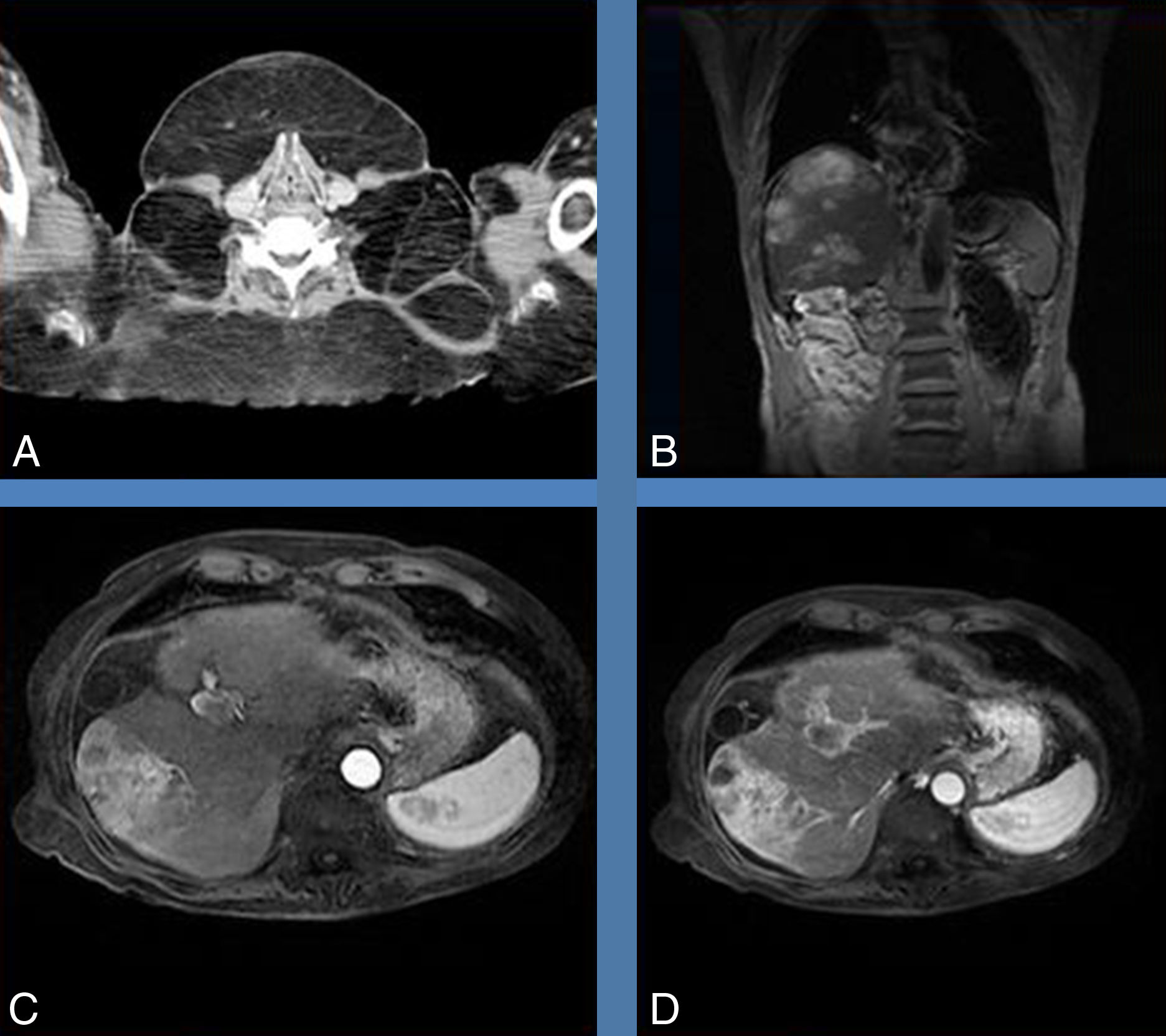
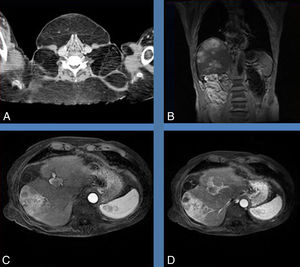
We present the case of a 67-year-old patient who came to our department with a two-year history of asthenia and anorexia, having not previously seen any other physician with these symptoms. A slight elevation of liver enzymes indicating cholestasis led us to suspect a liver disorder. Ultrasound showed space-occupying lesions, although without identifying their origin. As we suspected malignancy, we ordered an abdominal computed tomography (CT) scan. The CT was suggestive of hepatocarcinoma, but this required confirmation. Additional findings were tumour-related portal vein thrombosis with cavernous transformation, normal-sized spleen and collateral circulation with oesophageal varices. The liver had areas of impaired perfusion and discrete lobulation of segment I. Ascites made it unfeasible to take samples by biopsy, so a magnetic resonance imaging (MRI) scan was performed and identified the lesion as advanced LDH hepatocellular carcinoma (Fig. 1B–D). The patient had never been screened for hepatocellular carcinoma.
Other tests we carried out were serology for hepatotropic viruses, which were all negative; and blood analysis, showing elevation of GGT with normal ALT and AST, normal bilirubin and glucose, low albumin levels with normal total proteins, mild hyponatraemia, macrocytic anaemia without thrombocytopenia, decreased prothrombin activity and elevation of IgG and IgA.
The ascitic fluid was also analysed, finding a normal amount of polymorphonuclear cells and red blood cells. The albumin gradient was over 1.1g/dl and the protein concentration in the fluid was 2.6g/dl, compatible with ascites resulting from portal hypertension.
In view of the spread of the tumour and the patient's poor general condition, with his agreement, it was decided to provide palliative treatment at home.
On physical examination, multiple, hard, rounded subcutaneous lesions were noted on the neck and chest, as well as on the forearms, thighs and abdomen (Fig. 2A–D). The patient had started developing these lesions in his twenties and they had previously been asymptomatic. His alcohol consumption had been at excessive levels of approximately 60g a day since his youth. Although large in size, the lesions had not been causing any symptoms apart from restricting cervical flexion and extension movements. The patient had no family history of lipomatosis and had never required any medical care prior to this episode. The CT scan performed to study the liver lesion showed the fatty nature of these lesions (Fig. 1A). After reviewing the available literature, we attributed these abnormalities to type I Madelung's disease due to its characteristic distribution and morphology,1–6 and the diagnosis was supported by the patient's previous medical history.
Madelung's disease or benign symmetric lipomatosis or Launois-Bensaude syndrome, is a progressive disease with usual onset between the ages of twenty and forty, whose main manifestation is the growth of multiple benign non-encapsulated lipomas, typically on the neck, but also on the chest, abdomen, arms up to the elbow, thighs1 and, on occasion, on the tongue, in some cases causing macroglossia.7 The presence of multiple lipomas but with the distal parts of the extremities remaining unaffected is highly suggestive of Madelung's disease. It can be divided into two types: type I if the distribution is circumscribed; and type II when lipomatosis takes on the appearance of conventional obesity.1,2,5 The lipomas do not become malignant, with the main complication being limitation of mobility, especially of the neck. However, an increase in morbidity and mortality rates has been reported due to other causes, cardiac and cancer-related in particular, and the concept of benign disease is now under discussion. Other complications described are gynaecomastia, fatty liver disease, peripheral neuropathy and dyslipidaemia.1
The incidence is higher in males (15:1) and 90% of cases are related to alcohol abuse.1,2,8 Most of the cases reported are from countries in the Mediterranean area (mainly Spain, Italy and Greece).1 Madelung's disease is also associated with liver disorders,1,2,9 mainly steatosis, although here we have the important confounding factor of alcoholism, given that it is the main risk factor.5 Giving up alcohol is the only non-surgical treatment found to have any effect in reducing the size of the lesions; intra-lesional therapy with beta-blockers was no better than placebo.2 Lipomas should not be operated on unless they are causing compression or cervical mobility problems, because they will recur.2
The main genetic aetiopathogenic theory involves mitochondrial DNA, and there is a form with a maternal inheritance.1
Although the relationship between Madelung's disease and fatty liver disease is clearly described in the literature, there are no previous reports of associated hepatocarcinoma. Our case could therefore be the first example of such an association and, despite the alcohol being a confounding factor, it may have been a predisposing factor for the development of the patient's liver tumour.
Please cite this article as: Casas Deza D, Gotor Delso J, Bernal Monterde V. Síndrome de Madelung en un paciente con hepatocarcinoma avanzado. Gastroenterol Hepatol. 2018;41:645–647.