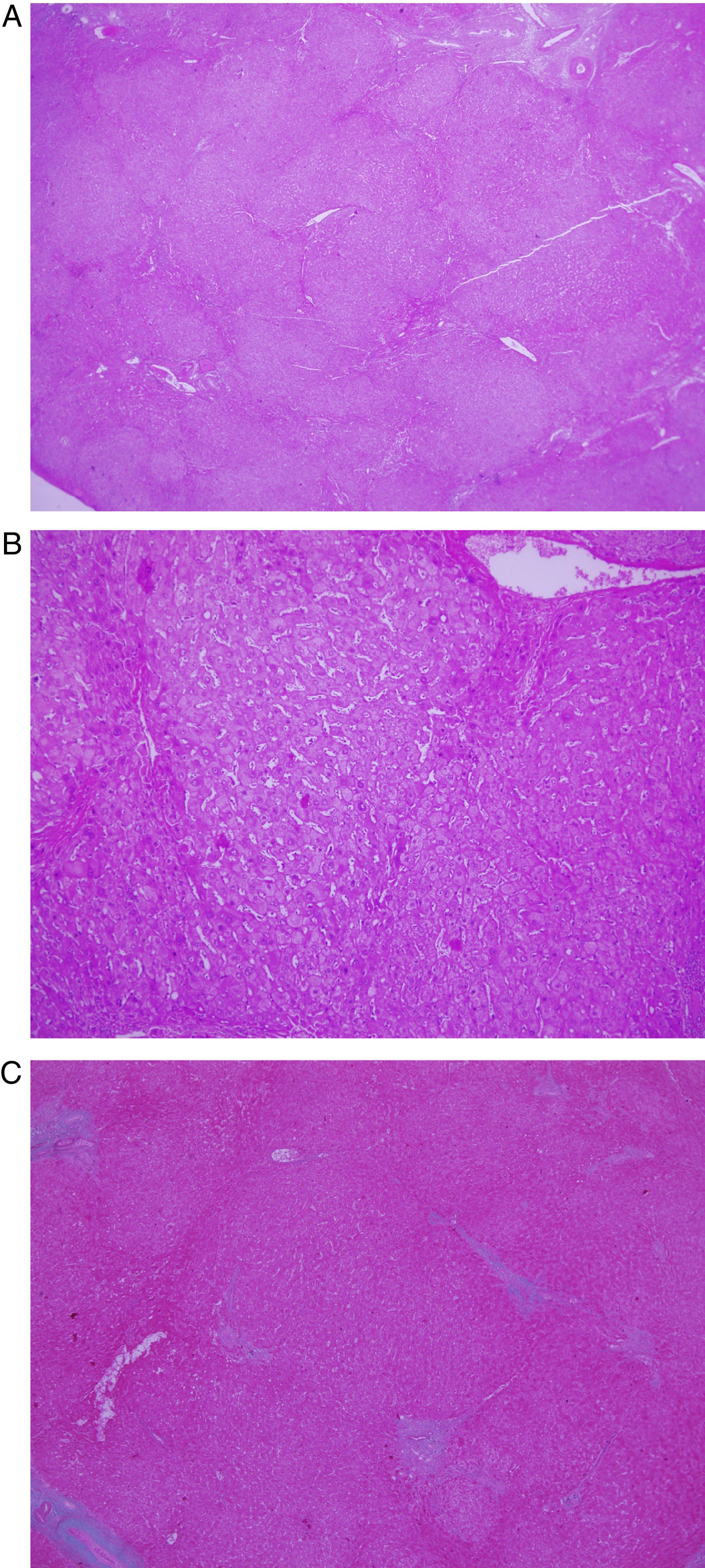
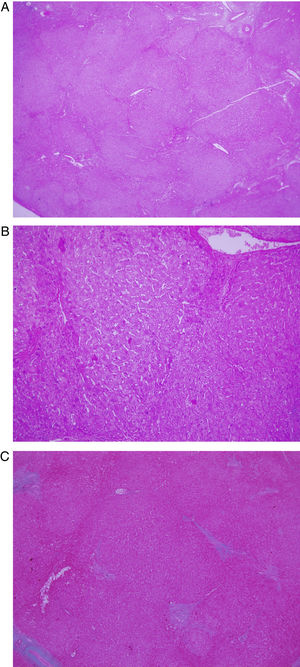
A 57-year-old male with a history of thrombocytopenia of autoimmune origin and seropositive rheumatoid arthritis diagnosed in 2001 was being treated with rituximab, non-steroidal anti-inflammatory drugs (NSAIDs) and Dacortin® [prednisone] 5mg daily. He was admitted due to an episode of upper gastrointestinal bleeding consisting of melenic stools. Gastroscopy revealed medium-sized oesophageal varices, which underwent band ligation. Laboratory testing revealed: gamma-glutamyl transpeptidase (GGT) 117U/l, alkaline phosphatase (AP) 119U/l, haemoglobin (Hb) 10g/dl and platelets 77,000/mm3. An abdominal ultrasound showed a liver with a slightly heterogeneous ultrasound structure, with regular borders, repermeabilisation of the umbilical vein, a dilated portal vein and splenomegaly with a permeable splenoportal axis. These findings were corroborated by a computed tomography (CT) scan. The patient denied having consumed alcohol or other toxic substances. Serology was ordered for hepatotropic viruses and hepatic autoimmunity (antinuclear antibodies [ANAs], antimitochondrial antibodies [AMAs], anti-smooth muscle antibodies [ASMAs], liver kidney microsome type 1 antibodies [anti-LKM-1s]), iron panel, ceruloplasmin and alpha-1-antitrypsin levels, and thyroid stimulating hormone (TSH). All serology was normal. Finally, a liver biopsy obtained scant liver tissue in an amount insufficient for diagnosis. This made it necessary to obtain a liver wedge through a laparoscopic surgical approach. Its histological analysis was as follows: areas of regenerative nodular hyperplasia with large-cell change and focal septal fibrosis, consistent with incomplete septal cirrhosis (Fig. 1). The patient was diagnosed with non-cirrhotic portal hypertension (NCPH) secondary to incomplete septal cirrhosis. Four years later, he continues to undergo ultrasound check-ups and gastroscopy to monitor his varices, and he remains stable.
(A) Magnification (2×) with haematoxylin and eosin staining showing areas of regenerative nodular hyperplasia and delicate fibrous septa which are often incomplete. (B) Greater magnification (10×). (C) Masson's trichrome staining showing periportal fibrosis with no visible connections with other portal tracts.
Incomplete septal cirrhosis was first reported by Popper in 1966 as a type of macronodular cirrhosis in which fine and incomplete septa delineate rudimentary nodules of regeneration.1 At present, this extremely uncommon disease is included in the histological forms responsible for NCPH.2
NCPH is a rare disorder characterised by increased intrahepatic portal pressure in the absence of cirrhosis, other causes of liver disease and thrombosis of the splenoportal axis. It comprises a broad spectrum of non-specific histological characteristics, which range from minor changes, sinusoidal dilatation and phlebosclerosis to portal fibrosis and nodular hyperplasia, and which today define each one of the forms responsible for NCPH: incomplete septal fibrosis, hepatoportal sclerosis, perisinusoidal fibrosis, obliterative portal venopathy and regenerative nodular hyperplasia. However, it is not clear whether these histological changes are diagnostic of different entities which share a single clinical presentation, or instead reflect different stages of the same disease.
The most common form of NCPH is regenerative nodular hyperplasia, reported above all in association with systemic diseases or use of medicines, and identified by regenerative nodules in the absence of fibrosis.2,3 However, incomplete septal cirrhosis represents a much more unusual pathological finding for which there are hardly any references.1,4,5
Incomplete septal cirrhosis is characterised by a vague nodularity with thin incomplete fibrous tracts surrounding nodules of regeneration, hypoplastic portal spaces with no inflammation, enlarged efferent veins and sinusoidal dilatation.5 Sometimes a differential diagnosis with other entities is nearly impossible, especially in fine-needle biopsies, and may only be suggested. It should be noted that its typical characteristics may be missing or incomplete in a simple biopsy and its recognition may be underestimated; therefore, a sample obtained through laparoscopy proves much more useful.
Overlapping traits of this and other forms of NCPH have been reported. Nakanuma et al. re-evaluated 107 liver biopsies with NCPH in Japan, and classic characteristics of incomplete septal cirrhosis were reported in just 25 cases, which in addition presented other traits shared with partial nodular transformation. This raised the question of whether these could be different stages of the same disease.6 In the same vein, our patient's biopsy also showed areas of regenerative nodular hyperplasia. This, too, raised the possibility of diagnosis of progressive forms of the same entity. The co-existence in a single biopsy of regenerative nodular hyperplasia and incomplete septal cirrhosis has been previously reported in the literature in a patient with autoimmune hepatitis treated with azathioprine. The authors believe that incomplete septal cirrhosis could be the result of regression of fibrosis following hepatic aggression.7 Recently a case was published of septal cirrhosis in a patient with multiple sclerosis treated with corticosteroids, which reversed after treatment was stopped. This supports the notion that this entity represents a dynamic, not necessarily progressive process, if not the notion that in some patients it is postulated as a stage of regression of fibrosis.4
In conclusion, our case featured the uncommon finding of 2 different histological entities—regenerative nodular hyperplasia and incomplete septal cirrhosis—in a patient with NCPH. This could bolster the idea that these are in reality different phases of the same disease, related to the process of progression or involution of hepatic fibrosis.
Please cite this article as: Martín-Lagos Maldonado A, Guilarte López-Mañas J, Vergara Alcaide E, Vinuesa Guerrero MD. Cirrosis septal incompleta: una condición infrecuente. Gastroenterol Hepatol. 2018;41:371–372.