The comorbidity of depression and fibromyalgia chronic syndrome has been well documented in the literature; however, the cognitive structure of these patients has not been assessed. Previous results reported variability in cognitive rigidity in depressive patients, the key for this might be the presence of chronic physical pain such as fibromyalgia. The present study explores and compares the cognitive rigidity and differentiation, between patients with depression with and without fibromyalgia syndrome.
MethodThirty one patients with depression and fibromyalgia were matched, considering age, sex and number of depressive episodes, with 31 patients with depression but without fibromyalgia diagnosis. Cognitive rigidity and differentiation were measured with the repertory grid technique.
ResultsThe results indicated that depressed patients with fibromyalgia presented higher levels of depressive symptoms, greater cognitive rigidity and lower cognitive differentiation than those without fibromyalgia.
ConclusionsThe results might inform future treatments to address the cognitive structure of these patients.
La comorbilidad de la depresión y la fibromialgia ha sido bien documentada en la literatura. Sin embargo, la estructura cognitiva de estos pacientes no ha sido evaluada. Estudios previos muestran variabilidad en medidas de rigidez cognitiva en pacientes con depresión. Los síndromes físicos crónicos podrían ser una variable clave para explicar esta variabilidad presente en estudios previos. El presente estudio explora y compara la rigidez y la diferenciación cognitiva entre paciente con depresión que tienen y aquellos que no tienen fibromialgia.
MétodoTreinta y un pacientes con depresión y fibromialgia fueron emparejados, considerando edad, sexo y números de episodios depresivos con 31 pacientes con depresión, pero sin diagnóstico de fibromialgia.
ResultadosLos resultados indican que los pacientes que presentan depresión y fibromialgia evidencian niveles más altos de síntomas depresivos, mayor rigidez cognitiva y menor diferenciación cognitiva que los pacientes sin fibromialgia.
ConclusionesEstos resultados podrían ser considerados al momento de crear tratamientos ajustados a la estructura cognitiva de estos pacientes.
Depressive disorder is one of the most severe health problems in our society because of its disabling effects, and societal and economic burden (Whiteford, Ferrari, Degenhardt, Feigin, & Vos, 2015). Moreover, it has been associated with several health issues (Brandolim Becker et al., 2018; Chen et al., 2019; Nieto, Hernández-Torres, Pérez-Flores, & Montón, 2018). An “all-or-nothing” thinking pattern (a tendency to extreme or catastrophic thinking) has been described as a core aspect of depressive cognition (Al-Mosaiwi & Johnstone, 2018; Antoniou, Bongers, & Jansen, 2017).
From a personal construct theory viewpoint, it has been suggested that depressed patients organize the construing of themselves, others and the world in relatively polarized, monolithic terms that are resistant to modification and revision (Neimeyer, 1985). In fact, using the Repertory Grid Technique (RGT) the configuration of the construct system in depressed patients has been defined as presenting high polarization (Neimeyer & Feixas, 1992) —the tendency of more extreme ratings— an low cognitive differentiation— measured by means of the percentage of variance accounted by the first factor (PVAFF; Kovářová & Filip, 2015) resulting from the analysis of each grid data matrix.
However, recent findings suggested similar mean, but also high variability, in polarization and in PVAFF between a group of depressed patients and a non-clinical group (Feixas, Erazo-Caicedo, Harter, & Bach, 2008). This result might be explained by the great amount of clinical variability among depressed patients. In fact, high rates of comorbidity with chronic syndromes related with pain have been reported (Velly & Mohit, 2018). Ohayon and Schatzberg (2003) indicated that around 43.4% of the individuals who met criteria for depression also had a chronic painful physical condition compared to 16.1% in the general population. Studies in fibromyalgia (FM) also showed a life-span prevalence of 90% of depressive symptoms, and a rate between 62 to 86% of comorbidity with a diagnosis of depression (Veltri et al., 2012). These rates were significantly higher compared with general population, and indeed, with other chronic pain disorders (Gormsen, Rosenberg, Bach, & Jensen, 2010).
The objective of the present study was to explore cognitive rigidity and differentiation in depressed patients and patients with comorbid FM. We hypothesized that participants with depression and fibromyalgia would have higher levels of depression, polarization and lower cognitive differentiation than participants with depression without fibromyalgia.
MethodParticipantsThis study analyze data from a previous randomized controlled trial (Feixas et al., 2016), which assessed the efficacy of a dilemma-focused intervention, a new variant of cognitive therapy for depression (Feixas & Compañ, 2016). All patients (N = 141) in that study met the criteria for either Major Depressive Disorder or Dysthymia (or both) as assessed with the structured clinical interview for DSM-IV axis I disorders (SCID-I-CV; First, Spitzer, Gibbon, & Williams, 1996). Also as an inclusion criterion, patients had to score more than 19 on the Beck's Depression Inventory-II (BDI-II; Beck, Steer, & Brown, 1996).The study protocol was approved by the Bioethics Committee of the University of Barcelona (Ref. IRB0003099). All the participants signed an informed consent document before enrolling.
From those, 31 (22%) had a concurrent diagnosis of FM at baseline. These patients were the target of the present study. Their mean age was 50.45 years (SD = 9.60), with an average of 2.06 depressive episodes (SD = 1.21). They reported a mean pain intensity of 76.21 (SD = 20.73) in the visual analogue scale (VAS; Price, McGrath, Rafii, & Buckingham, 1983), a 100-mm line for the assessment of pain intensity; and an average of 8.14 years (SD = 6.4) with FM diagnosis. The comparison group was a paired sample of 31 patients from the same trial who did not have the diagnosis of FM and who had not reported high levels of pain intensity (scored lower than 50 in VAS). Variables used for matching this control sample to the FM group were age (M = 50.85; SD = 9.47), sex (28 females and 3 males) and number of depressive episodes (M = 1.96; SD = 1.43). Both groups were also comparable in terms of time elapsed, in years, from the first episode (M = 12.48; SD = 11.46 for the target group and M = 10.45; SD = 9.78, for the control group).
InstrumentsThe repertory grid technique (Feixas & Cornejo, 2002), a semi-structured interview created to study personal constructs, was used for assessing cognitive structure. Constructs were elicited in each patient from comparisons among a set of elements (e.g., self, family relatives, friends, ideal self), followed by rating these elements for each construct with a 7-point Likert scale. This resulted in construct data matrix from which several measures were derived using specialized software (GRIDCOR v 4.0; Feixas & Cornejo, 2002). For the present study (see Feixas, Montesano, Erazo-Caicedo, Compañ, & Pucurull, 2014 for a wider variety of measures), the PVAFF resulting from a factor analysis of the grid data was used as an indicator of unidimensional thinking (Feixas, Bach, & Laso, 2004). The higher the percentage, the smaller the room for other dimensions of meaning to take prominence in construing self and others. The second grid measure used in this study was polarization, computed simply as the percentage of extreme ratings (1 or 7) in the grid data matrix. Most authors support the construct validity of the RGT as the notions employed (e.g., “personal construct”) are directly derived from the theory. Several studies have reported test-retest reliability scores of .71-.77 for the elements, and of .48-.69 for the elicited constructs (see Feixas & Cornejo, 1996; for a review). A recent study (Trujillo, 2016), in the same local context as the present one, yielded a test-retest reliability score of .84 for the PVAFF, and of .81 polarization measure.
Statistical analysisOne-tailed independent samples t-tests were performed using SPSS 23.0 (IBM Corp., 2015). Cohen's d effect sizes were calculated for each dependent variable.
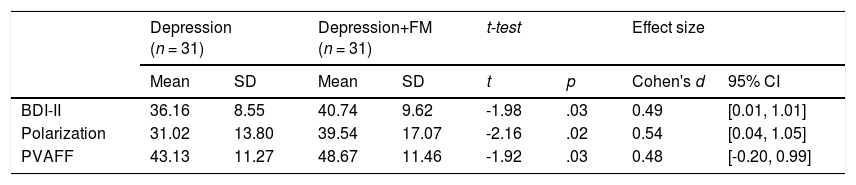
ResultsAs shown in Table 1, significant differences were found between both samples for depressive symptoms, polarization and PVAFF. Depressed patients with FM presented significantly higher BDI-II scores, higher polarization and higher PVAFF than those without FM. The two groups were different in their degree of symptom severity, polarization and cognitive differentiation with a medium effect size. No statistical differences were found in the number of constructs elicited in the grids of both samples.
Comparison of depressive patients with and without a concurrent diagnosis of fibromyalgia.
| Depression (n = 31) | Depression+FM (n = 31) | t-test | Effect size | |||||
|---|---|---|---|---|---|---|---|---|
| Mean | SD | Mean | SD | t | p | Cohen's d | 95% CI | |
| BDI-II | 36.16 | 8.55 | 40.74 | 9.62 | -1.98 | .03 | 0.49 | [0.01, 1.01] |
| Polarization | 31.02 | 13.80 | 39.54 | 17.07 | -2.16 | .02 | 0.54 | [0.04, 1.05] |
| PVAFF | 43.13 | 11.27 | 48.67 | 11.46 | -1.92 | .03 | 0.48 | [-0.20, 0.99] |
Note. FM = Fibromyalgia; BDI-II= Beck Depression Inventory-II; PVAFF= Percentage of Variance Accounted by the First Factor.
Our results, along with the review of Goesling, Clauw and Hasset (2013), indicated that at least for some patients, depression might be associated with the experience of pain. Twenty per cent of our sample had a concurrent diagnosis of FM. This result is convergent with that reported for patients with other chronic pain disorders (Ohayon & Schatzberg, 2003; Réthelyi, Berghammer, & Kopp, 2001). It is worthy to mention that this percentage rose to 60% if we took into account patients who experienced a high level of pain (over 50 in VAS). Interestingly, our results indicated that depressed patients with comorbid FM scored higher in depressive symptomatology. Further analyses of BDI-II showed higher scores in the FM comorbid group in the items concerning pessimism, irritability, concentration/difficulty, tiredness or fatigue and loss of interest in sex. The nature of the relationship between pain and depression needs further studies to develop a better understanding in the future.
Pain experience in depression seems to be associated also to cognitive structure. Polarized construing emerged as the most distinctive cognitive structure between the two groups. Although the tendency to construe themselves in extreme terms had been proposed as characteristic of individuals with depression (Neimeyer, 1985), depressed patients with comorbid FM showed higher scores in polarization with a medium effect size. Moreover, PVAFF showed a similar pattern indicating that depressed comorbid FM patients presented lower levels of differentiation in their dimensions of meaning. These results converged with those reported by Neimeyer and Feixas (1992), in which structural cognitive measures such as cognitive differentiation and polarization accounted for a specific factor of rigidity in depressive patients.
The small size of the study is a limitation for the external validity of the study. But, in spite of the fact that our study focused on a few aspects and also that larger samples may be needed, our findings if confirmed in other studies might have relevant implications for clinical treatment of depressed patients with comorbid FM. For patients with chronic pain, increasing their cognitive complexity might lead to better therapeutic results. In that sense, attunement to the patients’ views of themselves and of the world can be a relevant factor to help promoting an evolution of these patients’ meaning systems (in terms of cognitive flexibility) to increase their capacity to deal with current and future events and problems.
Overall, our study points to the need for more attention to the role of chronic pain in the study and treatment of depressed patients. Maybe models of depression should differentiate between depressed patients with a chronic pain condition, such as FM, and those without pain. In addition, treatment strategies and efficacy studies should follow that line as well.
FundingThis work was funded by Ministerio de Ciencia e Innovación [PSI2011-23246].