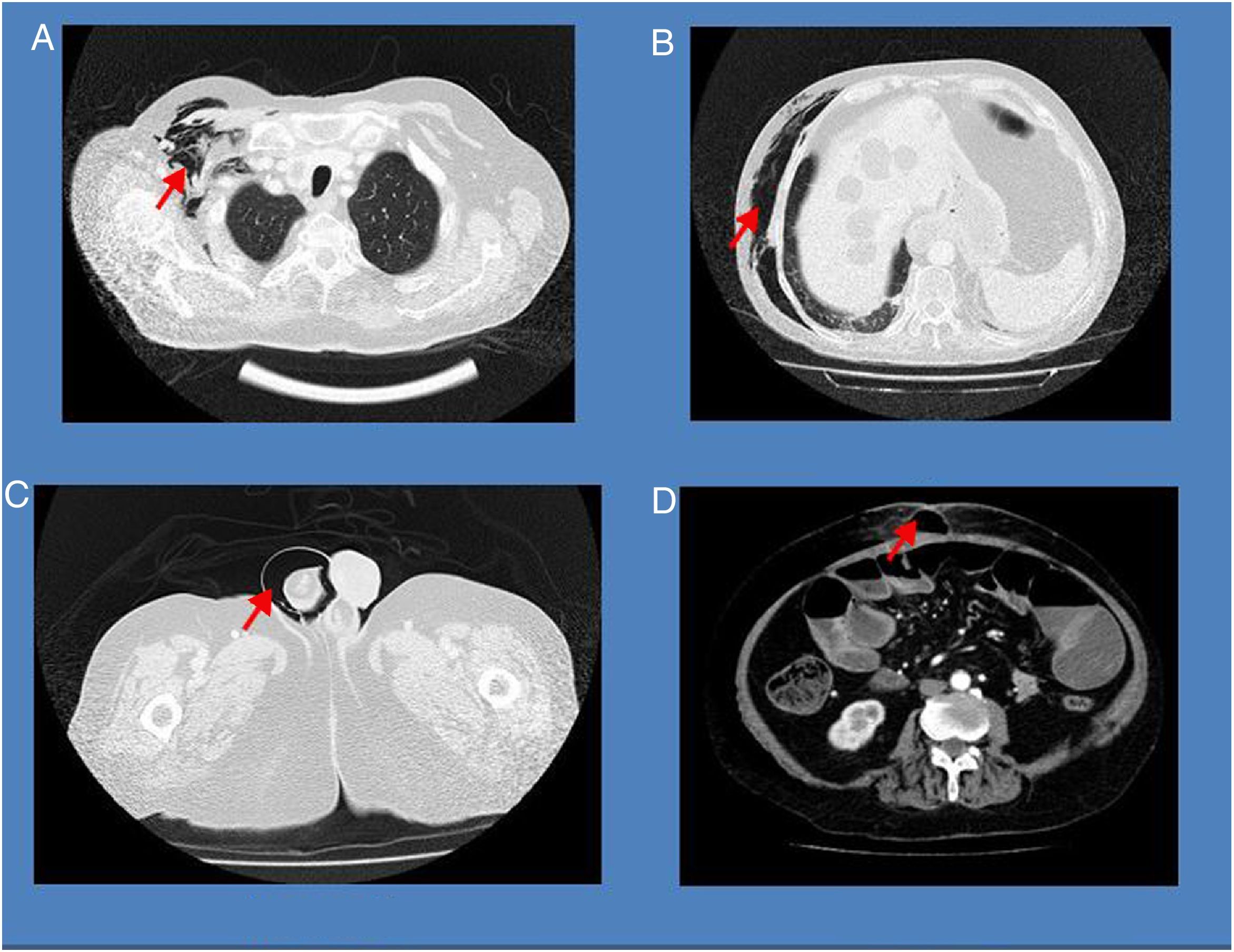
We present the case of a 71-year-old man with long-standing Crohn’s disease (A2B2L3), with stenosis of the distal ileum leading to dilation of the small intestine. He was on treatment with golimumab, azathioprine and prednisone. He was admitted due to signs and symptoms of a partial occlusion with a slowly favourable course. Suddenly, the patient presented a poor general condition and abdominal pain. An examination revealed crepitation of the subcutaneous tissue. An emergency scan revealed the findings below (Fig. 1).
The images show subcutaneous emphysema extending from the right axillary region to the ipsilateral testicle, resulting from a spontaneous perforation originating from an eviscerated loop. This perforation was visualised in the operating theatre and corrected with a single suture.
Intestinal perforation is a rare complication (1.5 %),1 even during colonoscopies,2 but it is a serious complication of Crohn’s disease. The most sensitive test for its diagnosis is computed tomography.3,4 As in our patient, it usually occurs in isolation and in patients with a stenosing–fistulising pattern. This complication is treated by means of surgery, usually emergency surgery. At the same time, medical treatment must be optimised by means of broad-spectrum antibiotic coverage and nutritional support.5
Please cite this article as: Casas Deza D, Gascón Ruiz M, García Fenoll R, García López S. Enfisema subcutáneo secundario a perforación intestinal en paciente con enfermedad de Crohn. Gastroenterol Hepatol. 2019;42:636–637.