Inflammatory bowel disease (IBD) is an independent risk factor for the onset of thromboembolic events (TE). We know that TE are extraintestinal manifestations that significantly increase morbidity and mortality in these patients.
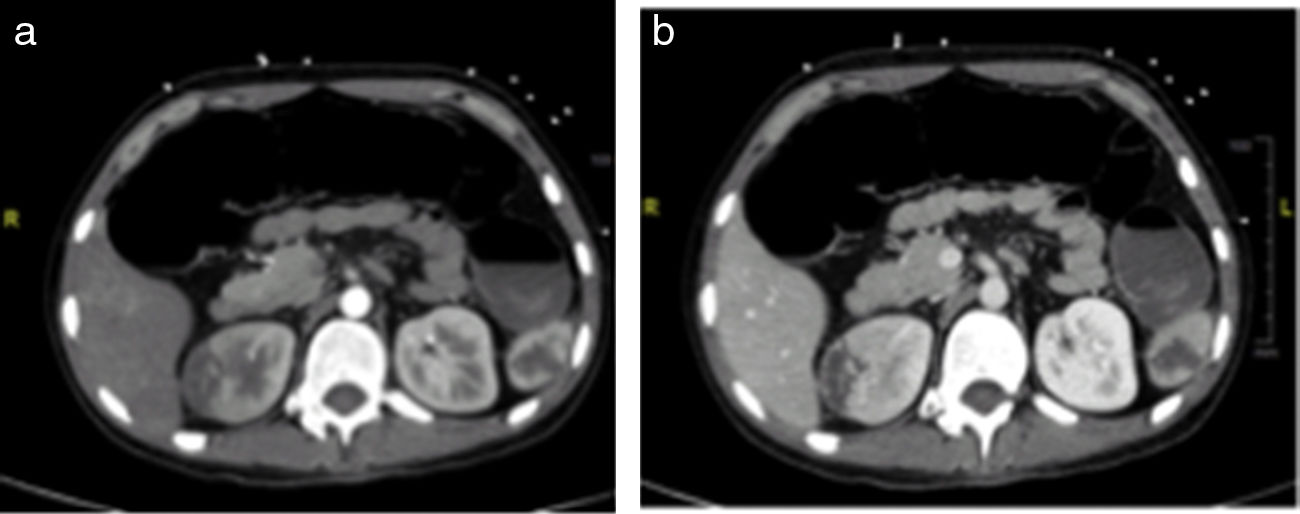
Case reportOur case study is that of a 19-year old male patient with no substance abuse, recently diagnosed with Crohn's ileocolitis during a moderate flare-up, and receiving outpatient treatment with corticosteroids and azathioprine. He came to the Emergency Department with chest pain associated with autonomic signs and symptoms of onset a few hours earlier. The electrocardiogram showed ST segment elevation with morphology characteristic of a subepicardial injury in V1–V4. Additional findings included increased cardiac enzymes revealed in blood tests and an emergency echocardiography suggestive of extensive anterior wall myocardial infarction. Emergency catheterisation was performed, revealing a thrombotic occlusion of the middle segment of the left anterior descending artery which was treated with a drug-eluting stent. In addition, dual antiplatelet and anticoagulation therapy with acenocoumarol was started. During this episode, he underwent CT angiography, which revealed a renal and splenic infarction and hepatic and colonic perfusion disorder (Fig. 1). The antiphospholipid antibodies, factor deficiencies (protein C, protein S and antithrombin III), mutations associated with thrombophilias (Factor V Leiden, prothrombin) and homocysteine levels were negative or in the normal range. Following his recovery from the acute episode, the patient continued receiving the anticoagulation. The course of the Crohn's disease was indolent; the patient developed a complex perianal fistula and abscesses, requiring surgical drainage and combined treatment with biological therapy and immunosuppressants to control the disease.
DiscussionVenous and arterial thromboembolism is an extraintestinal manifestation which significantly increases morbidity and mortality in patients with IBD.1 TE are 3 times more common in patients with IBD than in controls, and the relative risk increases 15-fold in disease flare-ups.2 These patients have an increased risk of developing coronary artery disease, at younger ages and without associated cardiovascular risk factors,3 as in the case of our patient. Although the principal hypothesis is that the inflammation maintained by the IBD flare-up causes an acceleration of the process of atherosclerosis and development of thrombosis,4 the underlying thrombotic mechanism is complex, multifactorial and not completely elucidated.
There are some related acquired factors such as treatment with corticosteroids, prolonged bed rest or canalisation from central venous catheters. It has also been speculated that certain genetic mutations in thrombosis factors could be the cause of increased TE in these patients. However, none of these is more common in patients with IBD than in the general population.4 Therefore, the genetics of thrombophilia does not explain the increased risk of TE in IBD, which indicates that the role of the acquired factors is relevant. In spite of this, we should investigate genetic coagulation abnormalities when they lead to TE because abnormalities in certain coagulation factors and fibrinolysis and in platelets have been observed in IBD.1,2 Numerous studies have been conducted to investigate abnormalities in the coagulation cascade, its natural inhibitors and the components of the fibrinolytic system, and quantitative and qualitative changes have been demonstrated. Recently, the role of platelets and the microvascular endothelium, as well as the possible link between the inflammatory and haemostatic process have been reviewed. Therefore, proinflammatory cytokines such as IL-6 and TNFα or CRP stimulate activation of the coagulation cascade. The inflammation represents a state of relative hypofibrinolysis, promoting hypercoagulability.4
However, the indications for prophylactic anticoagulation in IBD are not clearly defined, particularly in younger and paediatric patients. The consensus of the European Crohn's and Colitis Organisation (ECCO) recommends prophylactic anticoagulation for all patients with IBD during hospitalisation and even in outpatients during severe disease flare-ups and with associated risk factors.5 Our patient did not have risk factors or coagulation abnormalities and in spite of that developed a massive thromboembolism. Consequently, there must be other factors which have not yet been defined in these patients which increase predisposition to these events. TE is preventable in many cases, and, therefore, clinicians must understand its importance in patients with IBD.
Conflicts of interestThe authors declare that they have no conflicts of interest.
Please cite this article as: Navarro B, Blázquez T, Herreras J, Iborra M. Infarto agudo de miocardio en paciente con diagnóstico reciente de enfermedad de Crohn. Gastroenterol Hepatol. 2019;42:183–184.