High-dose intravenous corticosteroids are commonly used in different medical specialist areas for the management of clinical exacerbations in autoimmune diseases. In recent years, they have been found to cause acute liver damage, although, paradoxically, they are the treatment of choice in liver diseases such as autoimmune or alcoholic hepatitis.
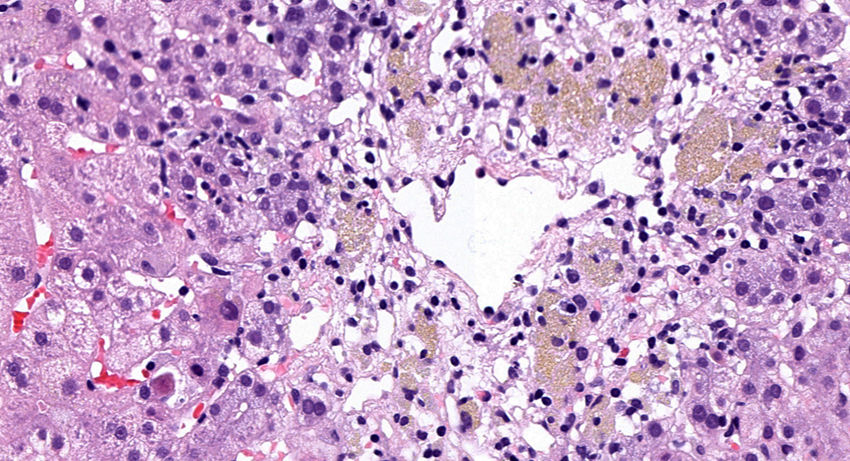
We present the case of a 55-year-old woman who was admitted to otolaryngology for sudden deafness with no apparent cause. She was started on empirical treatment with three doses of intratympanic corticosteroids and 500mg of IV methylprednisolone/24h for seven days (cumulative total dose of 3.5g), with subsequent oral descending deflazacort regimen. Seven weeks later, she developed pruritus and choluria, accompanied by liver function tests showing elevated liver enzymes (AST 205U/l, ALT 533U/l, alkaline phosphatase 102U/l, GGT 118U/l), which continued to increase progressively over the following weeks, with marked cytolysis (AST 858U/l and ALT 1468U/l), reaching a maximum bilirubin of 3.5mg/dl. The patient had no previous history of liver disease or alcohol consumption. Serology for hepatitis A, B, C and E viruses, herpes virus, varicella zoster, Epstein Barr and cytomegalovirus was all negative. The patient was only positive for antineutrophil cytoplasmic antibodies (ANCA P1/640), with the other autoantibodies (antinuclear, anti-native DNA, antimitochondrial, smooth muscle and anti-LKM antibodies) being negative. She also had normal immunoglobulin values and a normal electrophoretic profile. Abdominal ultrasound only showed cholelithiasis. Given the persistent elevation of transaminases, a therapeutic trial was conducted with 60mg of oral prednisone for suspected onset of seronegative autoimmune hepatitis, although this was subsequently ruled out by the liver biopsy result (Fig. 1). Finally, once viral and immunological causes had been ruled out and the temporal cause-effect relationship established with a score of six points on the CIOMS/RUCAM scale, the bolus treatment with methylprednisolone was identified as the origin of the hepatitis. Currently, seven months after onset of the symptoms, the patient's liver function test results have returned to normal.
Most drugs used in medicine can cause some degree of hepatotoxicity. “Drug-induced liver injury” (DILI) can be the result of predictable damage of intrinsic dose-dependent origin or an idiosyncratic reaction caused by host-dependent immunological hypersensitivity. In the idiosyncratic route, the drug or its metabolite causes activation of the adaptive immune response mediated by the recognition of damage-associated molecular patterns (DAMPs) which cause the release of proinflammatory cytokines, inducing a B/T-cell response against hepatocytes.1
The classic mechanisms of steroid treatment-induced liver damage are the viral reactivation of liver infections such as hepatitis B virus and the association with steatosis or steatohepatitis in long-term treatments.
In the case of acute methylprednisolone damage, the main hypothesis is that it is an idiosyncratic immune/allergic reaction caused by the interaction of the drug administered parenterally or of one of its excipients, such as sodium phosphate, causing necrosis or apoptosis of hepatocytes.2 This would explain why our patient's liver function did not get any worse when empirical treatment with prednisone was started orally.
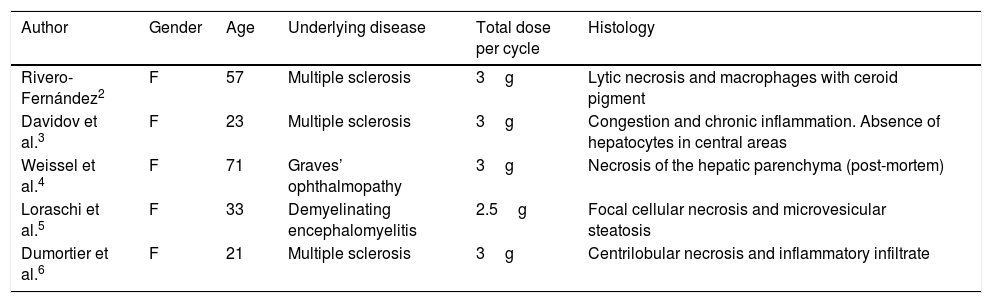
The clinical course can vary from asymptomatic hypertransaminasaemia,2,3 which is the most common, to fulminant hepatic failure.4 Its onset period can range from a few days to several weeks. The histological findings reported with this drug are wide-ranging, but data on hepatocyte necrosis and inflammation predominate (Table 1).
Histological findings secondary to methylprednisolone-induced hepatotoxicity.
| Author | Gender | Age | Underlying disease | Total dose per cycle | Histology |
|---|---|---|---|---|---|
| Rivero-Fernández2 | F | 57 | Multiple sclerosis | 3g | Lytic necrosis and macrophages with ceroid pigment |
| Davidov et al.3 | F | 23 | Multiple sclerosis | 3g | Congestion and chronic inflammation. Absence of hepatocytes in central areas |
| Weissel et al.4 | F | 71 | Graves’ ophthalmopathy | 3g | Necrosis of the hepatic parenchyma (post-mortem) |
| Loraschi et al.5 | F | 33 | Demyelinating encephalomyelitis | 2.5g | Focal cellular necrosis and microvesicular steatosis |
| Dumortier et al.6 | F | 21 | Multiple sclerosis | 3g | Centrilobular necrosis and inflammatory infiltrate |
F: female.
The differential diagnosis of DILI, after ruling out viral and metabolic causes, is autoimmune hepatitis. DILI can sometimes be complicated by the presence of autoantibodies, the most common being smooth muscle antibody in “autoimmune-like drug-induced liver injury”.7
The majority of published cases, like our patient, are in middle-aged women. This is probably due to the higher prevalence of autoimmune diseases in that subgroup.
In conclusion, intravenous corticosteroids are commonly used by specialists in areas such as neurology, endocrinology and ophthalmology, obtaining good clinical outcomes in the treatment of exacerbations of autoimmune diseases. However, there is poor general awareness of possible hepatotoxicity after high doses. Performing liver function tests during treatment with methylprednisolone may be beneficial for early recognition of this uncommon complication.
Please cite this article as: Monteserín L, Jiménez M, Linares P, Rodríguez-Martín L, Álvarez-Cuenllas B, Álvarez-Cañas C, et al. Hepatitis aguda secundaria a megadosis de metilprednisolona intravenosa. Gastroenterol Hepatol. 2018;41:508–509.