Gastrointestinal perforation is often considered a complication of endoscopic procedures. Nevertheless, non-iatrogenic perforations may also occur and their management is frequently challenging. Data about the management of non-iatrogenic gastrointestinal perforations are still scarce.
A 74 years-old female was referred to the emergency department with thoracic pain after esophageal fishbone impaction. Diagnosis was made by an upper digestive endoscopy performed in an outpatient basis. No fever or other symptoms were present. Cervical-thoracic computed tomography (CT) revealed a 34mm fishbone located transversally between the right branch of the pulmonary artery and descendent aorta, at about 6mm of each vessel (Fig. 1). After a multidisciplinary discussion, an endoscopic therapeutic approach was proposed. An upper digestive endoscopy revealed a V-shaped fishbone penetrating the esophageal wall in contralateral points. With the use of an overtube, the foreign body was endoscopically removed by a foreign body forceps. Endoscopic revaluation revealed two contralateral perforations. A totally covered self-expandable metallic stent (SEMS) – Hanarostent CCC 20mm×110mm was then placed over the referred perforations. The patient remained hospitalized during 2 weeks, with a favorable evolution. The SEMS was then removed one month later, revealing complete closure of the referred perforations.
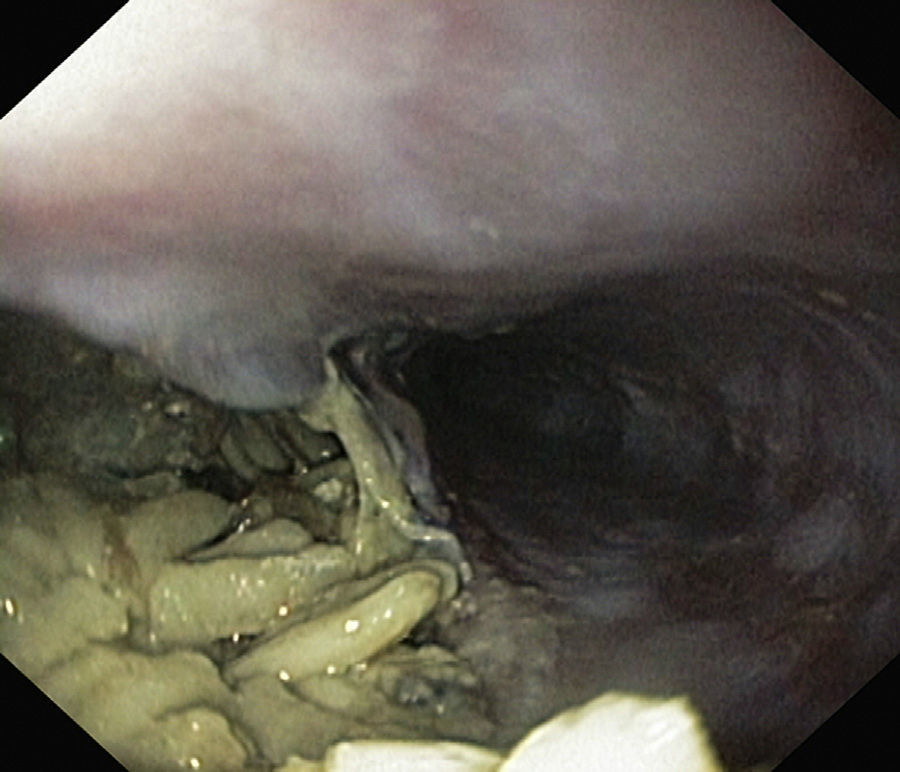
A 69 years-old female was referred to the emergency department with a strong post-prandial epigastric pain lasting for about 1h. A thoracic CT revealed an esophageal perforation with a massive pneumomediastinum. After a multidisciplinary discussion a therapeutic upper endoscopy was proposed. It confirmed a 5cm wide esophageal perforation through which a large amount of food was seen in mediastinum (Fig. 2). A two-step approach was then decided: a surgical drainage was performed and then a totally covered SEMS (Hanarostent CCC 20mm×140mm) was placed over the referred perforation. The patient remained hospitalized for 10 days, with a favorable evolution. The SEMS was easily removed six weeks later. Complete healing of the laceration was observed.
A 67 years-old female was referred to the emergency department with an intense constant abdominal pain lasting for about 24h. No fever, chills or others symptoms were present. CT revealed sigmoid wall thickening with an apparent foreign body (bone) and an adjacent gas collection with 22mm. After discussion, a therapeutic colonoscopy was performed. A foreign body (bone) penetrating the colonic wall was seen and removed with a foreign body forceps. The point of bowel perforation was not identified in the endoscopic re-evaluation. The patient was treated with NPO and empiric antibiotics. She was discharged about 2 weeks later, with no complications.
Gastrointestinal perforation consists in a rupture of the gastrointestinal tract wall. Although this condition may be readily recognized, it is not always evident. This is particularly relevant for non-iatrogenic perforations. An early diagnosis allows a prompt and optimal management.1
The management of gastrointestinal perforation is often challenging and complicated. Nevertheless, some aspects may be globally considered.
Broad-spectrum antibiotics, intravenous hydration and nothing per mouth are regularly considered in gastrointestinal perforations. Nasogastric or nasojejunal tube placement is recommended in gastric, duodenal and proximal small-bowels perforations.1 This conservative approach is commonly considered an adjunctive therapy. Surgical repair has been considered the gold standard in the management of gastrointestinal perforations. Nevertheless, this approach carries a significant morbidity and mortality. Endoscopic management of gastrointestinal perforations is being increasingly adopted in clinical practice. The latter is also deemed as an adjunctive therapy for a surgical approach.
Currently, there are some possibilities for endoscopic management of gastrointestinal perforations, which may be used in iatrogenic and non-iatrogenic perforations. Factors like the location, dimension, duration and etiology of the gastrointestinal perforation influence the selection of the method.
Recently, self-expandable metallic stent (SEMS) became a popular option in the management of gastrointestinal perforations. Although it may be used in other locations, it is mostly used in the esophagus. Fully covered SEMS, partially covered SEMS and plastic stents have similar efficacy for the management of benign esophageal perforations.2 In the esophagus, SEMS applicability and clinical success are very high. Its complication rate is substantial but it is associated with a very low stent-related mortality.2
Through-the-scope (TTS) clips have an established role in the management of gastrointestinal perforations.3 TTS clips are frequently used in gastrointestinal perforations with a high applicability and acceptable outcomes.4,5 Nevertheless, TTS clips were not designed for gastrointestinal closure and their ability to perform a convenient transmural sealing is still debated. The over-the-scope-clip (OTSC Ovesco®) has revealed good results in the management of gastrointestinal perforations.6,7 Considering its dimensions and design, it is considered to provide a better sealing quality, comparable to a manual surgical suture.7
Other endoscopic techniques, namely the omental patch method, suturing and stapler devices and biological glues have also been described for the management of gastrointestinal perforations.8 Nevertheless, more data are still needed.
Non-iatrogenic gastrointestinal perforations are a feared condition in clinical practice. Their management should be discussed in a multidisciplinary basis and a conservative, endoscopic and/or surgical approach is possible. The need of a high level of expertise and specific devices are the major limitations for an endoscopic approach.
FundingNothing to declare.
Conflict of interestNothing to declare to all the authors.
Nothing to declare.