients seen at nine community-based clinics supported by a large non-profit health system in Texas established to increase access to health services, provide quality care, and improve health outcomes for medically underserved populations discharged from the hospital. More than 17 full-time physicians and nurse practitioners provide care to nearly 12,000 unduplicated patients per year, with 4,500 of those being new patients. The clinics provide care to uninsured patients from the community. The patient population is 63% Hispanic, a majority of whom do not speak English, and 21% Black. Each clinic employs one licensed behavioral health provider.
Data was extracted from the EHR system (Epic) and included any patient seen at the nine clinics from January 2017 to December 2017. To ensure an accurate window of follow up data collection, a secondary extraction of data from January 2018 to July 2018 included the frequencies of anti-depressant use, behavioral health visits, and depression measures collected for patients diagnosed with depression in 2017. The study was reviewed and approved by the Institutional Review Boards of the health system and the University of Texas at Arlington.
MeasuresThe Patient Health Questionnaire-2 (PHQ-2) has been validated as a screening tool in the United States since 2003 with good specificity and sensitivity for depression throughout the general adult population (Kroenke et al., 2003). If a patient screens positive for symptoms of depression on the PHQ-2, the patient is then given the full Patient Health Questionnaire-9 (PHQ-9; Kroenke et al., 2003). It is the standard of practice in the clinics for the physician, nurse practitioners, and the licenced behavioral health provider to conduct a diagnostic interview using a checklist to confirm the presence of sufficent symptoms to meet the diagnostic criteria for depression (American Psychiatric Association, 2013). A diagnosis of depression in the EHR was identified using the recorded ICD-10 (2017) code in Epic. A list of specific ICD-10 (2017) codes were created and used to generate a list of patients with a depression diagnosis including F32.X, F33.X, F34.X, and F41.X.
The treatment of depression was defined as the accurate documentation in Epic of an antidepressant and/or behavioral health visit at the clinic. A list of commonly used anti-depressants was used to identify patients treated and included the following terms (generic names): sertraline, fluoxetine, citalopram, escitalopram, paroxetine, fluvoxamine.
Data analytic approachDescriptive statistics included frequencies (percentages) and means (standard deviations). Bivariate comparisons were conducted with chi-squared test for categorical measures and outcomes. Use of MBC was assessed from PHQ-9 data, antidepressant initiation, and behavioral health visits recorded within six months of the first diagnosis of depression and was analyzed using multivariable logistic regression adjusting for patient demographic variables including age, gender, race, and Charlson Comorbidity Index (Charlson et al., 2008).
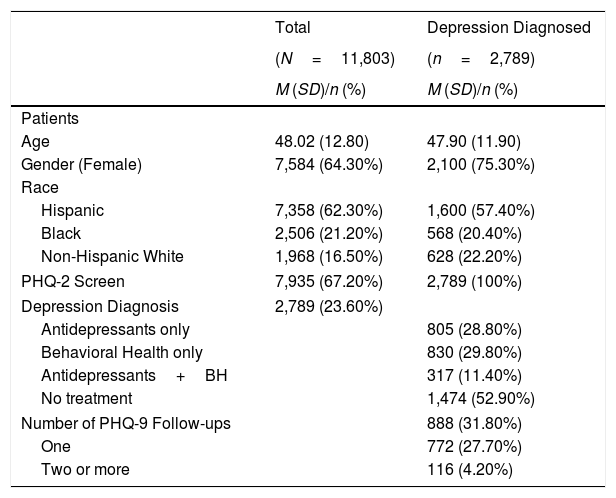
ResultsThe overall study sample included the 11,803 patients seen at the nine BCC clinics within the 2017 calendar year. The average age was 48 years old, 64.30% (n=7,584) of the study sample were female and 62.30% (n=7,358) of the sample identified as Hispanic (Table 1).
Patient characteristics, screening, diagnosis, and follow-up visits.
| Total | Depression Diagnosed | |
|---|---|---|
| (N=11,803) | (n=2,789) | |
| M (SD)/n (%) | M (SD)/n (%) | |
| Patients | ||
| Age | 48.02 (12.80) | 47.90 (11.90) |
| Gender (Female) | 7,584 (64.30%) | 2,100 (75.30%) |
| Race | ||
| Hispanic | 7,358 (62.30%) | 1,600 (57.40%) |
| Black | 2,506 (21.20%) | 568 (20.40%) |
| Non-Hispanic White | 1,968 (16.50%) | 628 (22.20%) |
| PHQ-2 Screen | 7,935 (67.20%) | 2,789 (100%) |
| Depression Diagnosis | 2,789 (23.60%) | |
| Antidepressants only | 805 (28.80%) | |
| Behavioral Health only | 830 (29.80%) | |
| Antidepressants+BH | 317 (11.40%) | |
| No treatment | 1,474 (52.90%) | |
| Number of PHQ-9 Follow-ups | 888 (31.80%) | |
| One | 772 (27.70%) | |
| Two or more | 116 (4.20%) | |
Of the 11,803 patients seen at the nine clinics, 67.20% (n=7,935) had a record of PHQ-2 and, after conducting a diagnostic interview, 23.60% (n=2,789) were diagnosed with depression in 2017. Of the 2,789 patients diagnosed with depression in 2017, 57.40% (n=1,600) of the patients identified as Hispanic and 42.60% (n=1,189) were non-Hispanic (Table 1). The odds of receiving a PHQ-2 screening for Hispanics was 26 % more than non-Hispanics (p<.0001). The odds of a depression diagnosis for Hispanic patients was 24% less than non-Hispanic patients (p<.0001).
Of the 2,789 patients with a depression diagnosis, 29% (n=805) received anti-depressant treatment only, 30% (n=830) received behavioral health visits only, and 11% (n=317) received both antidepressant and behavioral health visits. Fifty-three percent (n=1,471) of the patients had no treatment recorded (Table 1). Within six months of their first recorded depression diagnosis in 2017, the liklihood of anti-depressant use for Hispanic patients was 30% greater than it was for non-Hispanic patients (p=.002). The odds of behavioral visit use for Hispanic patients was 19% greater than the odds of behavioral health visit use for Non-Hispanic patients (p=.04).
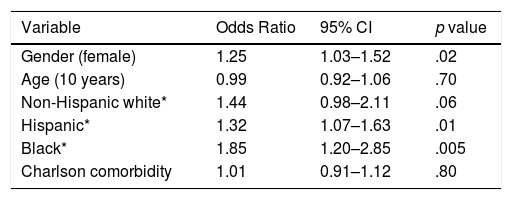
Follow-up assessmentsOf all the patients with a depression diagnosis in the sample, 888 (31.80%) had a follow up PHQ-9 recorded within six months after the first records of depression diagnosis. About 28% (n=772) had only one subsequent follow-up PHQ-9 and only 4% (n=116) of the patients with a depression diagnosis had two or more counts of a follow-up PHQ-9 (Table 1). In the adjusted models, the odds of behavioral health visit within six months of depression diagnosis for Hispanic patients were 32% more than that of non-Hispanics (OR = 1.32, CI: 1.07-1.63) (Table 2).
Logistic regression on behavioral health visits within 180 days of depression diagnosis.
| Variable | Odds Ratio | 95% CI | p value |
|---|---|---|---|
| Gender (female) | 1.25 | 1.03–1.52 | .02 |
| Age (10 years) | 0.99 | 0.92–1.06 | .70 |
| Non-Hispanic white* | 1.44 | 0.98–2.11 | .06 |
| Hispanic* | 1.32 | 1.07–1.63 | .01 |
| Black* | 1.85 | 1.20–2.85 | .005 |
| Charlson comorbidity | 1.01 | 0.91–1.12 | .80 |
Note. * a binary variable.
National rates of depression screening in primary care remain very low, with racial minorities half as likely to be screened compared with whites (Casey, 2013). In the current study, however, the overall screening rate with PHQ-2 was substantially higher at 67%, suggesting that implementation of EHR technology has likely enhanced routine screening at intake. Interetsingly, the odds of being screened was higher for Hispanic patients, yet they were less likely to actually be diagnosed with depression in comparison non-Hispanic patients, differences which may reflect language barriers in symptom measurement and persistent gaps in access to quality depression care and disparities in receipt of treatment (Akincigil & Matthews, 2017). Our previous work on symptom measurement among Hispanics in primary care characterized the specific manifestation of depression in a Hispanic population, with the single item related to fatigue showing the greatest varaition across groups (Killian, Sanchez, Eghaneyan, Cabassa, & Trivedi, 2021). It is important to note that while the PHQ-9 can be used to alert clinicians for evidence of disease, it cannot distinguish between differential depressive disorders nor can it confirm the diagnosis itself. Consideration of the use of additional screening tools, especially in Hispanic populations, could prove helpful for differentiating between disorders, such as anxiety, and may help shift clinical focus away from negative symtomotology to positive mental health (Guillot-Valdés et al., 2019; Teismann et al., 2019).
There was no significant difference between the portion of patients treated with antidepressants compared to behavioral health which is encouraging since patients with depression disorders often express a preference for counseling over pharmacological treatment (McHugh et al., 2013). However, more than half of patients with a depression diagnosis did not have a treatment plan recorded in the EHR. While it is possible that patients were referred to specialty care, that was not evident from the medical record. This finding is congruent with a recent analysis of depression treatment initiation patterns among primary care settings across five large, integrated US healthcare systems which reported only 35.70% of new episodes of diagnosed depression initiated antidepressant medication and/or psychotherapy, with all racial and ethnic minority groups having significantly lower odds of starting treatment, and the average delay in initiation of treatment being 6-8 years (Waitzfelder et al., 2018).
In the current analysis, Hispanic patients diagnosed with depression were more likely to use anti-depressants and had greater odds of behavioral health visits compared to non-Hispanic patients which contrasts with large health system data studies reporting that the odds of treatment initiation for Asians, non-Hispanic blacks, and Hispanics to be 30% lower than for non-Hispanic whites (Waitzfelder et al., 2018). Inclusion of the behavioral health provider on the primary care team can address significant barriers to treatment such as stigma, limited knowledge of mental health disorders, and treatment engagement and adherence, which disproportionately affect racial and ethnic minorities (Kahalnik et al., 2019; Siu et al., 2016), and was likely a factor in this study, though those gains may be limited in reach in low resource settings.
Only one-third of the patients with a depression diagnosis had a follow up PHQ-9 score recorded within six months of the first diagnosis, which reflects nonadherence to evidence-based treatment guidelines. Without proper documentation of regular quantitative assessment of symptoms and provider adjustment of the treatment plan in response to symptoms, trends in a single patient’s remission, relapse, and recovery cannot be assessed (Trombello et al., 2017). Even if a patient with depression reaches remission of depressive symptoms, they may have a relapse of symptoms or develop a new episode of depression. Further, the more failed treatment attempts a patient has, the higher the chances are of relapse. Active and routine measurement of depressed patients can help the clinician identify those at greatest risk for relapse (Lewis et al., 2019) and trends of the overall clinic population and depression management can be tracked.
Barriers to effective implementation of MBC include patient concerns about breach of confidentially, provider belief that measurement is inferior to clinical judgment, lack of resources for MBC training, and finally, competing clinical priorities (Kahalnik et al., 2019; Lewis et al., 2019). Opportunities for improving measurement include harmonizing EHRs and technology support to encourage MBC practices, prompts and reminders to set follow up appointments and to remind clinicians to collect follow up PHQ-9 scores within those appointments could be especially beneficial if integrated within EHR systems (Fortney et al., 2017).
This study has some limitations largely attributable to the data extracted from the EHR. Epic was implemented in the community clinics in 2017, so patient data prior to 2017 was not available. Additionally, data which may have been inaccurately documented, such as imbedded within clinician notes (primary and behavioral health), could not be extracted and accounted for in the analysis. In determining follow-up variables, it is possible that the patients failed to keep a scheduled appointment. In spite of these limitations, the EHR data revealed important depression screening, diagnosis, treatment and measurement patterns.
ConclusionsOver the past decade, robust research has demonstrated the gaps in care for low-income racial and ethnic minority groups in spite of incentives for primary care clinics with reimbursements for annual screening. Findings from this study demonstrate improved screening, diagnosis, and treatment initiation for patients with depression, however, there is substantial need for better implementation of MBC guidelines and consistent documentation of follow up PHQ-9 in the EHR. Routine measurement of depression symptoms should guide treatment decisions. Understanding the unique qualities, and potential reach, of behavioral health providers in community-based clinics has important implications for closing disparity gaps in depression treatment.
Future research should evaluate facilitators and barriers to implementing evidenced based interventions while incorporating technology solutions for decision support in the EHR. The practice transformation necessary for broad implementation of evidence-based depression screening and treatment guidelines into practice will require analysis of the contextual factors to overcome barriers, especially those related to organizational readiness and mechanisms to support implementation and sustain integrated behavioral health programs.