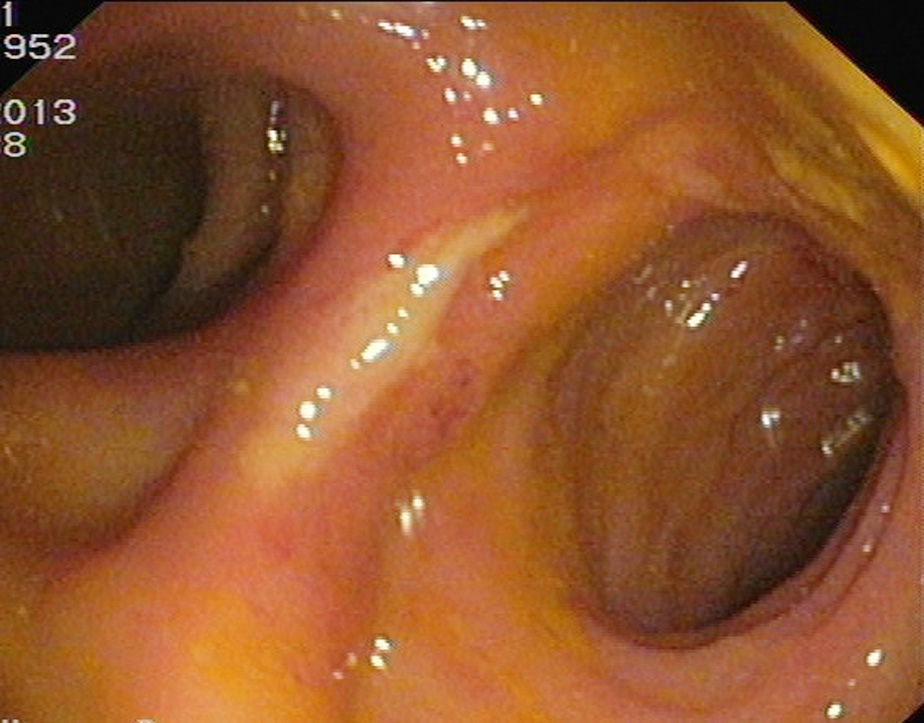
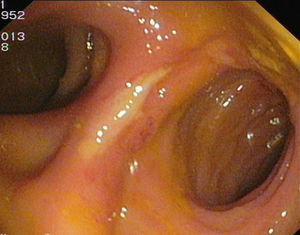
A 61-year-old woman was examined in outpatients for diarrhoea. Her personal history included total hysterectomy and double adnexectomy for endometrial adenocarcinoma two years previously. During the post-operative period, she had presented symptoms of bowel obstruction due to adhesions that required surgical intervention with adhesiolysis. She subsequently received chemotherapy and radiotherapy (RT). She reported no other surgical history. The patient presented with a six-month history of cramping abdominal pain accompanied by increased bowel movements of 6–7 watery stools daily with defecatory urgency. Colonoscopy was performed which revealed, 15cm from the anal margin, an ulcerated ileocolic anastomosis, which, in the image, had a surgical appearance (Fig. 1). The scope was advanced a further 30cm through a loop of small intestine, encountering an abundant flow of liquid content. The colonoscope was withdrawn through this loop and was advanced to the caecum, but no other abnormalities of note were found. In view of these findings, the patient was again questioned and her medical record reviewed, but no history of abdominal bowel surgery could be confirmed. A barium enema was injected and the contrast flowed through a short stenosis, observed at the level of the rectosigmoid junction, in three directions: towards the left colon, along the ileum and from the upper side to end in a blind loop (Fig. 2). The patient was diagnosed with ileocolic fistulas secondary to RT and offered surgical treatment. She opted for conservative therapy, since her symptoms were well controlled by symptomatic medical treatment.
Ileocolic fistulas are rare and most are due to surgical procedures, inflammatory bowel disease or RT. RT for the small intestine and colon can cause lesions such as adhesions, stenosis, ulcers or fistulas. Furthermore, previous surgery may cause loops of the small intestine to be less motile and so enhance the effect of radiation.1 Although the time between RT and the onset of clinical manifestations of intestinal damage cannot be predicted, three phases are evident: the acute phase, in which the mucosa is damaged; the sub-acute phase, in which the submucosa is predominantly affected; and the chronic phase, in which the entire intestinal wall becomes lesioned.2 The start and duration of each phase depends on the type and dose of radiation, with the chronic phase usually occurring three or four years after the RT.3 When fistulas form, depending on the intestinal segments they join, they may be asymptomatic, an incidental finding in complementary examinations, or they may become symptomatic, with a negative impact on nutrition and quality of life. Fistulas following RT do not tend to resolve spontaneously, so treatment is usually surgical.4 Because surgery of this type of fistula is complicated, cases need to be assessed on an individual basis. In our patient, the morphology of the fistula resembled surgical anastomosis. Due to the connection between distal and proximal sections, surgical treatment has not been entirely ruled out, but depends on how the patient's symptoms evolve.
Conflict of interestsThe authors declare that they have no conflict of interests.
Please cite this article as: Alcaide N, Velayos B, González Redondo G, Berroa de la Rosa E, Macho Conesa A, Fernández Salazar L, et al. Fístulas ileocólicas tras radioterapia por carcinoma de endometrio. Gastroenterol Hepatol. 2016;39:23–24.