Retroperitoneal liposarcoma, which has an incidence of 2.5 per million population, is a rare and usually asymptomatic tumour that may be underdiagnosed and can develop to the point that it compromises the surrounding structures.1
A 65-year-old female patient, with no medical history, who at six months from cystocele surgery attended the hospital with abdominal distension, early satiety, weight loss and pressure in the abdominal cavity in left lateral decubitus. In the physical examination a solid abdominal mass of 15×20cm was palpated. A blood test, abdominal computed tomography (CT) and endoscopic ultrasound were performed.
The blood tests revealed anaemia with haemoglobin of 10.5g/dl (11.5–16g/dl), thrombocytosis of 422,000/μl (130,000–450,000/μl), elevated C-reactive protein of 212mg/dl (<5) and an erythrocyte sedimentation rate of 105mm/h (up to 20mm/h).
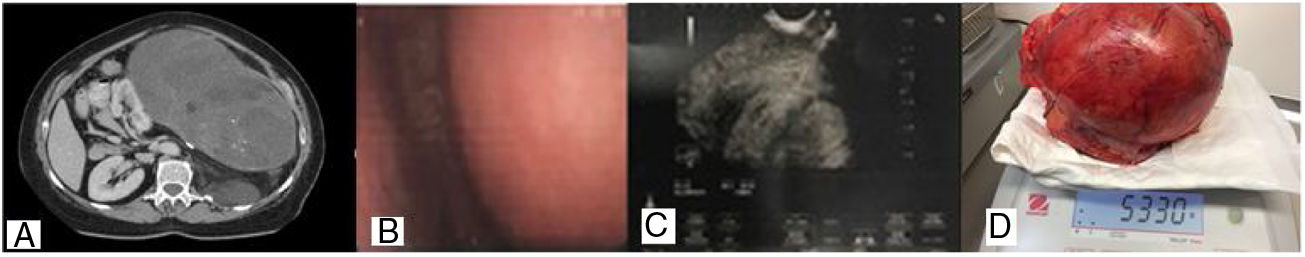
The abdominal CT with contrast showed an encapsulated, heterogeneous abdominal mass of 14cm×23cm with calcifications that was in contact with the tail of the pancreas, the spleen and the left kidney (Fig. 1). The patient presented isolated adenopathy in the hepatopancreatic region of 15mm, with a small quantity of free fluid in the pelvis. The endoscopic ultrasound (5–7MHz) revealed a large, solid, heterogeneous, vascularised and polylobulated retrogastric mass. A fine-needle aspiration biopsy was performed using a Shark-Core 22G (two passes) guided by endoscopic ultrasound to obtain material for a histological study. The histological sample suggested a gastric stromal type mesenchymal tumour with fibroblasts, abundant lymphoplasmacytic cells and occasional histiocytic cells. It was not possible to perform immunohistochemistry (IHC).
A complete resection of the tumour was performed by laparoscopy. The tumour was found to have attached to the left kidney, so a nephrectomy, splenectomy and ligature of the renal and ovarian arteries were performed. Due to its insertion in the diaphragm, the left diaphragm was reconstructed and a pleural drain placed. The patient required a blood transfusion during the surgery.
The extracted tissue revealed a mass measuring 30×23×16cm and weighing 5330g. The histological study revealed a mesenchymal neoplasm with a fusiform pattern and cells with marked pleomorphism. The IHC study was positive for vimentin and S-100 and negative for desmin, actin and CD34; all of this highly suggestive of pleomorphic liposarcoma. The kidney had been partially infiltrated by the neoplasm, while the ureter and the spleen showed no histological signs of malignancy. The patient was assessed by the Oncology Department, who found no recurrence of the tumour on the abdominal CT with contrast performed after the surgery, nor in that performed at six months’ follow-up.
Liposarcoma is the most common retroperitoneal sarcoma. Its incidence is greatest between 40 and 60 years of age and it presents in both genders with a 1:1 ratio.2 It is classified into four subtypes: undifferentiated, pleomorphic, well-differentiated and myxoid.3 The undifferentiated and pleomorphic types are neoplasms with a high degree of malignancy, while the well-differentiated and myxoid types are tumours with a low degree of malignancy.
Abdominal CT with contrast is the imaging test of choice for tumours of this type. Magnetic resonance imaging is reserved for cases where muscular or bone involvement or pelvic disease are suspected. Percutaneous biopsy with a large needle is the gold standard for diagnosis. On occasion, the lesions are not accessible or have a high risk of complications when performing the biopsy. In these cases, imaging-based differential diagnosis is crucial. Due to the variability in the tumour grade, FDG-PET/CT does not play a routine role and is only used when pulmonary anomalies are detected in the CT.4
Surgery continues to be the main treatment for retroperitoneal sarcomas. In most cases, it is necessary to resect one or more organs together with the tumour to achieve complete resection. Frequently, the ipsilateral hemicolon and kidney are resected “en bloc” with the tumour. If it is technically challenging to achieve clear resection margins in surgery, radiotherapy or systemic therapy may be considered to improve local control.5
To conclude, retroperitoneal sarcoma is a rare tumour, liposarcoma being the most common histological type. The absence of specific symptoms makes its diagnosis difficult and its clinical manifestations are caused by compression of the adjacent organs. Complete surgical resection is the treatment of choice.
Please cite this article as: Montenegro A, Varas M, Sánchez-Vizcaíno E, Naval J, Loras C, Abad R. Liposarcoma retroperitoneal gigante con afectación renal: reporte de un caso y revisión de la literatura. Gastroenterol Hepatol. 2019;42:490–491.