In the midst of the SARS-CoV2 virus (COVID-19) pandemic, health professionals, specifically gastroenterologists, have had to use personal protective equipment (PPE) to reduce contact with droplets and aerosols generated during gastrointestinal endoscopy.
ObjectiveTo evaluate the impact of the use of two types of PPE on quality of vision during gastrointestinal endoscopy.
MethodsA cross-sectional observational pilot study in gastroenterologists who undergo an ophthalmological examination of visual acuity and quality of vision when using two types of PPE. Type #1: 3M N95 1860 green respirator + 3M mono safety glasses + protective screen. Type #2: 3M 6800 full facepiece + 3M NIOSH 7093C HF/P100 filters.
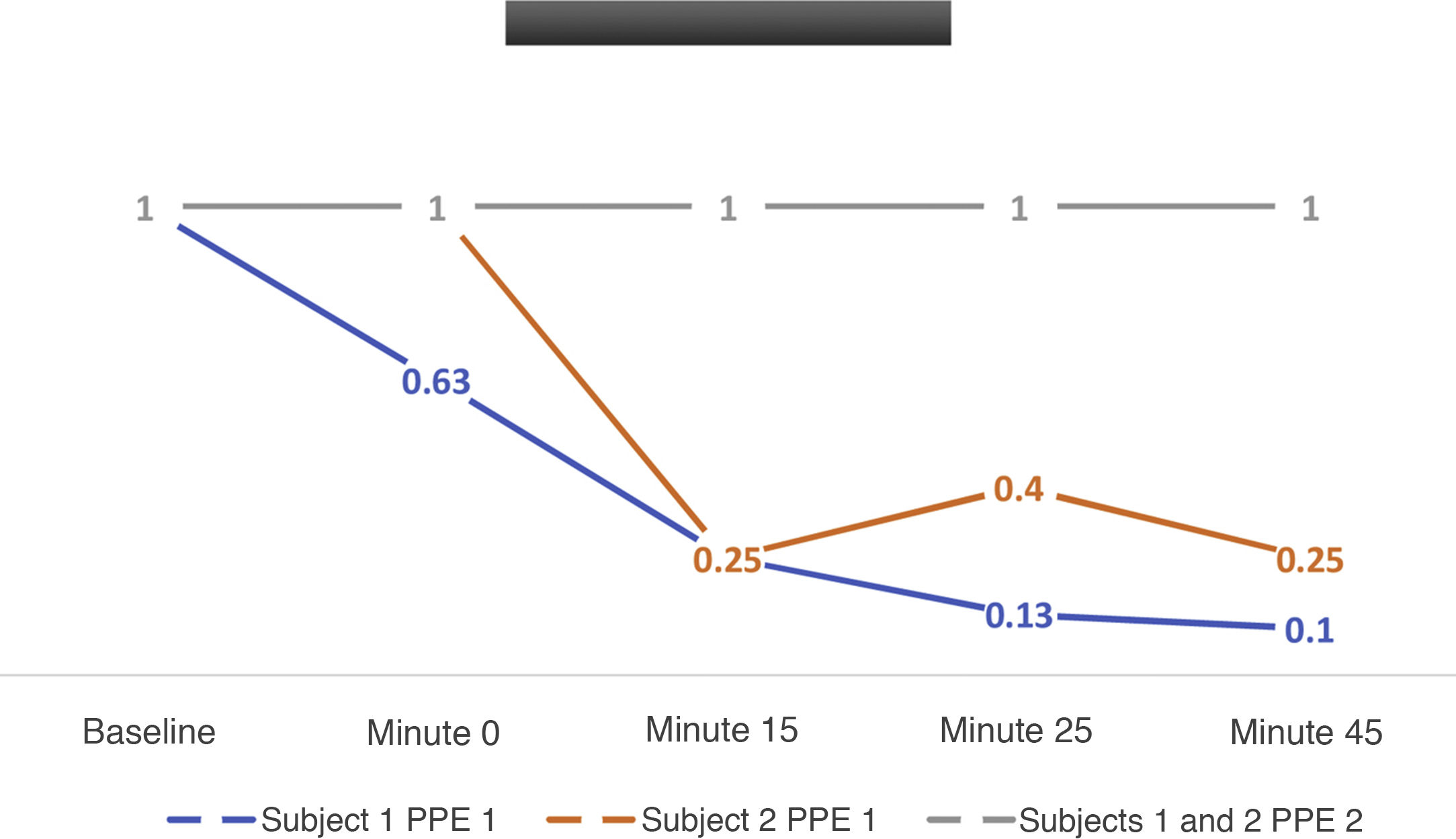
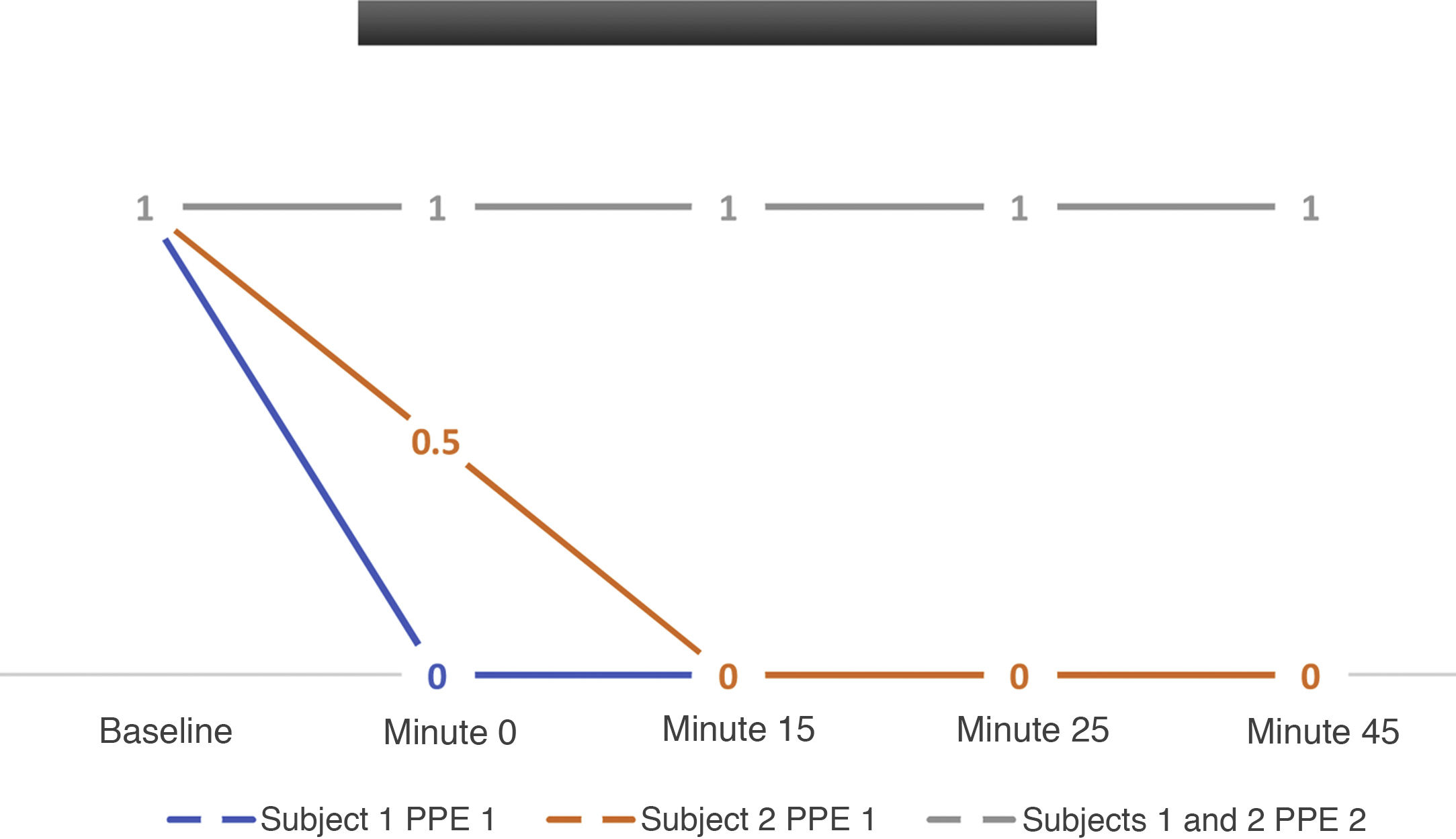
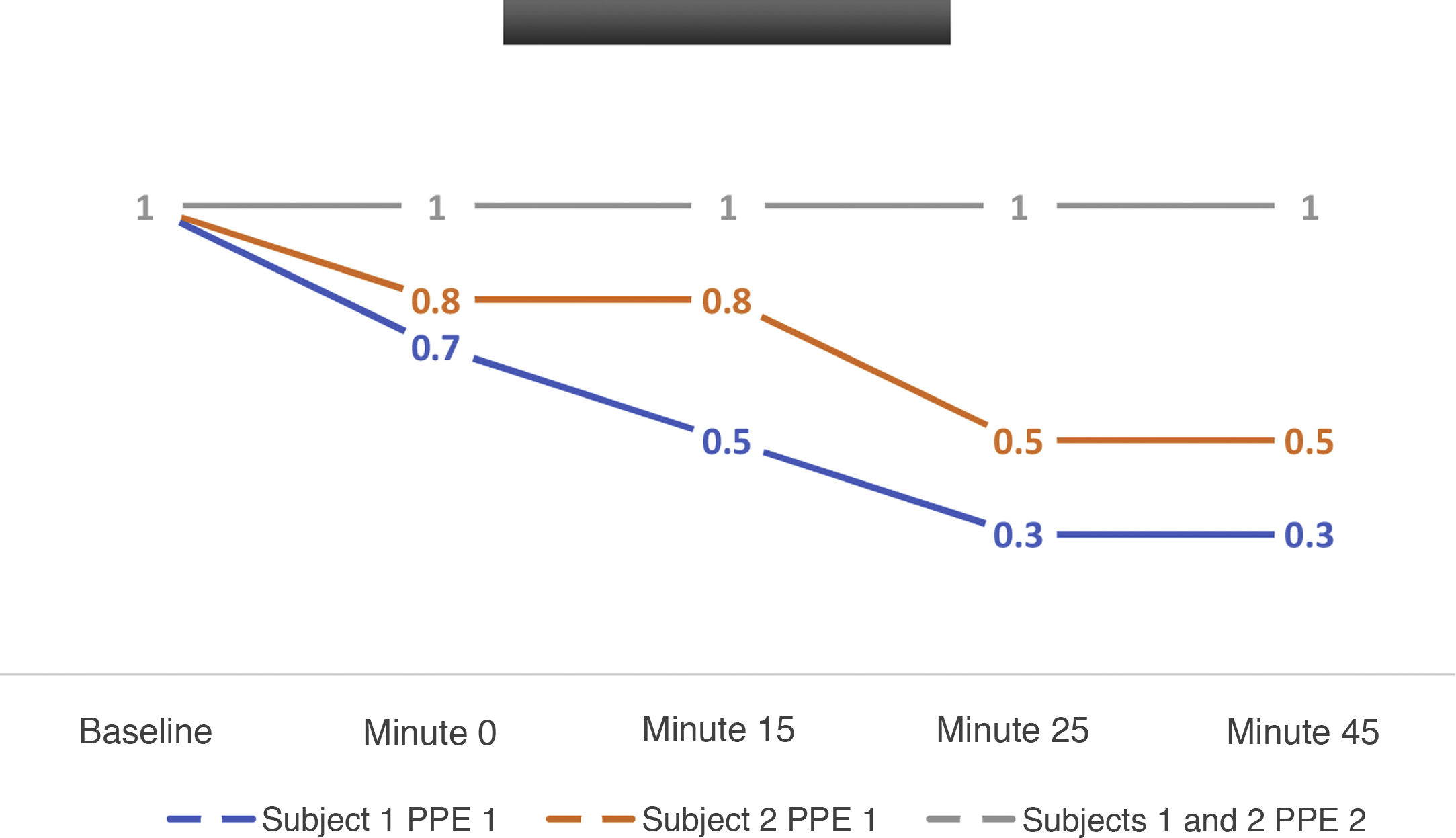
ResultsVisual acuity and quality of vison parameters while using the PPE that is routinely used when performing gastrointestinal endoscopy during the pandemic were evaluated. It was found that Modality #1 was associated with decreases of up to 37% in visual acuity, 25% in colour visualisation and 75% in contrast sensitivity among digestive endoscopists within minutes of placement. These figures worsened over the course of the procedure, rising to 75%, 60% and 100%, respectively. Modality #2 was not associated with any deterioration in quality of vision.
ConclusionsThe different PPE modalities used during gastrointestinal endoscopy could have an impact on the quality of endoscopy studies performed during the SARS COV2 (COVID-19) pandemic.
En tiempos de la pandemia por el virus SARS-CoV2 (Covid-19), los profesionales de la salud y específicamente los gastroenterólogos hemos tenido la necesidad de usar elementos de protección personal (EPP) para disminuir el contacto con microgotas y aerosoles durante la realización de endoscopia digestiva.
ObjetivoEvaluar el impacto del uso de dos modalidades de elementos de protección personal en la calidad de la visión durante la endoscopia digestiva.
MétodosEstudio piloto observacional de corte transversal en gastroenterólogos a quienes se les realiza examen oftalmológico de agudeza y calidad visual al utilizar dos modalidades de EPP Modalidad#1: Respirador N95 3M 1860 VERDE + Monogafas 3M + Pantalla protectora y modalidad #2: Pieza Facial de cara completa 3M 6800 con filtros 3M 7093C NIOSH HF/P100.
ResultadosAl evaluar los parámetros de agudeza y calidad visual al usar los EPP que se utilizan rutinariamente en el ejercicio de la endoscopia digestiva durante la pandemia, se identifica que con el uso de la modalidad #1, una disminución de hasta el 37% en la agudeza y en 25% en la visualización del color y el 75% en la sensibilidad al contraste en endoscopistas digestivos desde los primeros minutos de la colocación, lo cual empeora en el tiempo, hasta 75, 60 y 100% respectivamente durante el procedimiento. En el caso de la modalidad #2, no hay deterioro de la calidad de la visión.
ConclusionesLas diferentes modalidades de EPP utilizados durante la endoscopia digestiva podrían tener repercusión en la calidad de los estudios endoscópicos realizados durante la pandemia por SARS COV2 (Covid-19).
Since the advent of the SARS-CoV-2 (COVID-19) pandemic in December 2019, the entire population, particularly health personnel, has been forced to use personal protective equipment (PPE) to reduce the probability of contact and therefore of contagion of the disease caused by this agent, whose virulence is high compared to other recent epidemics in the world.1
Specifically in digestive endoscopy, the production of droplets and the protection of the personnel directly involved in the procedures has acquired great relevance, leading to the discussion of the subject in numerous forums, both in gastroenterology and endoscopy associations and in health institutions’ infectious disease committees. The recommendation made by most of the documents produced by such meetings and consensus is the use of respirators with N95 or higher filters (FFP2 and FFP3) and eye protection, by means of mono glasses and/or protective shields to reduce exposure of the conjunctiva or the mucosa to the virus. There are also fullface pieces with N95 filters and simultaneous face and eye protection on the market which have become an alternative for some specialist physicians.2,3
All endoscopists are well acquainted with the discomfort, the limitation upon free air flow during breathing and the effects of these devices on facial skin. However, another relevant aspect is the reduction in visual acuity and quality produced by misting in some of the adjustable mono glasses or the additional glare that could limit the effectiveness of the procedure at any moment, either due to the reduced capacity to detect and classify small lesions, or because certain therapeutic procedures, the efficacy and safety of which in many cases hinge on precision, are hampered or delayed.4,5
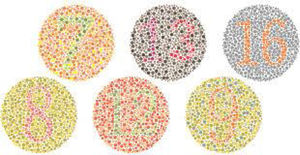
For this reason, a quantification and comparison of visual parameters such as visual acuity (VA) is proposed, where VA is defined as the human visual system's capacity to make out, recognise or distinguish details in objects under conditions of high contrast and with a good level of illumination,6 in the Snellen fraction, contrast sensitivity (CS), which represents the lowest contrast the visual system can detect7 and the Ishihara colour vision test (CV), a test that uses random-sized and coloured dot circles to identify colour vision defects, in endoscopist specialists with different PPE modalities, for the purpose of evaluating the impact of the use of two modalities of personal protective equipment on vision quality during digestive endoscopy.
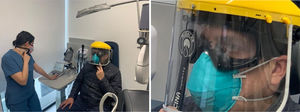
MethodsAn observational cross-sectional pilot study was carried out, in which gastroenterology professors with more than 10 years of experience in digestive endoscopy were examined, one of them with refractive error correction using glasses with conventional lenses and the other with a background of laser-assisted refractive surgery without the need for optical correction.
Each subject used both of the following PPE modalities: modality #1: N95 3M 1860 green respirator + 3M mono glasses + protective shield and modality #2: 3M 6800 full facepiece with NIOSH 3M 7093C HF/P100 filters.
The ophthalmological examination was performed by an ophthalmologist, a university professor with an NIDEK SC 1600 optotype screen (Fig. 1): with this, visual acuity (VA measured in Snellen fraction at 20 feet) (Fig. 2), contrast sensitivity (CS) test (with the optotype represented at 25%, 12.5% or 6% contrast, the best possible contrast vision being 6%) and the Ishihara colour vision (CV) test (10 images from the Ishihara test) are taken (Fig. 3). Before the subjects don the PPE, the best-corrected VA measurement is taken for each one of them, who then don the PPE, and a better-corrected VA, contrast sensitivity and colour vision test is performed when they put it on and after 15, 25 and 45 minutes (Figs. 4 and 5).
Subsequently, after a 30-minute rest, the subjects switch to the other PPE modality to perform the visual ophthalmological examination again at the same time intervals.
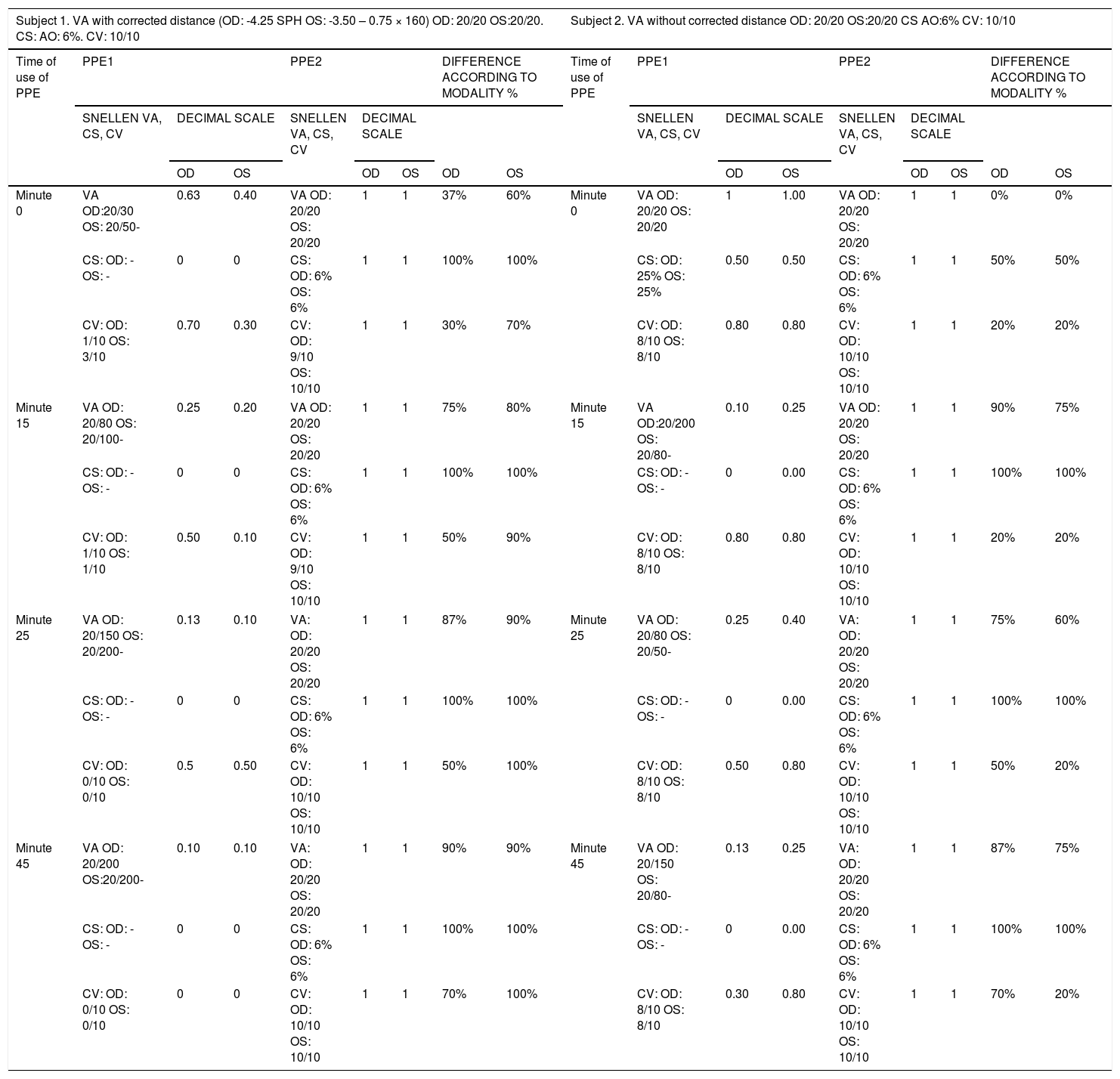
ResultsAfter the ophthalmological assessment of the visual examination of the subjects with the NIDEK SC 1600 optotype screen for visual acuity (VA measured in Snellen fraction at 20 feet), contrast sensitivity (CS) test and Ishihara colour vision (CV) test (10 images from the Ishihara test), with an independent evaluation of both eyes of each previous subject, minute 0, 15, 25 and 45 (Table 1).
Data from the assessment of visual acuity, contrast and colour visualisation with the use of two modalities of personal protective equipment.
| Subject 1. VA with corrected distance (OD: -4.25 SPH OS: -3.50 – 0.75 × 160) OD: 20/20 OS:20/20. CS: AO: 6%. CV: 10/10 | Subject 2. VA without corrected distance OD: 20/20 OS:20/20 CS AO:6% CV: 10/10 | ||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Time of use of PPE | PPE1 | PPE2 | DIFFERENCE ACCORDING TO MODALITY % | Time of use of PPE | PPE1 | PPE2 | DIFFERENCE ACCORDING TO MODALITY % | ||||||||||
| SNELLEN VA, CS, CV | DECIMAL SCALE | SNELLEN VA, CS, CV | DECIMAL SCALE | SNELLEN VA, CS, CV | DECIMAL SCALE | SNELLEN VA, CS, CV | DECIMAL SCALE | ||||||||||
| OD | OS | OD | OS | OD | OS | OD | OS | OD | OS | OD | OS | ||||||
| Minute 0 | VA OD:20/30 OS: 20/50- | 0.63 | 0.40 | VA OD: 20/20 OS: 20/20 | 1 | 1 | 37% | 60% | Minute 0 | VA OD: 20/20 OS: 20/20 | 1 | 1.00 | VA OD: 20/20 OS: 20/20 | 1 | 1 | 0% | 0% |
| CS: OD: -OS: - | 0 | 0 | CS: OD: 6% OS: 6% | 1 | 1 | 100% | 100% | CS: OD: 25% OS: 25% | 0.50 | 0.50 | CS: OD: 6% OS: 6% | 1 | 1 | 50% | 50% | ||
| CV: OD: 1/10 OS: 3/10 | 0.70 | 0.30 | CV: OD: 9/10 OS: 10/10 | 1 | 1 | 30% | 70% | CV: OD: 8/10 OS: 8/10 | 0.80 | 0.80 | CV: OD: 10/10 OS: 10/10 | 1 | 1 | 20% | 20% | ||
| Minute 15 | VA OD: 20/80 OS: 20/100- | 0.25 | 0.20 | VA OD: 20/20 OS: 20/20 | 1 | 1 | 75% | 80% | Minute 15 | VA OD:20/200 OS: 20/80- | 0.10 | 0.25 | VA OD: 20/20 OS: 20/20 | 1 | 1 | 90% | 75% |
| CS: OD: -OS: - | 0 | 0 | CS: OD: 6% OS: 6% | 1 | 1 | 100% | 100% | CS: OD: -OS: - | 0 | 0.00 | CS: OD: 6% OS: 6% | 1 | 1 | 100% | 100% | ||
| CV: OD: 1/10 OS: 1/10 | 0.50 | 0.10 | CV: OD: 9/10 OS: 10/10 | 1 | 1 | 50% | 90% | CV: OD: 8/10 OS: 8/10 | 0.80 | 0.80 | CV: OD: 10/10 OS: 10/10 | 1 | 1 | 20% | 20% | ||
| Minute 25 | VA OD: 20/150 OS: 20/200- | 0.13 | 0.10 | VA: OD: 20/20 OS: 20/20 | 1 | 1 | 87% | 90% | Minute 25 | VA OD: 20/80 OS: 20/50- | 0.25 | 0.40 | VA: OD: 20/20 OS: 20/20 | 1 | 1 | 75% | 60% |
| CS: OD: -OS: - | 0 | 0 | CS: OD: 6% OS: 6% | 1 | 1 | 100% | 100% | CS: OD: -OS: - | 0 | 0.00 | CS: OD: 6% OS: 6% | 1 | 1 | 100% | 100% | ||
| CV: OD: 0/10 OS: 0/10 | 0.5 | 0.50 | CV: OD: 10/10 OS: 10/10 | 1 | 1 | 50% | 100% | CV: OD: 8/10 OS: 8/10 | 0.50 | 0.80 | CV: OD: 10/10 OS: 10/10 | 1 | 1 | 50% | 20% | ||
| Minute 45 | VA OD: 20/200 OS:20/200- | 0.10 | 0.10 | VA: OD: 20/20 OS: 20/20 | 1 | 1 | 90% | 90% | Minute 45 | VA OD: 20/150 OS: 20/80- | 0.13 | 0.25 | VA: OD: 20/20 OS: 20/20 | 1 | 1 | 87% | 75% |
| CS: OD: -OS: - | 0 | 0 | CS: OD: 6% OS: 6% | 1 | 1 | 100% | 100% | CS: OD: -OS: - | 0 | 0.00 | CS: OD: 6% OS: 6% | 1 | 1 | 100% | 100% | ||
| CV: OD: 0/10 OS: 0/10 | 0 | 0 | CV: OD: 10/10 OS: 10/10 | 1 | 1 | 70% | 100% | CV: OD: 8/10 OS: 8/10 | 0.30 | 0.80 | CV: OD: 10/10 OS: 10/10 | 1 | 1 | 70% | 20% | ||
VA: visual acuity; CS: contrast sensitivity; CV: colour vision; OD: right eye; OS: left eye.
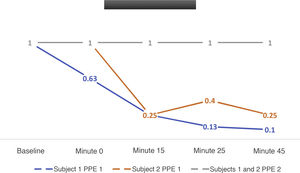
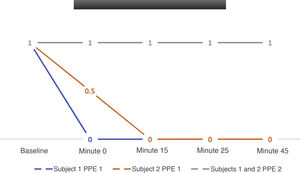
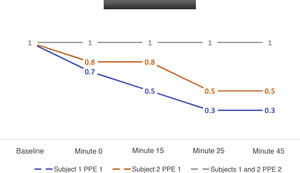
There is a significant decrease that worsens over time in the three parameters with the use of the first PPE modality (N95 3M 1860 green respirator + 3M mono glasses + protective shield), with a 37% reduction in visual acuity when the equipment is donned and of up to 75% after 45 minutes of use (Fig. 6), contrast sensitivity compromise is greater than 75% initially and is 100% after 45 minutes (Fig. 7), whereas in colour vision it is 25% at the beginning and up to 60% after 45 minutes (Fig. 8).
With the use of the second PPE modality (3M 6800 full facepiece with NIOSH 3M 7093C HF/P100 filters). There is no variation in any of the aforementioned parameters and visual quality remains equal to the baseline.
DiscussionThis is the first study to evaluate the impact of different PPE modalities on visualisation quality in medical procedures during the SARS-CoV-2 (COVID-19) pandemic and which impact the assessment of optical parameters and probably the quality of endoscopic studies (defined as an increased rate of complications and a reduction in diagnostic performance for lesions with subtle changes in the mucosal pattern, whether they are preneoplastic or early neoplastic). This alteration is due to significant limitations in visual acuity, contrast sensitivity and colour visualisation. These parameters are affected in this study between the moment the PPE are donned and worsen over time depending on the duration of the procedure.
Full facepiece PPE do not alter the optical parameters evaluated in the first measurement or as the procedure evolves and are equal to the optical measurements obtained without the use of PPE, which is considered the best vision possible for each subject.
Studies with a greater number of measurements that could confirm or refute the findings of this pilot study are required, as are prospective studies that would make it possible to determine whether the visual alterations documented during this pandemic have an impact on strong endoscopic quality outcomes.
One additional, but no less important, point, will be the evaluation of the impact on ergonomics and health at work PPE entailed in the use of this PPE.
ConclusionSome PPE modalities used during gastrointestinal endoscopy reduce endoscopists’ quality of vision, which could affect the quality and even the frequency of complications of diagnostic and therapeutic procedures performed during the SARS-CoV-2 (COVID-19) pandemic.
FundingNo funding was received for this study.
Conflicts of interestThe authors declare that they have no conflicts of interest.
Please cite this article as: Rincón Sánchez RA, Concha Mejía A, Viaña Ríos LM. Calidad de la visión en endoscopia en tiempos de pandemia: ¿Influyen los EPP en la calidad visual durante la endoscopia digestiva? Gastroenterología y Hepatología. 2021;44:637–643.