Liver cysts comprise a mixed group of diseases with different aetiologies and incidences but similar clinical signs.
We report four cases of symptomatic giant liver cysts treated by means of laparoscopic deroofing with excellent outcomes.
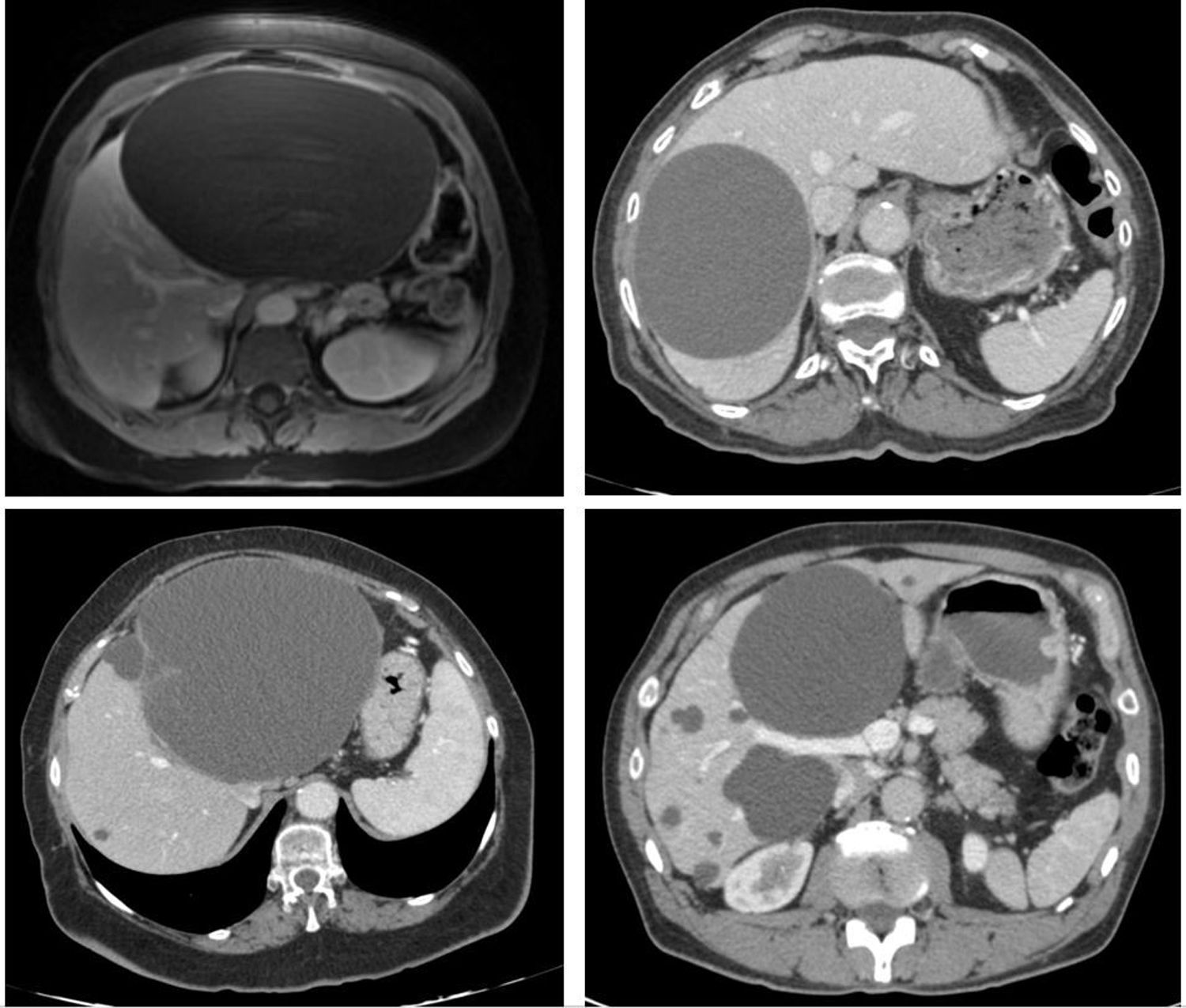
Case 1. A 53-year-old woman visited the emergency department for pain in her right hypochondrium for a week, initially thought to be nephritic colitis. Ultrasound and magnetic resonance imaging showed a simple cyst measuring 20 cm in liver segment 6. The cyst was hypointense in T1 and showed no wall enhancement following contrast administration.
Case 2. A 77-year-old man sought treatment for bilious vomiting and pain in his right hypochondrium for some months. An abdominal CT scan showed a cyst measuring 14 cm between liver segments 7 and 8, which, given the density of its contents, raised a differential diagnosis between a simple cyst, cystadenoma and/or biloma. A decision was made to perform exploratory laparoscopy. After the contents of the cyst were aspirated and it was confirmed that they were not of a biliary nature, deroofing was done.
Case 3. A 75-year-old man visited the emergency department due to a feeling of a mass in the epigastrium. An abdominal CT scan revealed a cyst measuring 18 cm that appeared to depend on the left liver lobe, occupying its entirety, with septations in its upper portion that raised suspicion that it might be a hydatid cyst. Serology tests ruled out this possibility and during the intervention it was observed that the cyst contained transformed blood.
Case 4. A 68-year-old man with a diagnosis of asymptomatic polycystic liver disease in follow-up for the past 5 years sought treatment for abdominal pain. A CT scan showed multiple cysts, the largest of which measured 12 cm and was causing displacement of the left portal branch (Fig. 1).
Case 1. Abdominal MRI: liver cyst measuring 20 cm in liver segment 6. It shows no wall enhancement following contrast administration (upper left). Case 2. Abdominal CT: cyst measuring 14 cm between liver segments 7 and 8 (upper right). Case 3. Abdominal CT: cyst measuring 18 cm. The upper portion features septations that raise suspicion of a hydatid cyst (lower left). Case 4. Abdominal CT: multiple liver cysts. The largest has a diameter of 12 cm (lower right).
The mean postoperative stay was 3 days. None of the patients experienced complications, and after a 5-year follow-up period none of them showed any recurrence of symptoms.
Both solitary and polycystic lesions grow slowly and are relatively asymptomatic. When they exceed 5 cm, they can cause symptoms due to compression of the hepatic veins, vena cava or bile ducts, or they can cause acute abdominal pain in the event of complications such as rupture, torsion or intracystic haemorrhage.1
Imaging tests (CT and/or magnetic resonance imaging) must be done to confirm a diagnosis of a simple cyst. Cystadenoma and cystadenocarcinoma should be ruled out, since laparoscopic fenestration would not be indicated. CT may aid in showing thick and irregular walls, septa, papillary inclusions and loculations. In endemic areas for hydatid disease, such as in our area, hydatid disease should be ruled out by means of serology (90–95% sensitivity), ultrasound and CT (95% specificity).2
Simple liver cysts generally require neither treatment nor follow-up, unless they are giant (10−20 cm) and cause symptoms and/or complications. Various techniques have been reported for the treatment of such cysts, depending on their number, location, relationship to other structures and contents: aspiration with or without injection of sclerosing agents3, argon plasma coagulation in the cyst cavity wall (contraindicated if it is in contact with the biliary tract)4, deroofing and connection with the peritoneal cavity, cystojejunostomy, complete cyst excision, partial hepatectomy, liver lobectomy (in cases of suspected cyst malignancy) and even liver transplantation (in cases of liver dysfunction due to advanced polycystosis).
At present, laparoscopic deroofing is the technique of choice, as reported by a recent systematic review of 62 studies with 1314 patients5, with a relapse rate similar to open surgery (25%), but with all the advantages a laparoscopic approach offers.
Laparoscopic deroofing is the technique of choice in symptomatic and/or complicated simple giant liver cysts.
Please cite this article as: Allue M, Palacios P, Jimenez A. Cuándo y cómo tratar los quistes hepáticos gigantes sintomáticos. Gastroenterol Hepatol. 2021;44:226–228.