Ulcerative jejunitis is typically associated with refractory coeliac disease type II. For its diagnosis, malabsorption-derived symptoms must present in a persistent or recurring fashion for at least six to 12 months from starting a gluten-free diet, after ruling out other reasons for the lack of response.1
Although not the most common scenario, ulcerative jejunitis can be present from diagnosis of the disease.
We present the case of a 62-year-old male, smoker (20 pack-years), drinker (30 g of alcohol/day), with a history of non-insulin dependent type II diabetes.
He was admitted to our hospital for a clinical picture of seven to eight months’ evolution consisting of an increased number of stools (five to six per day) with a soft consistency, persisting nocturnally, without associated abdominal pain or fever.
In the analyses performed, he presented normocytic anaemia and hydroelectrolytic imbalance. Investigations seeking to discern the causes of the diarrhoea revealed positivity for IgA antitransglutaminase antibodies with a level of over 100 U/mL, IgG anti-endomysium antibodies + 1/160 and genetics compatible with coeliac disease (HLA DQ2.5 [DQA1*05, DQB1*02]).
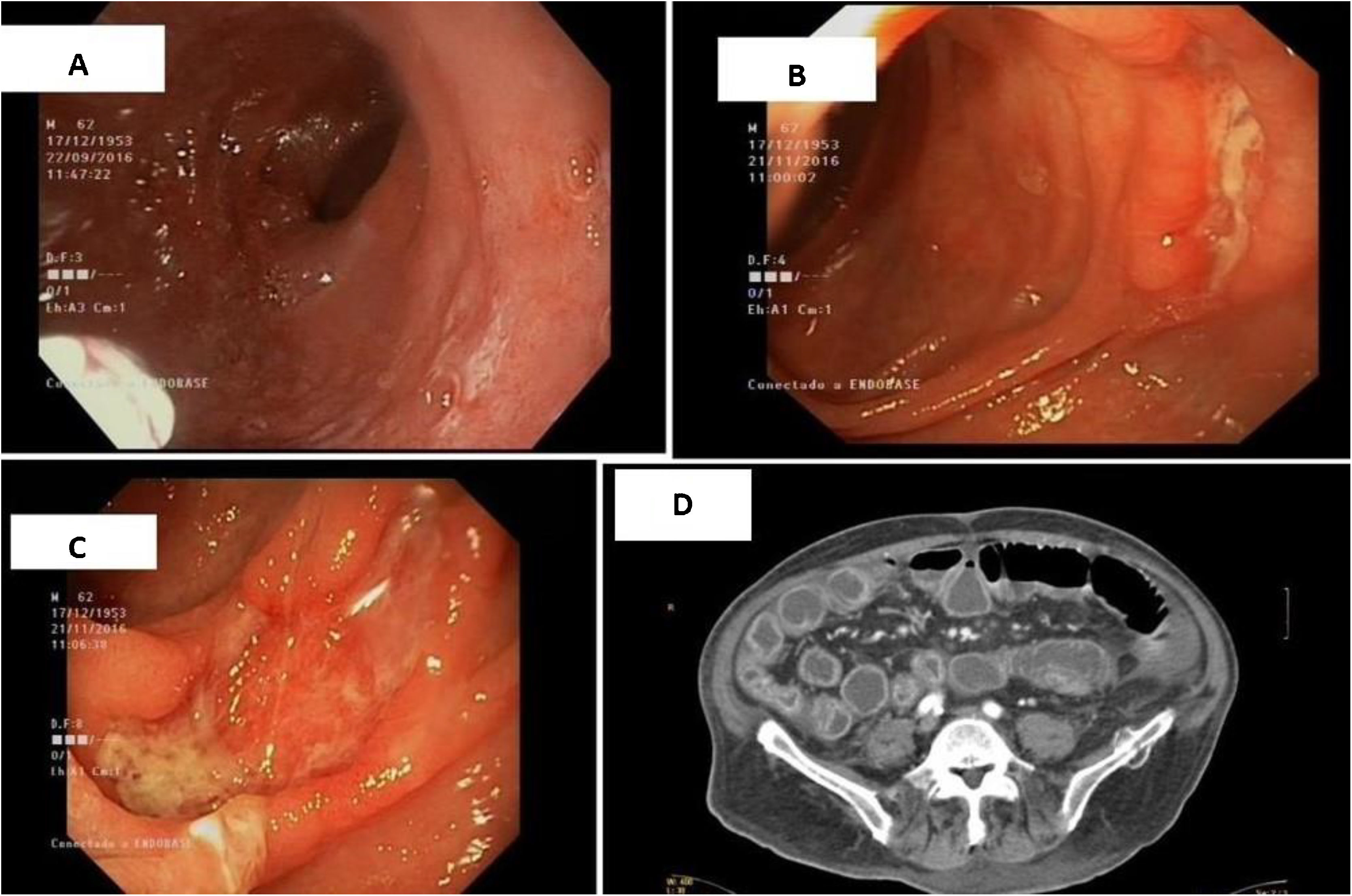
Gastroscopy (high-resolution white-light endoscopy with near focus) showed a bulbar, nodular and atrophic mucosa with small vessels visible in the submucosa (Fig. 1A).
Biopsies revealed a villous to crypt ratio <2:1 with villous atrophy corresponding to grade 3b in the Marsh classification.
In spite of introducing a gluten-free diet, the patient continued to experience diarrhoea, as well as significant and persistent weight loss and analytical alterations.
In view of his worsening clinical picture, computed tomography (CT) was performed, which showed loops of small intestine with marked enhancement in the mucosa and wall thickening (Fig. 1D).
For this reason, the study was expanded using capsule endoscopy, which revealed a multitude of ulcerated lesions of various sizes throughout practically the entire jejunum, associated with atrophy of the intestinal mucosa (Fig. 1B and C). The biopsies were taken by enteroscopy. The histological findings revealed villous atrophy with ulceration of the mucosa and increased inflammatory cells in the lamina propria, which confirmed active chronic jejunitis. They also revealed an increase in number of a population of intraepithelial lymphocytes with an aberrant immunophenotype, evidenced by cytoplasmic CD3 expression and loss of expression of surface makers such as CD3 and CD8, among others. This lymphocyte population was found in a proportion greater than 20%.
In view of the diagnosis of ulcerative jejunitis in the context of a patient with coeliac disease, treatment was initiated with corticosteroids at a dose of 1 mg/kg/day or a total of 70 mg/day for 10 days followed by a tapering regimen.
Following clinical improvement, the patient was discharged and follow-up continued on an outpatient basis, but after five months he was lost to follow-up. He was readmitted due to the reappearance of the clinical picture, associated with weight loss, intense asthenia, cough and expectoration. In recent months, he had continued the corticosteroid regimen at full doses.
During the admission, he was diagnosed with tuberculosis and pulmonary aspergillosis. In spite of the treatment administered, his evolution was poor with gradual deterioration and ultimately death.
Refractory coeliac disease has two subtypes depending on whether the proportion of aberrant intraepithelial lymphocytes present is greater than (type I) or less than (type 2) 20%, for which the clinical course, treatment and prognosis differ. It is often diagnosed from 50 years of age and its incidence varies from 0.04% (type I) to 1.5% (type II).2 As part of the differential diagnosis of this complex condition, it is important to take into account those patients with seronegative coeliac disease, as their condition can evolve to a primarily refractory status and is characterised by a more severe clinical course.3
Whereas type I may be indistinguishable from uncomplicated coeliac disease, type II is more commonly found alongside signs of malnutrition as a result of protein loss due to enteropathy and ulcerative jejunitis. This second type is associated with a worse prognosis and a survival rate at five years of 44%–58%, in particular because of the high risk of transformation to enteropathy-associated T-cell lymphoma.
Video capsule endoscopy plays a fundamental role in the diagnosis of this disease.
The finding of ulcerative lesions in both the duodenum and the jejunum supports the diagnosis of refractory coeliac disease type II, in which immunosuppressant treatment plays a limited role.
In stable patients, the recommended treatment is budesonide (3 mg three times/day). In severe disease, intravenous prednisone (0.5−1 mg/kg/day) is recommended.4
Due to the risk of steroid dependence, drugs such as azathioprine or anti-TNF agents may be used. Nevertheless, although they are associated with clinical improvement, they are not capable of inducing healing of the mucosa due to the lack of impact to the clonal proliferation of intraepithelial lymphocytes. For this reason, medical treatment is challenging, and on many occasions the use of chemotherapeutic agents such as the purine analogue inhibitors cladribine or fludarabine is called for.5
In conclusion, we stress the importance of close follow-up, ideally remotely as well as in-person, of patients with refractory coeliac disease due to the complexity of their management and the importance of anticipating possible complications such as those suffered by our patient.
Please cite this article as: García Mateo S, Velamazán Sandalinas R, Hijos Mallada G, Abad Baroja D, Hernández Ainsa M, Saura Blasco N, et al. Yeyunitis ulcerativa. Manifestación grave e infrecuente en el debut de la enfermedad celíaca. Gastroenterol Hepatol. 2021;44:568–569.