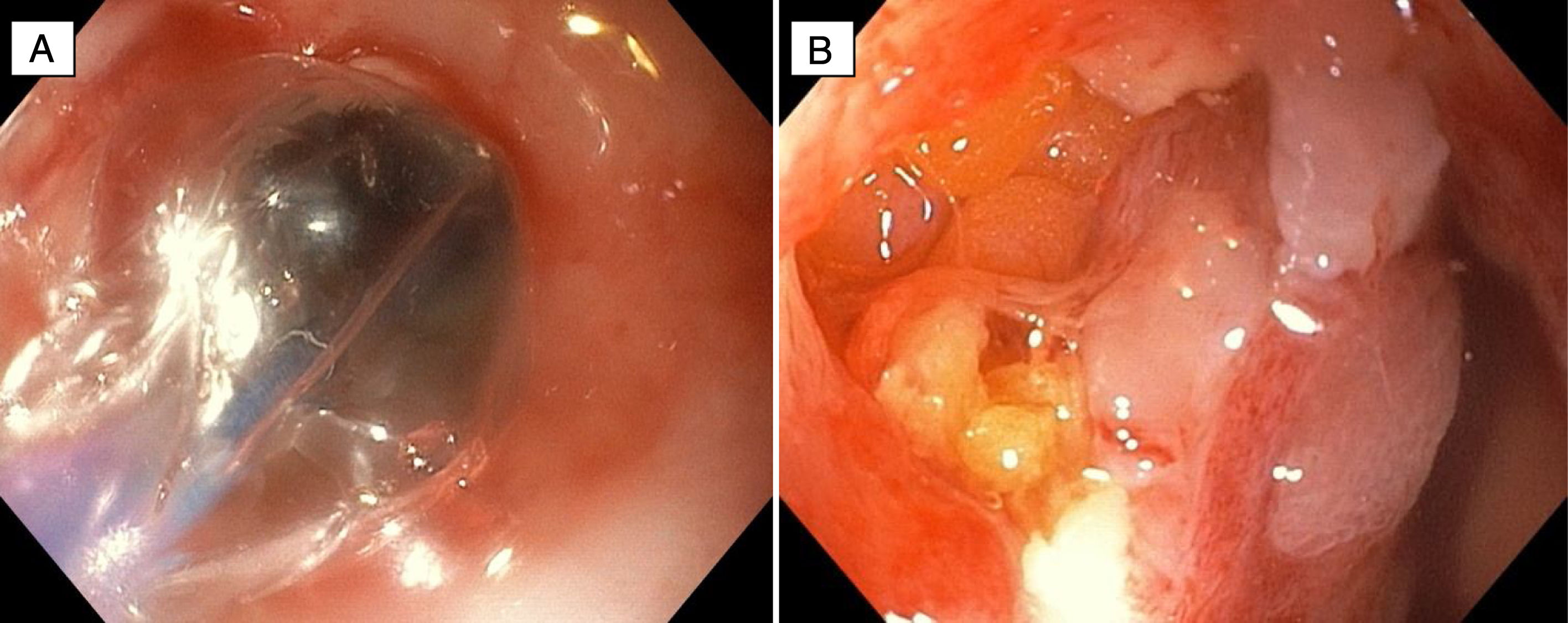
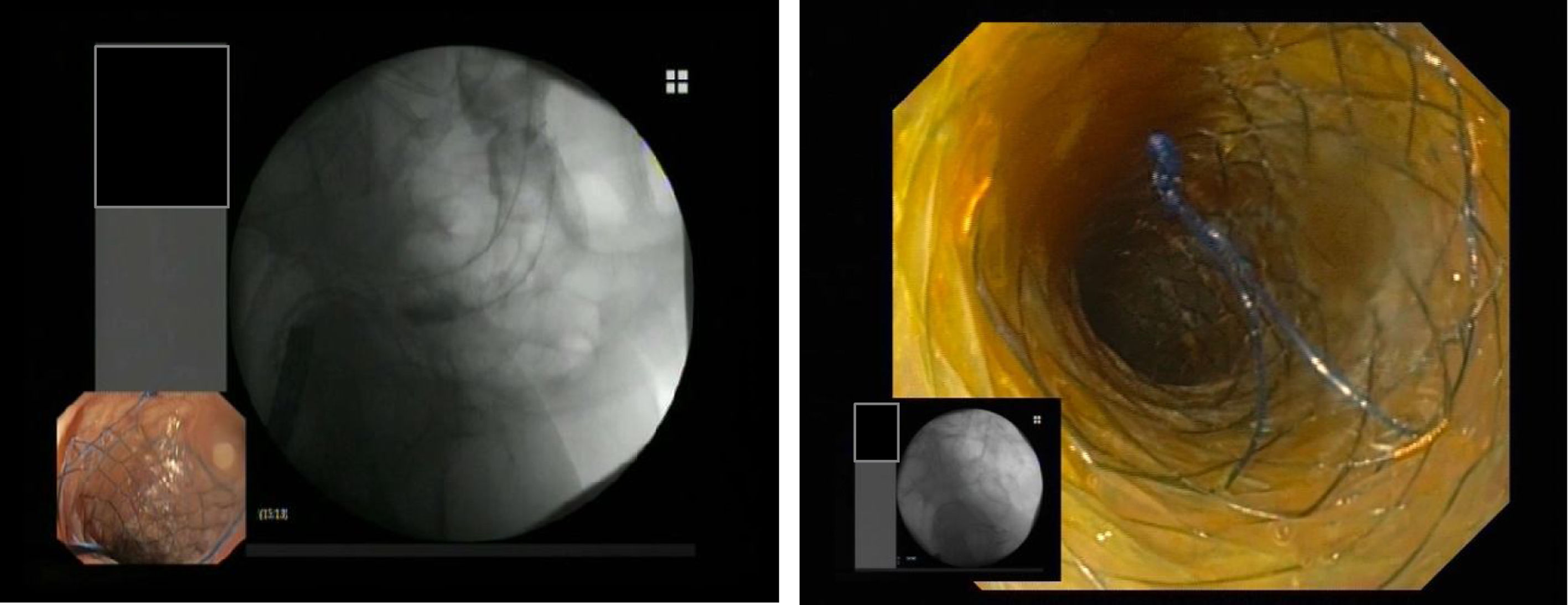
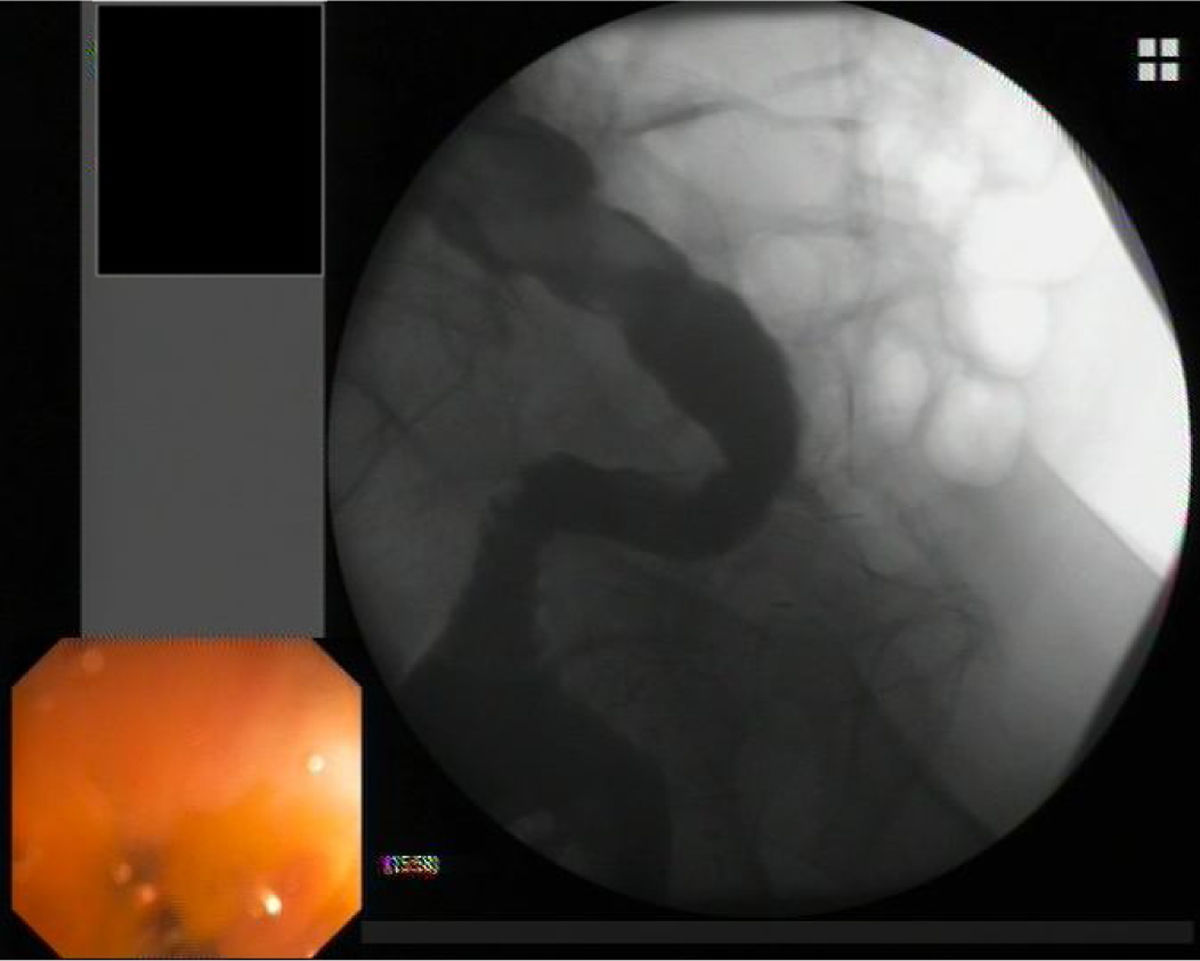
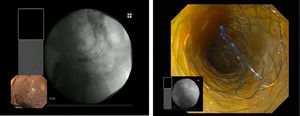
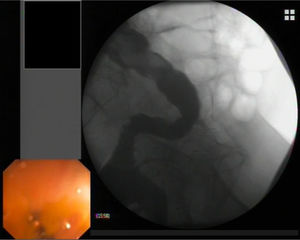
We present a 75-year-old man with a 20mm length×8mm width colonic stenosis after radiotherapy for prostatic adenocarcinoma at 15cm of anal margin. In the second pneumatic dilation (12–15mm) a perforation was produced (Fig. 1). The patient was treated with a guided 20-130-23mm covered self-expandable metallic stent (CSEMS). Four days after, the patient reported tenesmus. A new endoscopy showed the migration of the stent with the leakage still covered. A second CSEMS “stent in stent” was placed (Fig. 2). After 10 days both protheses were removed with perforation and stenosis resolution (Fig. 3).
Due to the increase in the number of colonoscopies, its associated perforations have raised.1 CSEMS use in colonic perforations has been anecdotally reported.2 On the other hand, CSEMS represents a stabilised therapeutic option for colonic stenosis.3 An advantage of CSEMS is that it can be easily removed; however, the probability of migration is up to 42%.4 Thus, perforations of the proximal colon or without stenosis represent a non-candidate for the use of CSEMS. In conclusion, CSEMS can be an effective therapeutic option for the management of distal colonic perforation in a patient with post-radiotherapy stenosis, allowing the resolution of both perforation and stenosis.
Conflict of interestThe authors declare no conflicts of interest.
To all the endoscopy team, doctors, nursing and auxiliaries.