Splenic rupture of traumatic origin is the most frequent and known cause of spleen injury; however, this haematological organ can rupture in the absence of trauma in spleens with parenchymal involvement due to neoplastic processes, haematological diseases or other infectious affections.1
Rupture of neoplastic origin is exceedingly rare, with few references in the bibliography, the most common cause being the primary lymphoproliferative processes of the spleen,2,3 although other types of tumours are even rarer.4
The etiopathogenesis of non-traumatic rupture is triggered by an increase in the size of the spleen, increases in the pressure of the splenic artery territory, or pathological infiltration of the splenic hilum.3,5
Clinically, we must suspect a splenic rupture in patients with pain in the epigastrium and left hypochondrium radiating to the back, with evidence of peritoneal irritation which, in many cases, evolves very quickly to shock with hypotension and tachycardia.
With clinical suspicion, the diagnosis must be confirmed with ultrasound, and in those patients with haemodynamic stability, an abdominal CT scan is recommended.
The gold standard treatment is emergency splenectomy.
We present the case of a 75-year-old man with hypertension and no other medical history of interest, who visited the emergency department for abdominal pain in the left upper quadrant that radiated to the ipsilateral shoulder for 12 h, associated with a fever of 38°C. In the anamnesis, he reported melenic stools and weight loss of around 10 kg in the last six months.
On physical examination, the patient's general condition was normal with pale mucous skin and systolic blood pressure of 90 mmHg and 120 bpm. The abdomen was soft and depressible with pain and defence in the left hypochondrium. Bowel sounds were diminished.
Analytically, a haemoglobin of 7 g per decilitre, 17,000 leukocytes with neutrophilia and a high CRP stood out.
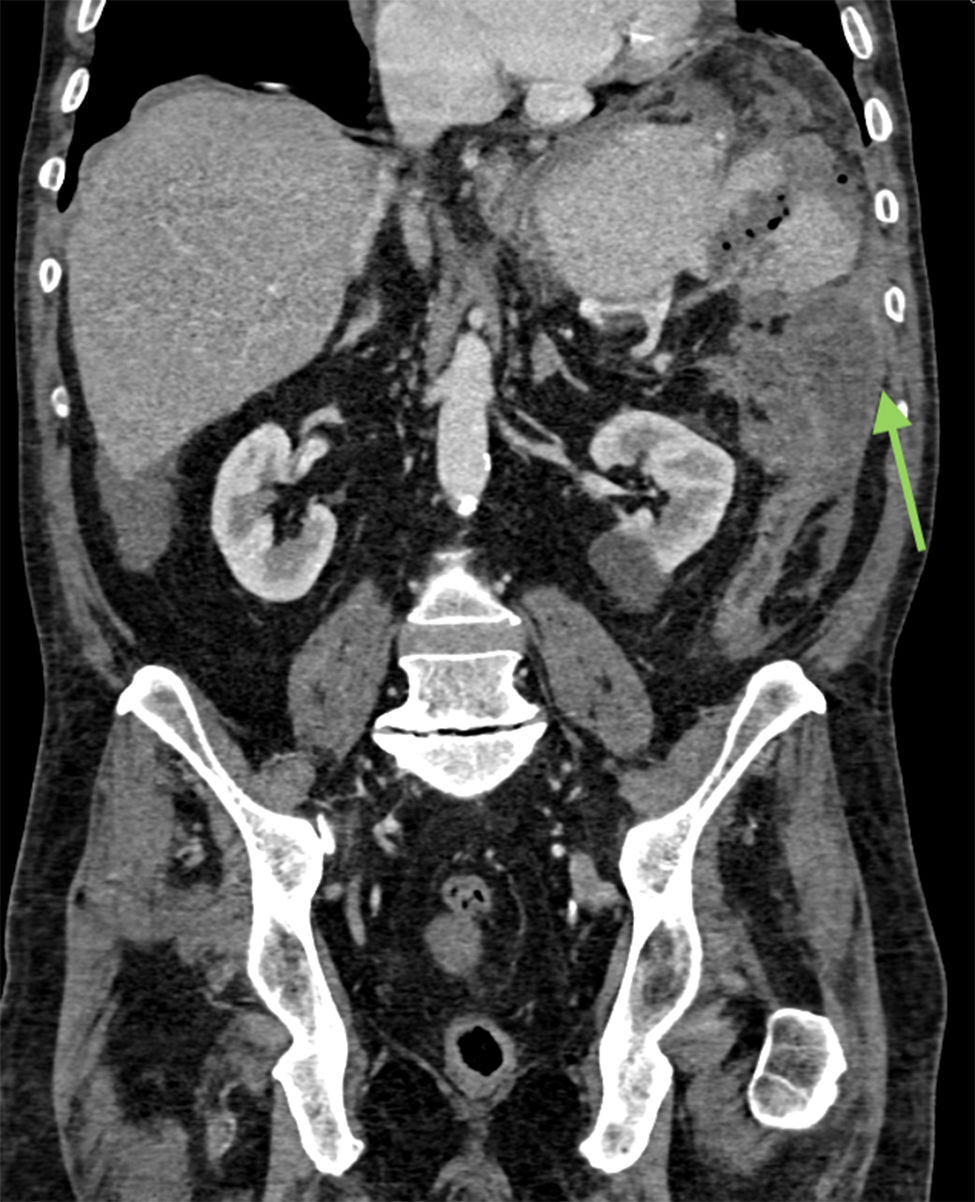
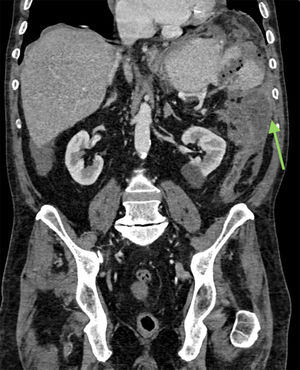
Two peripheral venous cannulae were inserted, and volumetric resuscitation with lactated Ringer's solution was started, improving the blood pressure figures and correcting the tachycardia, owing to which, given the haemodynamic stability, an abdominal CT scan was performed; this revealed a large splenic haematoma with a grade IV splenic laceration (Fig. 1), with abundant hemoperitoneum and a thickening of the splenic flexure of the colon (Fig. 2).
An urgent laparotomy was indicated, revealing a hemoperitoneum with a tumour of around 10 cm that encompassed the splenic flexure of the colon and spleen, with involvement of the hilum and splenic parenchyma, as well as infiltration of the left adrenal gland and the tail of the pancreas, performing an en bloc resection of the splenic flexure of the colon, spleen, tail of the pancreas and left adrenal gland.
The patient responded favourably and was discharged on the 7th day post-surgery.
The pathological study of the specimen showed a poorly differentiated adenocarcinoma of the colon, with associated lymphovascular invasion and three positive lymph nodes out of 33, with all the resection margins free of tumour. The patient subsequently received adjuvant chemotherapy, and six months after surgery he is disease free.
Non-traumatic rupture of the spleen is extremely rare, with very few cases described in the literature, although when the underlying cause is neoplastic, the main aetiology is lymphoproliferative processes at the splenic level.1,3
The presentation of splenic flexure colon cancer as haemorrhagic shock secondary to splenic rupture is even more unusual, with no references in the literature.
The aetiopathogenesis of non-traumatic splenic rupture is poorly understood, but there are several theories that establish that it is of multifactorial origin due to an increase in the size of the spleen, association with splenic infarcts, coagulation disorders, tumour infiltration of the spleen, haematological diseases with splenic involvement and infectious processes.1,2,5 Any pathological process that entails an increase in pressure in the vascular territory of the spleen may be the trigger for its rupture, and cases of compression rupture of the spleen due to contraction of the diaphragmatic and abdominal muscles that occurs in the Valsalva mechanism have even been described.3,5
The rarity of the case is not the primary tumour -since colorectal cancer represents the neoplasm with the highest incidence in men and women in Spain, and is usually diagnosed in earlier stages due to symptoms of alterations in stool habits, weight loss and blood in the stool-but rather the form of presentation, since the diagnosis was made intraoperatively when it was found that the colonic tumour had infiltrated the hilum and splenic parenchyma, leading to its rupture, with the consequent situation of haemorrhagic shock.
In conclusion, despite the rarity of the condition, we must suspect a ruptured spleen in the emergency department in the absence of trauma as a cause of sudden abdominal pain in ICH, which characteristically radiates to the back and left scapula and can evolve rapidly to hypovolemic shock, with surgery being the treatment of choice.
FundingThe authors declare that they have not received funding to carry out this work.
Please cite this article as: Soto-Darias IC, López-Fernández J, Fettane-Gómez S, Pérez-Alonso E, Hernández-Hernández JR. Shock hemorrágico secundario a rotura esplénica no traumática como forma de presentación del cáncer de ángulo esplénico. A propósito del caso. Gastroenterol Hepatol. 2020;43:519–521.