Retrorectal cystic hamartoma also known as tailgut cyst is an uncommon congenital disease located in the presacral region-retrorectal space. It has been described in numerous anatomical locations, namely perianal, perirenal and subcutaneous involvement. Its rarity and location make it difficult to diagnose, often leading to misdiagnosis. Although it may affect individuals of all ages, this lesion occurs more frequently in middle-aged women with a 5:1 ratio.1 It is accepted to origin from an alteration of the development of the distal end of the embryonic intestine, or tailgut. This structure reaches its largest diameter on the 35th day of gestation, and regresses by the eighth week of embryonic development. The ectoderm makes an invagination and fuses with the primitive gut to form the anus a few centimetres above its distal end, giving rise to postanal embryonic intestinal remnants with a linear tubular structure composed of 2–4 lines of cuboidal epithelium.
Due to its location, the tailgut cyst can generally be palpated by rectal examination. Whenever suspected, magnetic resonance imaging (MRI) is the most accurate non-invasive imaging technique for its diagnosis, showing a homogeneous hypodensity on T1 images and high-signal intensity on T2 images, caused by its mucinous content.2 The differential diagnosis includes a wide spectrum of congenital, neoplastic, and inflammatory disorders which may be present in the presacral region. These different entities include cystic sacrococcygeal teratoma, anal gland cyst, pyogenic abscess, neurogenic cyst, and necrotic sacral chordoma.2
Although it is a benign developmental alteration, some reported cases have degenerated into a malignant adenocarcinoma originated on the epithelial layer of the tailgut cyst.3 Song et al. reported six cases that developed neuroendocrine neoplasms.4 The risk of malignant transformation has been reported to be about 13%, thus, complete resection of the cyst is always recommended.5 The risk of malignant transformation cannot be determined by any clinical, imaging or pathological characteristics. To our knowledge, there is no recognized association of the retrocecal cyst hamartoma to any other type of syndromes or malformations.
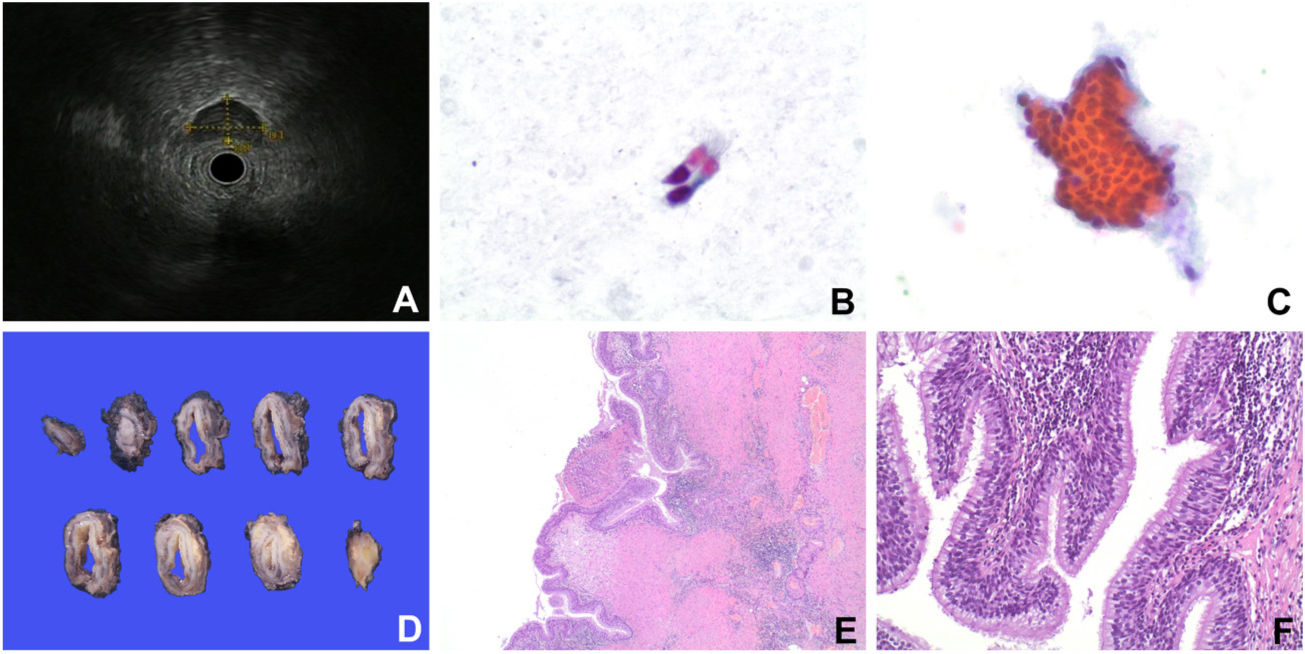
We present a case of a 26-year-old male with no relevant past medical history, who presented with sacral pain unresponsive to pharmacological therapy. An MRI study performed three years earlier in another centre showed a paracentral posterior L4–5 disc herniation. As an incidental finding, an oval retrorectal lesion measuring 31×22mm was observed, which was in the presacral space anterior to the left piriformis muscle. The lesion had well-defined contours and thin walls, showing hyperintensity on T1 and T2. A second MRI was performed at our institution, showed that it had diminished its size to 25×20mm. Its intensity suggested a cystic lesion with haemorrhagic or proteinaceous content. An endoscopic ultrasound fine-needle aspiration (EUS-FNA) was performed, observing a very hypoechoic lesion located in the presacral region, at 14cm from the anal verge. The lesion had well-defined regular borders, not depending on the rectal wall, which had a normal thickness and preserved the layered echostructure (Fig. 1A). No pathologic lymph nodes were identified in the perirectal fat. A FNA was performed using a 22G needle, obtaining purulent material for cytological diagnosis. The patient had fever and pain after the procedure, which resolved with systemic antibiotics. Cytologic analysis revealed the presence of few isolated cylindrical ciliated epithelial cells without atypia, in a background of amorphous-proteinaceous material and occasional groups of transitional-like epithelial cells (Fig. 1B, C). Cytological diagnosis was compatible with a hamartoma-tailgut cyst. Surgical resection was considered due to patient's symptoms, with a monoblock lateral dissection of the mesorectum including the presacral fascia. The post-operative course was uneventful. A fresh intact nodular lesion measuring 30×18×8mm was received at the Pathology Department, and the entire surface was painted with black Indian ink. Gross sectioning revealed a cystic lesion with a 2mm thick wall with yellowish areas of medium consistency, lined by a thin and smooth surface containing a brownish fluid (Fig. 1D). Histologic examination revealed a cystic lesion lined by non-dysplastic ciliated columnar pseudostratified epithelium containing mucinous cells and few lymphocytes. In some areas the epithelium showed a transitional appearance (Fig. 1E and F). The rest of the wall was composed by smooth muscle with ectasic vessels, and areas of chronic lymphohistiocytic and xanthomatous inflammation, corresponding to the FNA trajectory. The final pathological diagnosis was of retrorectal hamartoma (tailgut cyst) lined by ciliated-cylindric epithelium with mucin production and no displasia.
A: Endoscopic Ultrasound shows a hypoechoic lesion with had well-defined regular borders and is not dependent on the rectal wall. B: Cytologic findings: Ciliated cylindrical epithelial cells without atypia. C: Occasional groups of transitional-like epithelial cells. D: Gross findings: sections of the cyst showed a 2mm thick wall with a delicate muscular layer, whitish fibrous tissue, and yellowish areas of medium consistency. E: Microscopic findings: some areas the epithelium showed a transitional appearance (H&E ×10). F: Higher power view showing a cystic lesion lined by non-dysplastic ciliated columnar pseudostratified glandular epithelium with mucinous cells (H&E ×20).
We are acknowledge to the Department of Pathology from the Biomedical Diagnostic Center (CDB) of Hospital Clinic for technical support.