Research on selective mutism (SM) has been limited by the absence of standardised, psychometrically sound and cross-culturally valid assessment measures. Our aim is to present the results of a study of the factor structure and the reliability and concurrent validity of the scores of the Selective Mutism Questionnaire (SMQ), translated and adapted into Spanish. The SMQ contains 17 items about children's difficulty in speaking adequately in the family, school and social environment (out-of-school and out-of-family), each of which is answered according to a Likert scale with four response alternatives on speech frequency. Method: The study involved 110 pairs of parents of children diagnosed with SM whose ages ranged from 3 to 10 years. Results: The results show that the data from the Spanish sample fit the factorial model obtained by Bergman et al., and that data on its reliability and validity are robust and confirm that it as a good instrument for assessing SM in Spanish-speaking children. Conclusions: Therefore, we can affirm that the SMQ is a good instrument to assess SM in Spanish-speaking children.
La investigación sobre el mutismo selectivo (MS) se ha visto limitada por la ausencia de medidas de evaluación estandarizadas, psicométricamente sólidas y con validez transcultural. Nuestro objetivo es presentar los resultados de un estudio de la estructura factorial, fiabilidad y validez concurrente de las puntaciones del Selective Mutism Questionnaire (SMQ), traducido y adaptado al español. El SMQ contiene 17 ítems sobre la dificultad de los niños para hablar adecuadamente en el ámbito familiar, escolar y social (extraescolar y ajeno al ámbito familiar), cada uno de los cuales se contesta según una escala tipo Likert con cuatro alternativas de respuesta sobre la frecuencia del habla. Método: En el estudio participaron 110 parejas de padres de niños y niñas diagnosticados con MS. Resultados: Los resultados muestran que los datos de la muestra española se ajustan al modelo factorial obtenido por Bergman et al., así como que los datos sobre su fiabilidad y la validez son robustos. Conclusiones: Por todo ello podemos afirmar que el SMQ es un buen instrumento para valorar el MS en niños y niñas españoles de habla castellana.
Selective mutism (SM) is a child behavior disorder characterized by the partial or complete absence of speech in specific social situations, despite the fact that in other situations, children make adequate use of speech. According to the Diagnostic and Statistical Manual of Mental Disorders (DSM-5; American Psychiatric Association, 2013), for the diagnosis of SM, lack of speech must cause interference, last at least 1 month, and not be produced by lack of knowledge of the language spoken in the place where one lives. Despite its low prevalence (less than 1% of the school population; American Psychiatric Association, 2013), SM is considered a disabling disorder that interferes with school learning and alters the child's socialization process, in addition to generating a high level of subjective suffering and being the origin of a high number of comorbid disorders (Cornacchio et al., 2019; Steffenburg et al., 2018)
Among variables hindering SM assessment and treatment research is the scarcity of standardized measurement instruments that assess the altered responses associated with the disorder and that have cross-cultural validity. In fact, we currently only have one test with verified psychometric properties, the Selective Mutism Questionnaire (SMQ; Bergman et al., 2008), which is not validated for use with Spanish-speaking populations.
As recalled by Bergman et al. (2008), prior to the development and validation of SMQ, researchers evaluated MS-related behavioral problems without quantifying the altered responses specific to the disorder. Until the advent of SMQ, researchers who had studied the diagnosis of SM, its phenomenology, or the outcomes of its treatment had not addressed the design, development, and validation of a standardized measure of speech frequency and intensity that would also allow for estimation of the interference and distress produced by this disorder.
The lack of an instrument of this nature has conditioned and reached more relevance in the context of the evaluation of the psychological treatment of this disorder. Not having a tool that produces reliable and valid scores has hindered comparison of results between different studies, as well as the possibilities of replicating findings (Driessen et al., 2020).
In addition, given the phenomenological overlap between SM and social anxiety disorder (SAD), measures of the latter such as those provided by the Social Anxiety Scale for Children-Revised (SASC-R; LaGreca & Stone, 1993) or the Multidimensional Anxiety Scale for Children (MASC) in their adaptations for parents (Olivares & Olivares-Olivares, 2018), despite being relevant for the study of SM, do not evaluate its main characteristics, such as not speaking in certain situations (Johnson & Wintgens, 2017).
Therefore, although being necessary to better understand SM, they are not sufficient. In other words, they cannot replace the information provided by a parental measure that quantifies the frequency of speech in functional domains that are decisive in guiding clinical diagnosis, as made possible by SMQ (Oerbeck et al., 2020).
This situation prevents the development of studies that allow relationships between variables to be established and the effectiveness of treatments to be quantified more rigorously, as has been done, for example, in the TAS (Gómez-Ortiz et al., 2019; Neufeld et al., 2020). Moreover, the SMQ is an instrument that has already proven useful in distinguishing children with SM from those with SAD or other anxiety disorders, as well as from controls without psychological disorders (Olivares & Olivares-Olivares, 2018).
For these reasons, we understand that the translation, adaptation and psychometric validation of the original SMQ version (Bergman et al., 2008) into Spanish is necessary, since we currently possess no instrument of these characteristics validated to evaluate the SM. Our objectives are (1) to study the factorial structure of the SMQ in a Spanish sample of children with SM, (2) to examine its reliability, and (3) to verify its concurrent validity.
MethodParticipantsThe participants are parents whose children were referred for diagnosis from different clinical centers and specialists, as well as by personal searches through the web page of our research group (https://www.um.es/grupos/grupo-fobiasocial/cientifico.php), to the Behavior Therapy Unit (UTECO) of the Faculty of Psychology of the University of Murcia.
After the diagnosis of the children by clinical psychologists with experience in the evaluation and treatment of selective mutism, following the DSM-5 diagnostic criteria, parents were included or excluded from the sample that completed the SMQ (and the rest of the tests) based on the following criteria:
Inclusion: that it had been verified during the diagnosis of the child that the persistent lack of speech in specific social situations, despite speaking correctly in other situations (according to their age), this lack of speech caused interference, lasted at least 1 month and was not due to a lack of knowledge of the language spoken in the social situation neither by the parents nor by the child.
Exclusion: the diagnosis verified that the child met the criteria for separation anxiety disorder, for a communication disorder (such as stuttering, for example), for an autism spectrum disorder, or for a diagnosis of schizophrenia or other psychotic disorder.
The sample is composed of 110 pairs of parents of boys and girls, diagnosed with SM as the main disorder, with ages between 3 and 10 years (M = 6.60; SD = 1.98), an average delay of 1.70 years (SD = 1.25) between the memory of the beginning of the disorder and its evaluation at UTECO; 64.5% of the sample were girls. The mean parent-reported clinical severity ratio in ADIS-IV-C/P was 5.61 (SD = 1.04; range: 4 minimum - 8 maximum).
With regard to speech, 70.90% were monolingual (61.8% Spanish from Spain and 9.1% from Latin America). In 7.3% of cases, the Spanish mother tongue was different from the area of Spain in which they lived (Spanish speaking family in Galician, Basque or Catalan speaking areas and vice versa). For 21.8% their mother tongue was another European language different to that spoken in their area of residence.
Of the total number of children in the sample, 13.6% had a family history of SM. In addition, 15.5% of the children with MS who participated in the study consumed anxiolytics and other drugs which had been prescribed by the family doctor and/or pediatrician.
The children in this sample presented comorbidity with other disorders in the following proportions: specific phobia (45.5%), separation anxiety disorder (30%), generalized anxiety (10%), panic attacks (3.6%), tics (9.1%), enuresis (21.80%), encopresis (12.7%), oppositional defiant disorder (12.7%), obsessive-compulsive disorder (10%), attention-deficit/hyperactivity disorder (10%), depression (7.3%) and speech and language disorder (8.2%).
MeasuresDiagnostic evaluation was conducted through a clinical interview (Silverman et al., 2003) and four questionnaires for parental reporting measures were self-administered. The order in which the instruments were applied was as follows:
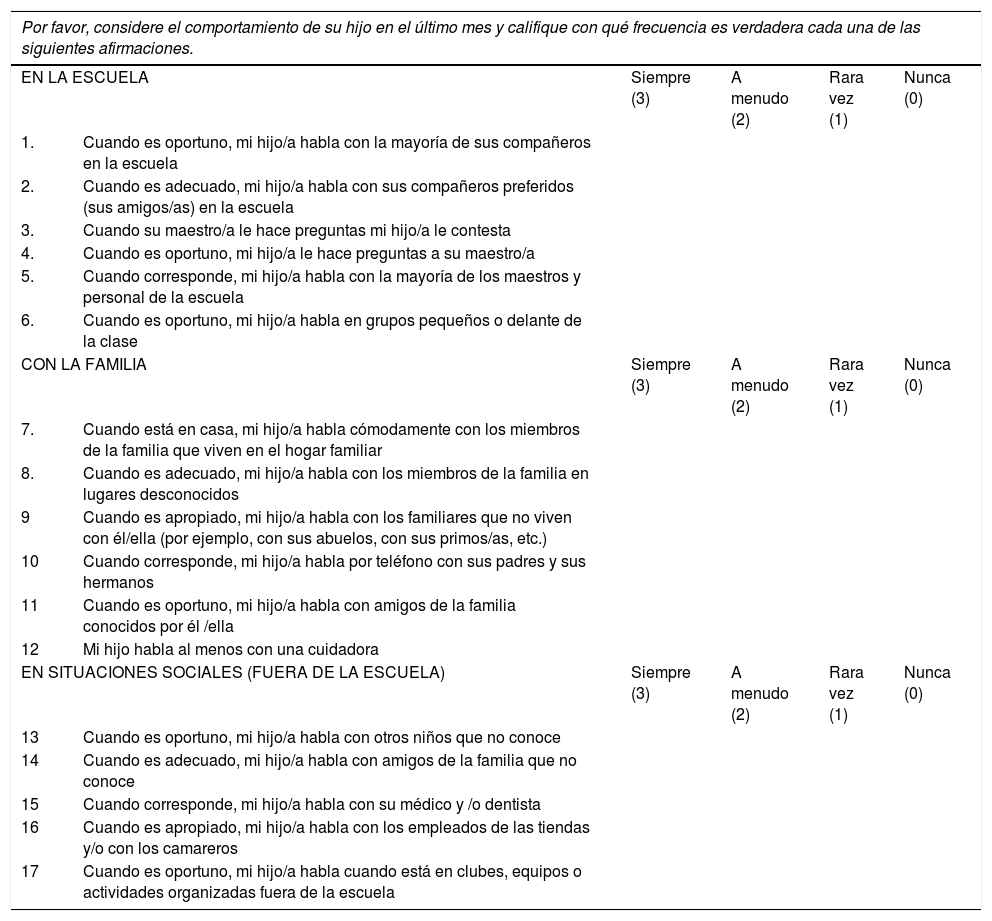
Selective Mutism Questionnaire (SMQ; Bergman et al., 2008). It quantifies the behavior of the child with SM through 17 items that parents value, on three subscales: home, school, and out-of-school social situations. Each item includes four possible responses (0 = Never, 1 = Rarely, 2 = Frequently, 3 = Always); the lower the score the greater the severity and interference. The results support its convergent and discriminant validity (Letamendi et al., 2008); the internal consistency is acceptable and sensitive to the effects of treatment (Bergman et al., 2013). Two native Spanish speakers who were proficient in English independently translated the original version into Spanish. An evaluation was carried out to determine whether the items drafted in Spanish were clearly and unambiguously written in language appropriate to the potential target population. Finally, the consensus version was blind back-translated by a bilingual native English speaker and, in order to ensure semantic equivalence, it was subsequently compared with the original version and validated by the authors of the spanish translation of the SMQ.
The Social Anxiety Scale for Children-Revised-Parent (SASC-R-P; LaGreca & Stone, 1993). The SASC-R-P is a parent-reported measure of children's social anxiety, adapted from the Social Anxiety Scale for Children-Revised. The scale consists of 18 items with three response alternatives: Never, Sometimes, and Often. It includes three factors or subscales: SASC-R-FNE-P (Fear of Negative Evaluation), SASC-R-SADG-P (Social anxiety and avoidance in the face of general people), and SASC-R-SADN-P (Social anxiety and avoidance in the face of strangers). Bergman et al. (2013) reported good reliability (Cronbach's alpha = .87) for their English versión. In this study the internal consistency coefficients of the scale and subscales scores have been: .99 (SASC-R-P), .98 (SASC-R-FNE-P), .95 (SASC-R-SADG -P) and. 97 (SASC-R-SADN-P); the test-retest reliability coefficients were .99 in SASC-R-P, .99 in SASC-R-FNE-P, .96 in (SASC-R-SADG-P) and .98 in (SASC-R-SADN-P).
The Multidimensional Anxiety Scale for Children-Parent (MASC-P; March et al., 1997). The MASC-P is a measure of childhood anxiety of 38 items completed by parents (Kovacs, 1992; March et al., 1997). Baldwin and Dadds (2007) found that ASM-P has a factorial structure similar to the child version of this measure. It includes four subscales or factors: MASC-P-SF (physical symptoms); MASC-P-ASE (Separation/panic anxiety); MASC-P-ASO (Social anxiety); MASC-P-ED (Avoidance of harm/distress). Studies using MASC-P showed high test-retest reliability, good convergent and divergent validity, and high internal consistency in all four subscales (Palitz et al., 2018). In this sample, the coefficients of internal consistency were: .85 (MASC-P), .74 (MASC-P-SF), .96 (MASC-P-ASE), .84 (MASC-P-ASO) and. 72 (MASC-P-ED); the test-retest reliability coefficients were: .97 (MASC-P), .94 (MASC-P-SF), .97 (MASC-P-ASE), .97 (MASC-P-ASO), and .94 (MASC-P-ED).
The Children's Depression Inventory-Short-Parent (CDI-S-P; Olivares-Olivares & Olivares, 2014). The CDI-S-P is the parent's adaptation of the abridged version of the CDI-S (Kovacs, 1992). It consists of 10 items, each comprising three phrases or sentences that describe an intensity gradient evaluated according to a Likert type scale (range: 0-2). The children's version was validated for use in Spanish-speaking populations, showing good internal consistency in all studies conducted (Ventura-León et al., 2020). In this study the internal consistency of the CDI-S-P scores is .92 and the test-retest reliability coefficient was .98.
Anxiety Disorders Interview Schedule. Parents Interview Schedule, ADIS-IV: P (Silverman et al., 2003). This allows for parental assessment of anxiety disorders and detection of other associated disorders. In addition, it was verified that the children's behavior met the DSM-5 (American Psychiatric Association, 2013) criteria for SM diagnosis, since the ADIS-IV (American Psychiatric Association, 1994) did not consider it an anxiety disorder. The scale has shown good test-retest and inter-judge reliability, as well as good convergent validity with other self-report measures of anxiety (see Palitz et al., 2018).
ProcedureThis research was authorized by the Clinical Research Ethics Committee (CEIC) of the University of Murcia. All parents of children referred for evaluation and differential diagnosis of their child's presenting disorder were asked to complete the four questionnaires and clinical interview described in the Measures section to specify or exclude the primary diagnosis of SM. In order to perform the necessary calculations, test and retest measurements were carried out. In instructions prior to completion of questionnaires, parents were informed that, since both were required to come to be attended to, in the event of a conflict in the most appropriate response to some item, the opinion of the person who spent most time with the child on a daily basis would prevail.
Data analysisSPSS v. 25.0 was used for the descriptive sample study, internal consitency, concurrent and predictive validity. To check the factorial structure of the SMQ, a confirmatory factor analysis (CFA) with MPLUS v. 8.4 (Muthen & Muthen, 2012) was performed, using the robust weight least squares estimation (WLSMV). The goodness-of-fit indexes of the data to the modeland their cutoffs used were, the approximation mean square error (RMSEA) equal to or less than 0.08, the comparative fit index (CFI) equal to or greater than 0.95, and the Tucker-Lewis fit index (TLI) equal to or greater than 0.95 (Brown, 2006).
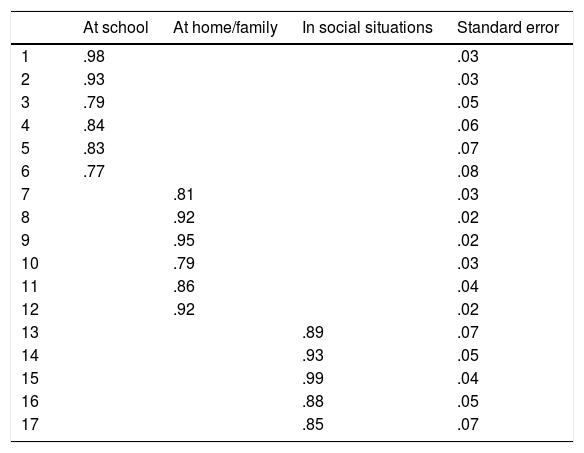
ResultsValidity evidence based on internal structureThe goodness-of-fit indexes have been: RMSEA = .044, CFI = .992 and TLI = .991. These values show a good fit of the data to the model. The factor loadings are high (Table 1), ranging from .77 of item 6 to .99 of item 15, these values support the fit of the data to the three-factor model.
The correlations between the scores of the three factors were SMQ-at-school and SMQ-at-home/family equal to .68, between SMQ-at-school and SMQ-social situations equal to .19, and between SMQ-at-home/family and SMQ-social situations equal to .50.
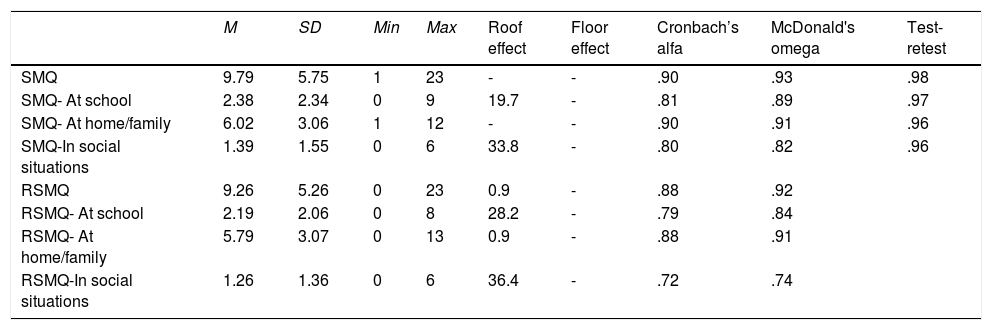
ReliabilityTable 2 contains the mean, standard deviation, minimum and maximum scores, floor and ceiling effects, internal consistency coefficients (estimated internal consistency with Cronbach's alpha coefficient and McDonald's omega) and test-retest reliability of the scales and subscales.
Mean (M), standard deviation (SD), minimum (Min) and maximum (Max), floor and ceiling effects, internal consistency and MSQ test-retest reliability.
| M | SD | Min | Max | Roof effect | Floor effect | Cronbach’s alfa | McDonald's omega | Test-retest | |
|---|---|---|---|---|---|---|---|---|---|
| SMQ | 9.79 | 5.75 | 1 | 23 | - | - | .90 | .93 | .98 |
| SMQ- At school | 2.38 | 2.34 | 0 | 9 | 19.7 | - | .81 | .89 | .97 |
| SMQ- At home/family | 6.02 | 3.06 | 1 | 12 | - | - | .90 | .91 | .96 |
| SMQ-In social situations | 1.39 | 1.55 | 0 | 6 | 33.8 | - | .80 | .82 | .96 |
| RSMQ | 9.26 | 5.26 | 0 | 23 | 0.9 | - | .88 | .92 | |
| RSMQ- At school | 2.19 | 2.06 | 0 | 8 | 28.2 | - | .79 | .84 | |
| RSMQ- At home/family | 5.79 | 3.07 | 0 | 13 | 0.9 | - | .88 | .91 | |
| RSMQ-In social situations | 1.26 | 1.36 | 0 | 6 | 36.4 | - | .72 | .74 |
Note. SMQ = Results of the first application RSMQ = Results of the retest (one month later).
The lowest mean is that of subscale SMQ-social situations (M = 1.39, SD = 1.55 in the test, M = 1.26, SD = 1.36 in the retest), indicating a higher degree of SM in these situations than in the family environment, since the SMQ-at-home/family subscale is where the mean is the highest of the three subscales (M = 6.02, SD = 3.06 in the test, M = 5.79, SD = 3.07 in the retest). The mean of the SMQ-at-school subscale is between the two previous and its values are low (M = 2.38, SD = 2.34 in the test, M = 2.19, SD = 2.06 in the retest), indicating that it is also in this setting where children present the highest degree of SM.
In the study of the floor and ceiling effects of scores, a ceiling effect was observed in subscale SMQ-at-school and SMQ-social situations both in test and retest, being more noticeable in the latter. There was no floor effect in either application. A detailed analysis of response choices showed that categories 0-Never and 1-Rarely were those most chosen in almost all items, category 2-Frequently was chosen in only 50% of items, and category 3-Always was not marked in most items but when so did not receive a high choice rate (it was only selected for items 2, 3, 7 and 8).
The highest scores on the internal consistency are those corresponding to the SMQ and the SMQ-at-home/family subscale that reached a value of .90. The subscales SMQ-at-school and SMQ-social situations were those showing the lowest internal consistency in the second application of the questionnaire (retest), although all were higher than .70. McDonald's omega coefficient obtained acceptable values in the first application of the SMQ, it varied between .82 on the SMQ-social situations subscale and .93 on the total scale; for the retest, their values varied between .74 on the SMQ-social situations subscale and .92 on the total scale.
As for the study of temporal stability, high correlations were obtained between test and retest scores, above .95 in the SMQ and its subscales with one month between the two applications.
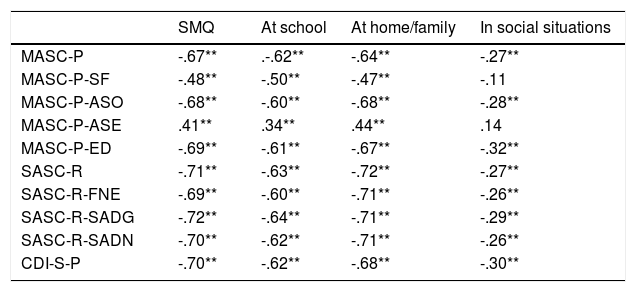
Concurrent validityTable 3 shows correlations between the SMQ and the other instruments applied in the sample. The interpretation of the SMQ scores is the lower the score the higher the degree of SM, while in the MASC-P, SASC-R and CDI-S-P scales the higher the score the higher the degree of anxiety and depression. Except for correlations between the SMQ and its subscales with the separation anxiety subscale evaluated with the MASC-P-AP which are positive, all correlations are negative and statistically significant; therefore, these results indicate that the higher the degree of SM the higher the levels of anxiety and depression. The highest correlations in absolute value were obtained between total scores in the SMQ and SMQ-at-school subscales and SMQ-at-home/family with the MASC-P-ASO subscale (r = -.68) which evaluates social anxiety, and with the SASC-R-SADG scale and subscales (r = -.72) which also evaluate avoidance and social anxiety. These results indicate that the higher the degree of SM, the higher the social anxiety. However, the SMQ-In Social Situations subscale obtained lower correlations in absolute value with all scales and subscales used, two of which were not statistically significant, those that evaluate anxiety from physical symptoms (MASC-P-SF r = -.11) and separation anxiety (MASC-P-AP, r = .14).
Correlations between the Selective Mutism Questionnaire, its subscales and other variables.
| SMQ | At school | At home/family | In social situations | |
|---|---|---|---|---|
| MASC-P | -.67** | .-.62** | -.64** | -.27** |
| MASC-P-SF | -.48** | -.50** | -.47** | -.11 |
| MASC-P-ASO | -.68** | -.60** | -.68** | -.28** |
| MASC-P-ASE | .41** | .34** | .44** | .14 |
| MASC-P-ED | -.69** | -.61** | -.67** | -.32** |
| SASC-R | -.71** | -.63** | -.72** | -.27** |
| SASC-R-FNE | -.69** | -.60** | -.71** | -.26** |
| SASC-R-SADG | -.72** | -.64** | -.71** | -.29** |
| SASC-R-SADN | -.70** | -.62** | -.71** | -.26** |
| CDI-S-P | -.70** | -.62** | -.68** | -.30** |
Notes. SMQ = Selective Mutism Questionnaire MASC-P = Multidimensional anxiety scale for Children-Parent MASC-P-SF = Physical symptoms MASC-P-ASE = separation anxiety), MASC-P-ASO (social anxiety) MASC-P-ED = harm avoidance SASC-R = Social Anxiety Scale for Children-Revised SASC-R-FNE = Fear of Negative Evaluation SASC-R-SADG = Social Anxiety and Avoidance in front of people in general SASC-R-SADN = Social Anxiety and Avoidance in front of Strangers CDI-S-P = Children's Depression Inventory-Short.
The SMQ correlations and its three subscales were positively correlated with the MASC-P-ASE one which evaluates separation-panic anxiety, in other words, high levels of SM are related to low separation anxiety.
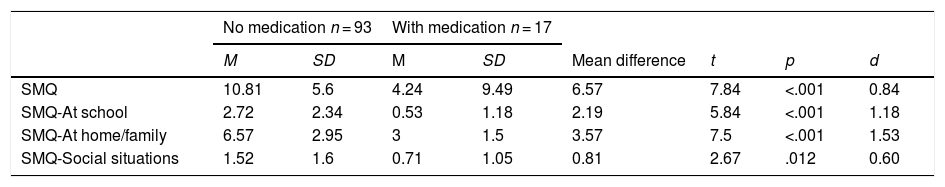
Predictive validityThe Student t test for independent samples showed no statistically significant differences in the means of SMQ and its subscales in either the sex variable or family history variable with SM. However, there was a statistically significant difference in the SMQ and its three subscales when comparing groups of boys and girls who take some type of medication or not: SMQ, t = 7.84, p < .001; SMQ-at-school, t = 5.84, p < .001; SMQ-at-family, t = 7.5, p < .001; SMQ-social situations, t = 2.67, p = .012. In all cases the means were higher in the group of children not taking medication, that is, their SM grade was lower (Table 4). The effect size indices are large for the scale and subscales.
Mean (M), standard deviation (SD) and test for comparison of means of the Selective Mutism Questionnaire and its subscales in the variable Consumption of psychotropics.
| No medication n = 93 | With medication n = 17 | |||||||
|---|---|---|---|---|---|---|---|---|
| M | SD | M | SD | Mean difference | t | p | d | |
| SMQ | 10.81 | 5.6 | 4.24 | 9.49 | 6.57 | 7.84 | <.001 | 0.84 |
| SMQ-At school | 2.72 | 2.34 | 0.53 | 1.18 | 2.19 | 5.84 | <.001 | 1.18 |
| SMQ-At home/family | 6.57 | 2.95 | 3 | 1.5 | 3.57 | 7.5 | <.001 | 1.53 |
| SMQ-Social situations | 1.52 | 1.6 | 0.71 | 1.05 | 0.81 | 2.67 | .012 | 0.60 |
A one-factor ANOVA to study differences in the spoken language variable showed statistically significant differences in the SMQ [F(3, 109) = 3.46 p = .019, ¿2 = .08] and the SMQ-at-school subscale [F(3, 109) = 6.06 p = .001, ¿2 = .14]. Two-to-two comparisons showed that these differences were among children whose native language is Spanish [median-SMQ = 10.93 (SD = 5.95), median-SMQ-In School = 2.96 (SD = 2.48)] and those whose mother tongue is a European language other than Spanish spoken in their area of residence [median-SMQ = 6.71 (SD = 3.98), median-SMQ-In School = 0.75 (SD = 0.95)]: mean difference-SMQ = 4.21 p = .011, and in the subscale mean difference-SMQ-In School = 2.20 p < .001.
DiscussionThe results of our research provide clear support for the psychometric properties of SMQ (Appendix A). It is confirmed that the factorial structure of the SMQ in this application is the same as that found by Bergman et al. (2008), therefore it can be stated that the solution of three factors is clearly interpretable. The confirmation of the three subscales already identified (Home/family, School and Social situations) shows the stability of the altered response pattern (clinical phenomenology) and allows us to evaluate the use of speech in the three categories of situations contemplated by the scale, as well as quantifying treatment response (if applicable). Results show the great impact of SM, from highest to lowest, on the children's speech in social situations, followed by school and finally the home, in line with that previously hypothesized in our tentative model (Olivares-Olivares & Olivares, 2018).
Regarding treatment, data from the English version (Bergman et al., 2013) and a previous version used experimentally in Spanish (Olivares et al., 2019) and those reported by Oerbeck et al. (2020) in Norwegian children with SM support the sensitivity of SMQ regarding treatment effects. Moreover, the results of the internal consistency and validity of SMQ and its subscales, show that it is a good instrument to assess SM in Spanish-speaking children. Results are also consistent with those reported by Letamendi et al. (2008) regarding concurrent validity.
In addition, results support the concurrent validity between the SMQ and the SAD. Taking the current phenomenological delimitation of the SM as reference, we can predict relatively robust relationships between the scores in the SMQ and in the TAS, measured with the SASC-R-P, the MASC-P-ASO or with other ad hoc scales. The same occurs with the CDI-S-P. The results we have obtained are consistent with those reported by Cummings et al. (2014) in their review of the relationships between anxiety and depression in research performed in the last 20 years.
There was absence of statistically significant differences in the comparison of the SMQ means and its three subscales in the sex variable. Neither did we find differences due to the presence of family history with MS, pointing out that more than a disorder produced by learning through modeling, or of genetic order, we are facing one most likely generated by classical conditioning and maintained by the positive reinforcement of adults and by the negative of escape/avoidance responses (Olivares-Olivares & Olivares, 2018). However, if we find differences between children with SM taking medication and those not, it reaches statistical significance in favor of the former. In other words, the intake of anxiolytic medication is not associated with minor SM impact reported by parents. This seems to indicate that even if anxiolytic medication reduces the intensity of anxiety responses, it does not improve the negative effects of SM in responses assessed in the questionnaire related to oral activity in school, family and social environment. In addition, differences were also observed between those whose mother tongue was Spanish and those who had another European language. Consequently, having a vernacular language different from that spoken where one resides is shown to be a vulnerability factor that enhances the degree of MS.
A limitation of this work is the small size of the clinical sample. Future research should increase the sample size.
Regarding the implications of our findings for future research and clinical practice, the following should be noted: one of them, analyze the factorial structure for a null model and a two-factor model. The reason for the latter is the high correlation of the factors At school and At home/family, which could be due to a bias in the evaluation of MS in the school context, since it is the parents who respond to the items to be evaluated in both environments. In this sense, it is convenient to carry out more research where these results are contrasted with those of the adaptation of the School Speech Questionnaire assessed by the teacher (Bergman et al., 2002), to discuss them both with those obtained in the SMQ and in other research (e.g., Oerbeck et al., 2020). Another one, study the convergent and discriminant validity.
Yet another, assessment of the diagnostic accuracy of SMQ with sensitivity and specificity analyzes, determinate of the cutoff and norms for clinical scores into groups in which there are differences (e.g., whether they take medication or not, as would be the case in this sample).
In future research, it would be convenient to test the diagnostic capacity of the SMQ and its sensitivity to quantify the effects of treatment in the Spanish population.
| Por favor, considere el comportamiento de su hijo en el último mes y califique con qué frecuencia es verdadera cada una de las siguientes afirmaciones. | |||||
|---|---|---|---|---|---|
| EN LA ESCUELA | Siempre (3) | A menudo (2) | Rara vez (1) | Nunca (0) | |
| 1. | Cuando es oportuno, mi hijo/a habla con la mayoría de sus compañeros en la escuela | ||||
| 2. | Cuando es adecuado, mi hijo/a habla con sus compañeros preferidos (sus amigos/as) en la escuela | ||||
| 3. | Cuando su maestro/a le hace preguntas mi hijo/a le contesta | ||||
| 4. | Cuando es oportuno, mi hijo/a le hace preguntas a su maestro/a | ||||
| 5. | Cuando corresponde, mi hijo/a habla con la mayoría de los maestros y personal de la escuela | ||||
| 6. | Cuando es oportuno, mi hijo/a habla en grupos pequeños o delante de la clase | ||||
| CON LA FAMILIA | Siempre (3) | A menudo (2) | Rara vez (1) | Nunca (0) | |
| 7. | Cuando está en casa, mi hijo/a habla cómodamente con los miembros de la familia que viven en el hogar familiar | ||||
| 8. | Cuando es adecuado, mi hijo/a habla con los miembros de la familia en lugares desconocidos | ||||
| 9 | Cuando es apropiado, mi hijo/a habla con los familiares que no viven con él/ella (por ejemplo, con sus abuelos, con sus primos/as, etc.) | ||||
| 10 | Cuando corresponde, mi hijo/a habla por teléfono con sus padres y sus hermanos | ||||
| 11 | Cuando es oportuno, mi hijo/a habla con amigos de la familia conocidos por él /ella | ||||
| 12 | Mi hijo habla al menos con una cuidadora | ||||
| EN SITUACIONES SOCIALES (FUERA DE LA ESCUELA) | Siempre (3) | A menudo (2) | Rara vez (1) | Nunca (0) | |
| 13 | Cuando es oportuno, mi hijo/a habla con otros niños que no conoce | ||||
| 14 | Cuando es adecuado, mi hijo/a habla con amigos de la familia que no conoce | ||||
| 15 | Cuando corresponde, mi hijo/a habla con su médico y /o dentista | ||||
| 16 | Cuando es apropiado, mi hijo/a habla con los empleados de las tiendas y/o con los camareros | ||||
| 17 | Cuando es oportuno, mi hijo/a habla cuando está en clubes, equipos o actividades organizadas fuera de la escuela | ||||
Note. The original English version is available at http://www.oxfordclinicalpsych.com/view/10.1093/med:psych/9780195391527.001.0001/med-9780195391527-interactive-pdf-002.pdf and at Bergman (2013).