Chilaiditi sign is characterised by interposition of the intestine (usually the hepatic angle of the colon) between the liver and right hemidiaphragm. It is a rare entity that was first described by Demetrius Chilaiditi, a Greek radiologist, in 1910.1 It is more common in men (4:1 ratio), and is generally an incidental finding that appears in between 0.02% and 0.14% of radiological studies performed for any reason.2 Its cause is unknown, although it is probably multifactorial.
Chilaiditi sign is asymptomatic. When associated with symptoms, it is called Chilaiditi syndrome. The most common symptoms are digestive: vomiting, anorexia, constipation and bloating. It can also be associated with respiratory symptoms like dyspnoea or pleuritic pain. As the physical examination is usually unremarkable, it is often underdiagnosed.3
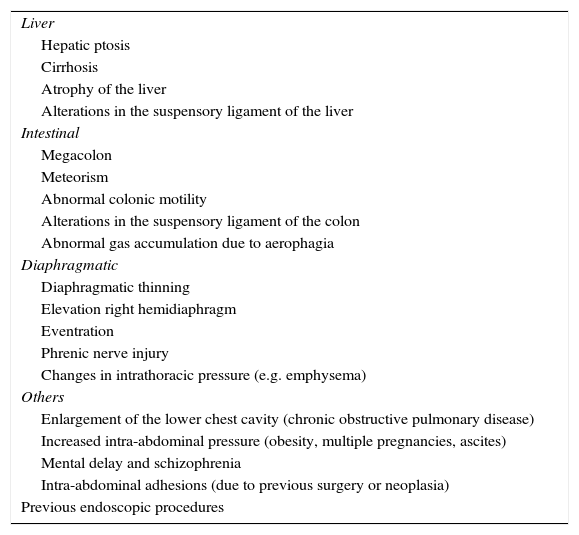
The suspensory ligaments and fixation of the colon normally impede interposition of the colon between the liver and diaphragm. Chilaiditi syndrome has been associated with several predisposing factors (Table 1) that can change the relationship between the liver, colon and diaphragm.2,4
Predisposing factors for Chilaiditi syndrome.
| Liver |
| Hepatic ptosis |
| Cirrhosis |
| Atrophy of the liver |
| Alterations in the suspensory ligament of the liver |
| Intestinal |
| Megacolon |
| Meteorism |
| Abnormal colonic motility |
| Alterations in the suspensory ligament of the colon |
| Abnormal gas accumulation due to aerophagia |
| Diaphragmatic |
| Diaphragmatic thinning |
| Elevation right hemidiaphragm |
| Eventration |
| Phrenic nerve injury |
| Changes in intrathoracic pressure (e.g. emphysema) |
| Others |
| Enlargement of the lower chest cavity (chronic obstructive pulmonary disease) |
| Increased intra-abdominal pressure (obesity, multiple pregnancies, ascites) |
| Mental delay and schizophrenia |
| Intra-abdominal adhesions (due to previous surgery or neoplasia) |
| Previous endoscopic procedures |
It is important to identify the presence of Chilaiditi sign in patients with predisposing factors in order to minimise iatrogenesis, as in the case of percutaneous transhepatic procedures or liver biopsy in cirrhotic patients or during colonoscopies.
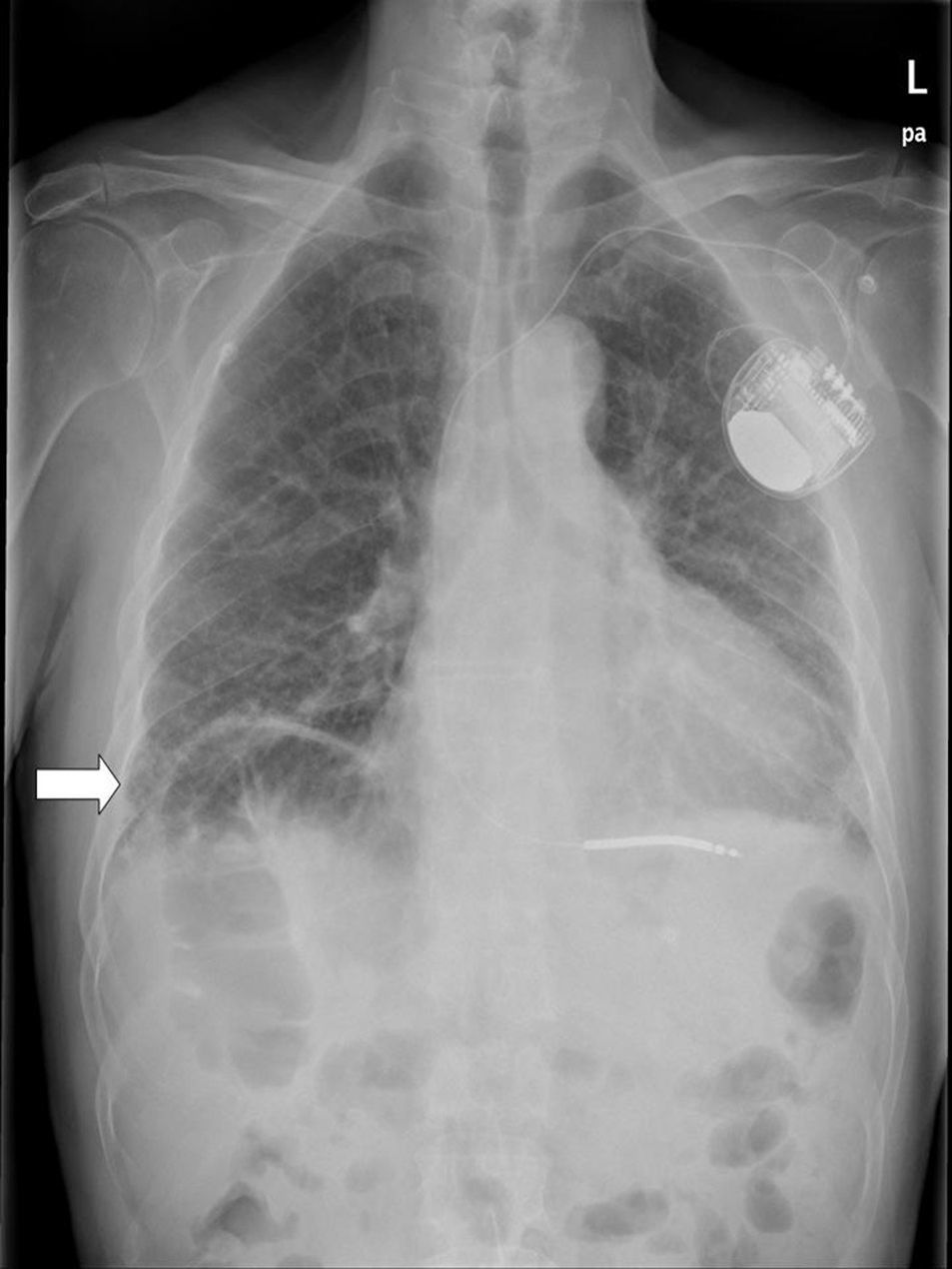
Hepatodiaphragmatic interposition is generally diagnosed by plain X-ray. The typical image shows air below the diaphragm, with visible haustra between the liver and surface of the diaphragm (Fig. 1). In case of diagnostic uncertainty, the location of the air will not change when the patient changes posture.
Differential diagnosis should be made mainly with pneumoperitoneum, typically seen on X-ray as a half-moon shape extending below the diaphragm, with no visible haustra, and which changes with posture.
Other entities that should be included in the differential diagnosis are subphrenic abscess, intestinal pneumatosis, infected hydatid cyst and liver tumour.2 Cases have also been documented with symptoms similar to renal colic, so this should also be considered in the differential diagnosis of this disease.
In the case of diagnostic uncertainty, ultrasound or computed axial tomography are the most commonly used additional studies.
No treatment is required in the case of asymptomatic patients. In cases of Chilaiditi syndrome with no severity criteria, treatment is initially conservative: bed rest, decompression with a nasogastric tube, intravenous fluids, enemas, laxatives and discontinuation of potentially related medication. Despite treatment, 26% of symptomatic patients eventually require surgery (colectomy, hepatopexia or colopexia).5,6
Please cite this article as: de Pablo Márquez B, Pedrazas López D, García Font D, Roda Diestro J, Romero Vargas S. Signo de Chilaiditi. Gastroenterol Hepatol. 2016;39:361–362.