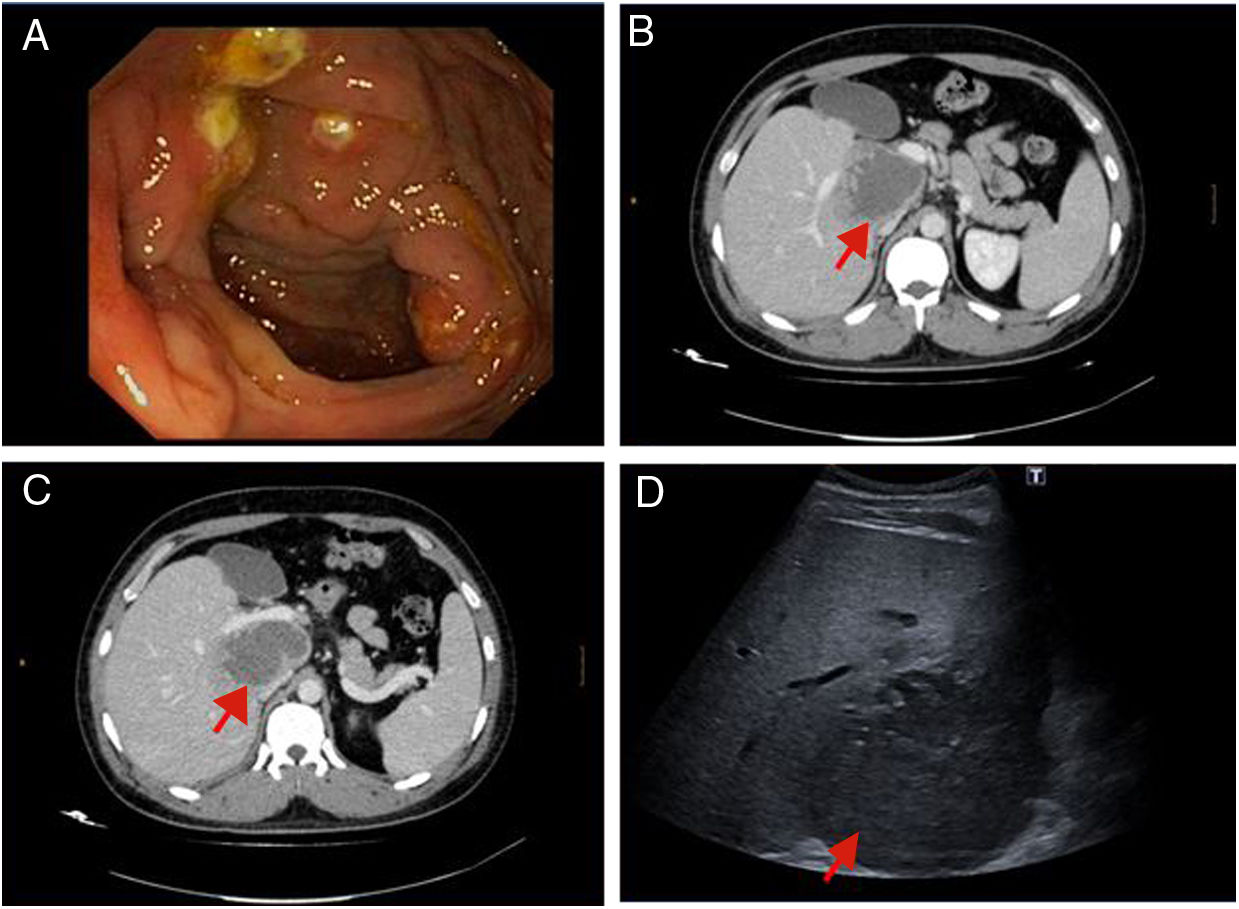
We present the case of a 29-year-old male from Romania who attended the Emergency Department having experienced diarrhoea with rectorrhagia and general malaise for several weeks. Following symptoms of diarrhoea and rectorrhagia, he had been diagnosed five months prior with Crohn's disease (CD) following a colonoscopy that showed several round, fibrinous ulcers on erythematous mucosa measuring 5–7 mm in the ascending colon (Fig. 1A). The biopsies were reported as "possible CD, to be correlated with the symptoms".
An abdominal ultrasound was performed in the Emergency Department, which revealed signs of inflammation in the wall of the ascending colon. Suspecting a CD flare-up, treatment was started with intravenous steroids at a dose of 1 mg/kg per day.
Whilst in hospital, the patient's condition began to worsen. An abdominal computed tomography (CT) scan was performed that revealed a liver abscess up to 90 mm in diameter (Fig. 1B and C), for which empirical antibiotic therapy was started (imipenem and amikacin).
On reviewing the patient's medical history and complementary tests, the morphology of the colic ulcers was found not to be typical of CD. The biopsy was also inconclusive and the patient's wife was originally from Nicaragua, which he frequently visited. In light of the above, amebiasis was included in the differential diagnosis and ultrasound-guided percutaneous drainage of the abscess was performed (there was a risk of rupture and dissemination given its size) (Fig. 1D). Another parasitic study was requested and intravenous metronidazole was added at a dose of 750 mg/8 h. Stool samples were reviewed and either Entamoeba histolytica or Entamoeba dispar was identified.
The drained abscess fluid had a typical chocolate-coloured appearance, although no germ was isolated. After drainage and treatment with metronidazole, the patient gradually improved. As a result, the drain was removed 14 days later and he was discharged on oral paromomycin to eradicate the luminal amoebae.
In this case, the misdiagnosis of CD led to treatment with high-dose corticosteroids, which probably exacerbated the liver abscess. A CD diagnosis is based on clinical, laboratory, endoscopic, radiological and pathological criteria, as well as the exclusion of other conditions that can mimic similar lesions. A single suggestive finding should not lead to a definitive diagnosis without the appropriate context and differential diagnosis.1 In this case, the consequences of an incorrect diagnosis were significant.
Amebiasis is one of the diseases that should be included in the differential diagnosis of possible CD2 and correct diagnosis is crucial given that treatment with corticosteroids is one of the trigger factors of extraintestinal invasion. In our patient, the liver abscess, together with clinical suspicion and proper history taking, including "risk" contacts, were key.
Intestinal amebiasis is a parasitic disease caused by the protozoan Entamoeba histolytica. Although in most cases it is asymptomatic, in some patients it may cause bowel disease or even extraintestinal invasion. Whilst its incidence in Spain is low, it is increasing due to influxes of migrants from countries where the disease is more prevalent.3
Approximately 90% of patients remain asymptomatic. The main risk factors for developing this disease are being extremely young or old, malnutrition, treatment with steroids and immunosuppression.
Amoebic colitis is normally subacute, with diarrhoea, abdominal pain and rectorrhagia. Given these symptoms, a differential diagnosis should be performed with other infections like Shigella, Salmonella, Campylobacter or Escherichia coli, as well as other conditions such as inflammatory bowel disease, acute diverticulosis or ischaemic colitis.4
The most common extraintestinal manifestation is a liver abscess, which is normally associated with fever and pain in the right hypochondrium. There tends to be just one abscess in the right lobe and it is diagnosed with imaging tests: CT scan, MRI or ultrasound. The primary cause of liver-abscess-related mortality is its rupture into the pericardium or peritoneum. Treatment consists of intravenous antibiotic therapy (metronidazole) and drainage when required, particularly for larger abscesses of around 10 cm or abscesses in the left lobe.5
Please cite this article as: Casas Deza D, Llorente Barrio M, Monzón Baez RM, Lamuela Calvo LJ, Gascón Ruiz M, Ramos Lisbona AI, et al. No siempre es una enfermedad de Crohn: amebiasis como diagnóstico diferencial de la enfermedad inflamatoria intestinal. Gastroenterol Hepatol. 2019;42:548–549.