Hypoxic-ischaemic encephalopathy is one of the main causes of neurological damage in the new-born. Therapeutic hypothermia is the current treatment to reduce mortality and disability in new-borns with this condition.
ObjectiveTo identify nursing care in new-borns with severe to moderate EHI, treated with active therapeutic hypothermia.
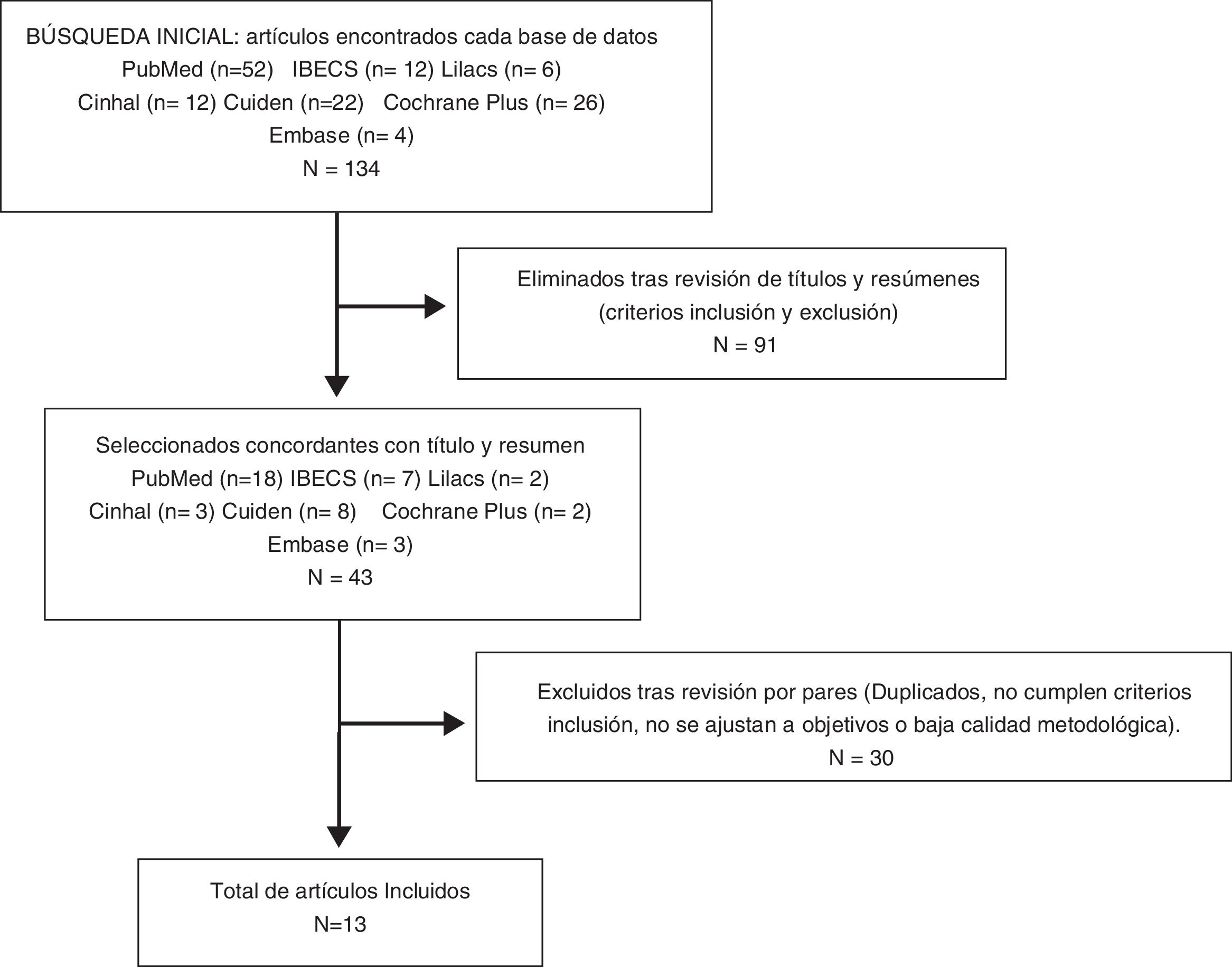
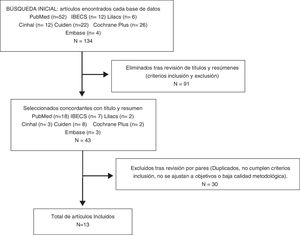
Materials and methodsA review of the scientific literature was carried out in different databases (PubMed, Lilacs, IBECS, Cinhal, OvidSP, Cuiden, Embase and Cochrane Plus) over the last five years. The documentary assessment was carried out by peers and the quality was evaluated using the CEBM and GRADE scales.
ResultsOf the 22 articles selected and reviewed, it is evident that therapeutic hypothermia is effective in reducing the mobility and mortality of neo-nates with hypoxic-ischaemic encephalopathy. Nursing care during hypothermia treatment focuses on four basic pillars: general care for stabilisation of the new-born, preparation of the material, administration of medical treatment in all its phases and emotional support of the family.
ConclusionsTherapeutic hypothermia is effective in reducing the sequelae and mortality of neonates with hypoxic-ischaemic encephalopathy. Nursing care is essential throughout the treatment, in the early detection of complications in the infant and psychological support for parents. It is essential for nurses to receive training in this care.
La Encefalopatia Hipóxico-Isquémica es una de las principales causas de daño neurológico en el neonato. Actualmente, la hipotermia terapéutica es el tratamiento de elección para reducir la mortalidad y la discapacidad en los niños que presentan esta patología.
ObjetivoIdentificar los cuidados enfermeros en RN con EHI moderada severa tratados con Hipotermia terapéutica activa.
Materiales y MétodosSe realizó una revisión de la literatura científica en diferentes bases de datos (PubMed, Lilacs, IBECS, Cinhal, OvidSP, Cuiden, Embase y Cochrane Plus) durante los últimos cinco años. La valoración documental se realizó por pares y la calidad se evaluó mediante las escalas CEBM y GRADE.
ResultadosDe los 22 artículos seleccionados y revisados se evidencia que la hipotermia terapéutica es efectiva al reducir la morbimortalidad de los neonatos con Encefalopatia Hipóxico-Isquémica. Los cuidados enfermeros durante el tratamiento de hipotermia se centran en cuatro pilares básicos: los cuidados generales para la estabilización del recién nacido, la preparación del material, la administración del tratamiento médico en todas sus fases y el soporte emocional de la familia.
ConclusionesLa hipotermia terapéutica es efectiva al reducir las secuelas y la mortalidad de los neonatos con Encefalopatia Hipóxico-Isquémica. Los cuidados enfermeros son esenciales y están presentes durante todo el tratamiento, detectan precozmente complicaciones en los niños y ofrecen apoyo psicológico a los padres. La formación del personal de enfermería en estos cuidados es fundamental.
According to the Spanish Society of Neonatology (SSN) a neonate is the term given to all newborns at a gestational age (GA) of 37 weeks or more, and premature to all newborns whose gestational age is under 37 weeks. In turn, preterm newborns may be classified into moderate-late (born at 32–36 weeks GA), highly preterm (born between 28 and 31 weeks GA) and extremely preterm (born at 27 weeks GA or under).1
The most prevalent pathologies in the neonate are due to respiratory causes, neurological causes, sepsis and congenital malformations. In the preterm neonate they are derived from their lack of maturity, mainly due to the shortening of the gestational period and to hypoxia at birth.1
Hypoxic-ischaemic encephalopathy (HIE) is a clinical syndrome of neurological dysfunction caused by secondary cerebral hypoxia and different adaptative processes of the newborn after birth. Firstly, a cerebral lesion occurs during a complex process: the primary phase of the lesion, caused by asphyxial damage and impairment of the oxidative metabolism. After cerebral reperfusion partial recovery occurs, called the latency phase, also known as the therapeutic window, which is the interval prior to the secondary damage phase. In the secondary damage phase biochemical, molecular and cellular changes occur in cascades, leading to brain damage. This phase begins between 6 and 15 h after the asphyxia damage and may be prolonged for several days. During the therapeutic window phase therapeutic intervention may be undertaken to reduce brain injuries, with this period being ideal for treatment initiation.2–4
The neurological examination of the neonate establishes the presence or absence of acute encephalopathy. A series of grading levels have been designed to classify the HIE into different stages (mild, moderate and severe). Mild HIE carries no risk of mortality nor moderate or severe ulterior disability, although between 6% and 24% present with slight delays in psychomotor development. In moderate HIE there is a change in awareness during the first 6 h of life, associated with a perinatal background of hypoxic-ischaemic aggression markers and the neonates present with a risk of death of approximately 10%, whilst 30%–40% of the survivors will present with disability. The neonate with severe HIE is stuporous or in a coma, intensely hypotonic and may present with subtle convulsions and multifocal seizures. Between 24 and 72 h of life, impairment of the ability to wake up appears to worsen, with a frequent appearance of encephalic stem dysfunction and some newborns present with signs of intracranial hypertension. The risk of death in neonates with severe HIE is approximately 60%, and the great majority of survivors will have permanent sequelae and disabilities.3,5 Several studies suggest that 20% of the neonates who survive with severe HIE will have cerebral paralysis.1–3 This impact on the child’s health and the family, social and even legal implications in terms of their disability, convert this pathology into a major sociosanitary problem.6
The rate of HIE is uneven in the world. The highest rates are found in countries with poor resources. In these countries, the World Health Organisation calculates that up to 25% of newborns, (WHO), 8% of all deaths below,5 years of age are related to perinatal asphyxia. Several authors indicate that the distribution of this pathology not only differs between countries, but also between regions of the same country.3,7
In Spain, a study conducted in 90 neonatal units showed there to be a rate of .77/1000 live newborns of 35 weeks GA affected by moderate-severe HIE, with no difference observed between communities. Of these, 18% died during the neonatal period and 36%during their first year of life.5
During the 20th century no specific therapeutic approach was available for this pathology. Its treatment was limited to the provision of general supportive medical care and to treat its complications, such as seizure crises.3 In 2006 the Americana Academy of Paediatrics considered this disease as “one of the unresolved medical frustrations in contemporary neonatal medicine”.8 Fortunately, from then onwards several authors have demonstrated that therapeutic hypothermia is an effective intervention to reduce mortality, morbidity and disability in the babies who survive this condition.2–7,9,10 Disability is understood to be all the consequences derived from severe changes in the neurodevelopment of the newborn after hospital discharge, such as cerebral paralysis and its associated problems (cognitive deficit, behavioural problems, oral-motor and visual changes, memory disorders, seizures, etc.).6
Within the modalities of therapeutic hypothermia we found 2 types mainly: passive and active. The passive or non induced hypothermia is understood to be cooling down on non application of active warming, such as not switching on the thermal cot heater or not covering the newborn up, maintaining the temperature between 33 and 34 °C. Its main use is in the birth hospital and during the transport of the newborn with HIE to a centre of reference to prevent delay in treatment initiation with active hypothermia.11
Induced or active hypothermia consists in deliberately lowering the central temperature of neonates between 3 and 4 °C using cooling equipment. Three phases may be distinguished here: cooling down, maintenance and warming up. The cooling down phase consists in producing moderate cooling down to the desired temperature of 33−34 °C. This phase has to be started prior to 6 h of life, with experimental studies demonstrating that this period represent the therapeutic window for starting HIE treatment. Once the temperature of 33−34 °C has been reached, for the next 72 h, the maintenance phase is undertaken with a strict body temperature control for the newborn. After this, in the warming up phase, gradual and progressive warming up would start, at a rhythm under. 5 °C per hour, to reduce the appearance of complications, such as seizures.
Also, during the whole management of the neonate with HIE, hyperthermia must be avoided, as this would lead to a worsening of neurotoxic damage.2,4 It has been demonstrated that therapeutic hypothermia is effective for reducing neurological impairment, particularly in neonates with moderate HIE.4 In studies conducted using cooling equipment, sustained moderate hypothermia is achieved in 2 ways: through total body cooling or through selective cooling of the head. Both methods have obtained favourable outcomes.2,3
In Spain, this therapy has been used since the year 2008. Its implementation had been progressive in up to 60% in tertiary centres of all communities by 2015.5 Improvements in neonate morbimortality have been obtained with this therapy with HIE, since it reduces cerebral metabolism and neuronal excitability. It also reduces the synthesis and release of free radicals and nitric oxide, reduces lipid peroxidation, the freedom of excitotoxic amino acids (glutamate), and reduces the activity of apoptosis and preserves endogenous antioxidants.2 Great progress has been made in Spain for the introduction of this treatment. After analysing and assessing 90 level 3 neonatal units in Spain, Arnáez et al.5 concluded that 90% of newborns with moderate or severe HIE who were candidates for the treatment received it.
Notwithstanding, this treatment is not risk-free. It may lead to serious complications such as: changes in coagulation, increased risk of thrombosis due to the slowing down of blood flow and reduction of cardiac output and heart rate, with sinus bradycardia being the most common arrhythmia. There is also a tendency towards hyperglycaemia, a reduction of metabolism and on a renal level, oliguria and anuria may appear, as hypothermia promotes tissue fluid retention.12 Despite this, treatment with hypothermia is an effective intervention to reduce mortality and disability of survivors, providing higher benefits than complications.3–6
In a meta-analysis which included 13 clinical trials and a total sample of 1806 neonates, the benefits and adverse effects of this treatment were described. As adverse effects, it was found that the application of therapy with hypothermia increased the risk of thrombocytopenia and cardiac arrhythmia, with a high risk of coagulation and intracranial bleeding during its application. Benefits described were its protective efficacy, proven by the reduction of mortality and as adverse events, the risk of systemic infection, hypoglycaemia and acute kidney damage. Also, during the follow-up of the neonates at 12 and 24 months of life, moderate hypothermia had improved survival rates.13
At the same time, the results of a clinical trial conducted in the United States with a sample of 364 neonates (≥ 36 weeks GA) with HIE from 18 centres supported the current application of cooling for the first 72 h at 33.5 °C since it was confirmed that, with this treatment, death and disability at 18 months of age was lower.14
Regarding care of children with therapeutic hypothermia, several authors state that the nurses play an essential role in the treatment of children with moderate-severe HIE. They highlight that nurses should provide basic care both to the newborns and their family, whatever the final prognosis is.6,15,16 It is notable in those cases where the neonate does not overcome this disorder, they must be provided with care to prevent physical suffering, offering psychological and human support to the family and if applicable, continue providing it with the child to allow for a dignified death.17
It should finally be emphasized that newborns treated with induced hypothermia, due to their critical status, need to be admitted into neonatal intensive care units (NICU), where there is great complexity of new technologies and their prolonged treatment requires highly specialised nursing care. Due to all of the above, we proposed the undertaking of a bibliographic review aimed at identifying nursing care in newborns with moderate-severe HIE treated with active therapeutic hypothermia.
Materials and methodsDesignA review of the scientific literature was undertaken using a bibliographic search in national and international databases for the month of January and February 2017. The search started with a research question in PICO18 format (Patients: neonates with HIE; Intervention: treatment with hypothermia; Comparison: not present: Outcomes: nursing care). The electronic databases consulted were: PubMed, Lilacs, IBECS, Cinhal, OvidSP, Cuiden Plus, Embase and Cochrane Plus. For the search the following descriptors were used: Medical Subject Headings (MeSH) and Health Sciences descriptors (DeCS). The MeSH used were: “newborn”, “hypothermia induced”, “nursing care”, “premature”, “nurse’s role”, “hypoxia-ischemia, brain”; and the DeCs: “cuidado”, “hipotermia inducida”, “neonate”, “encefalopatía”, “hipotermia” and “hypoxia-isquemia encefálica”. The Boolean operators used were “AND” and “OR”.
Selection criteriaThe inclusion criteria established were: studies conducted in neonates with moderate or severe HIE, treated with induced hypothermia; documents published in Spanish, English, or Portuguese during the years 2011–2016; qualitative, quantitative sties, bibliographic and systematic reviews, protocols and clinical guidelines. Several articles from previous years were included too, due to their relevance. We also undertook a manual search of works which were not published, such as internal protocols of different Spanish hospitals, so as to avoid publication weighting. These were directly acquired from the centres themselves.
All documents and studies based on paediatric patients and adults with different pathologies, mild HIE and low quality scientific-technical documents were excluded.
Data extractionThe extraction of data was performed in several phases. First a documental assessment phase took place searching to minimise biases and offer greater reliability of results. Each article was reviewed by 2 of the study authors with a selection of those which coincided by titles and abstract. After this, the articles were assessed according to the review purpose and inclusion criteria. Duplicates were eliminated. After this, methodological assessment took place using critical reading of the documents. To so this, several scales were used, depending on study type: Strengthening the Reporting of Observational studies in Epidemiology (STROBE)19 for the observational studies, Critical Appraisal Skills Programme Spain (CASPe)20 for narrative reviews and the AGREE II tool for evaluation and clinical practice guidelines. Finally, levels of evidence and degrees of recommendation of all selected documents were assessed, using the recommendations of the GRADE17,21 scale and the Centre for Evidence-Based Medicine (CEBM) de Oxford.22
Ethical considerationsData obtained were treated in accordance with the general data protection ruling of the European Union 2016/679 of the European Parliament, applicable in Spain on 25th May 2018, and Law 41/2002, of 14th November, the basic regulator of patient autonomy, or rights and obligations in matters of information and clinical documentation.
ResultsDuring the initial search, a total of 134 documents were found. After applying the corresponding filters, ruling out duplicates and those which did not meet with the corresponding selection criteria, and reading the title and abstract, a total of 43 articles were selected. Finally, with filtering, after critical reading of the articles, 30 were removed, selecting a total of 13 articles for undertaking this review (Fig. 1).
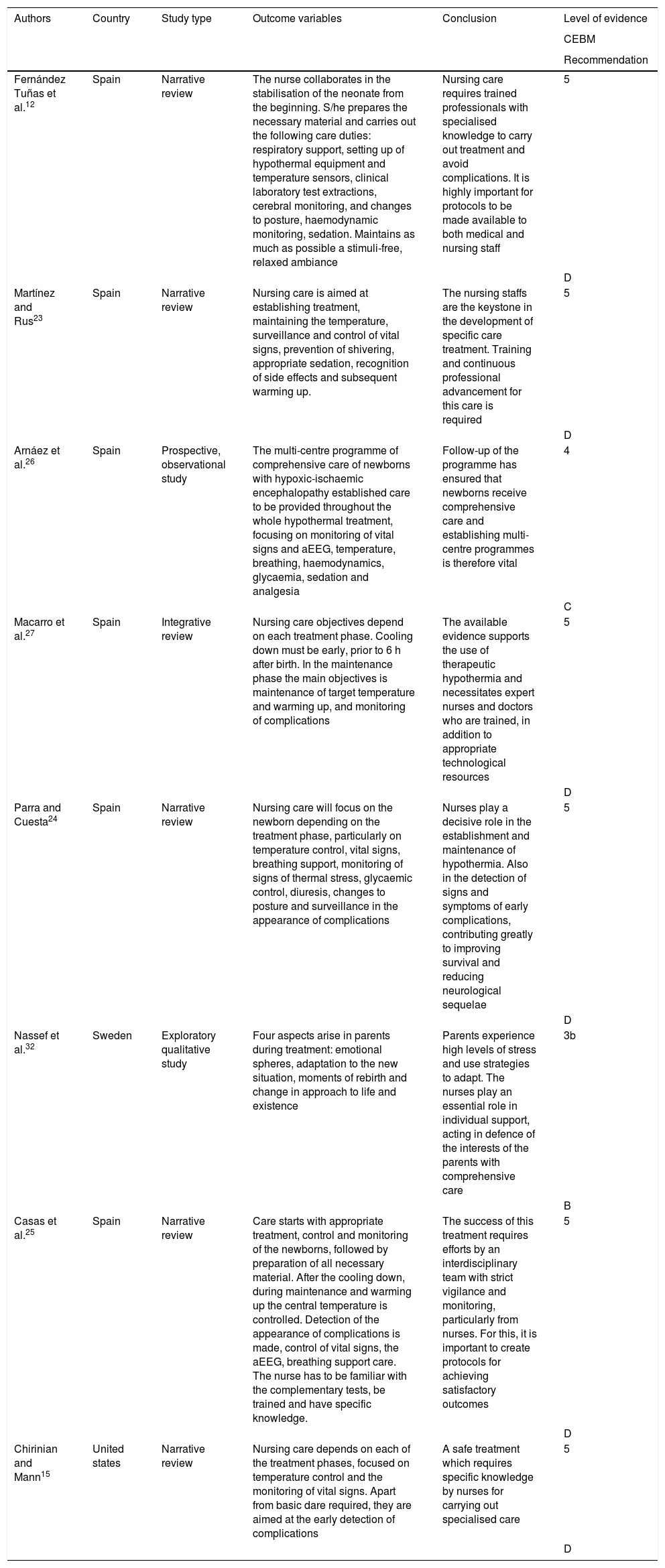
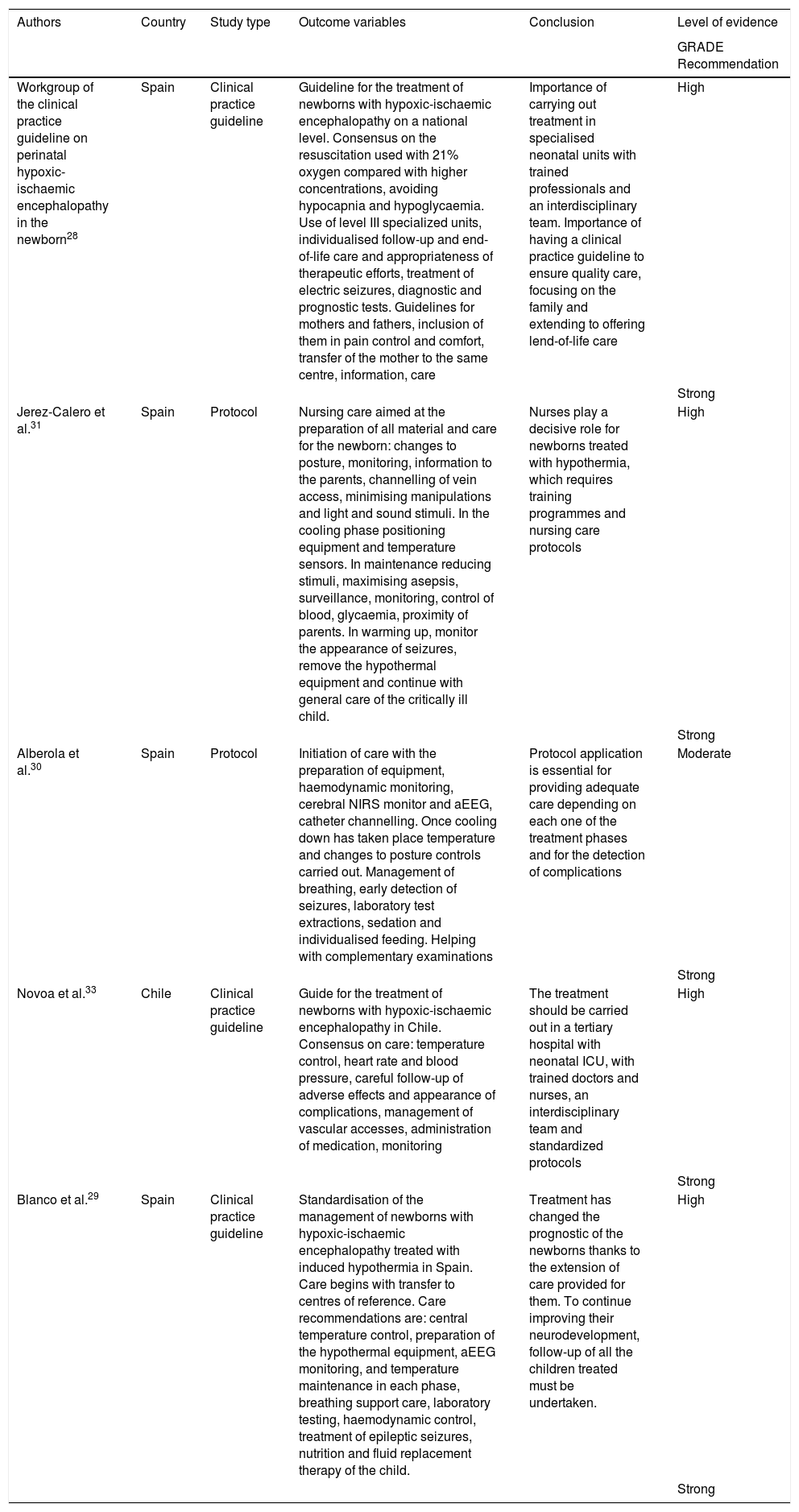
Table 1 contains the results obtained, based on nursing care applied in neonates during treatment of induced hypothermia and Table 2 the care included in protocols and clinical practice guidelines. Out of the total studies included in this review, 10 are studies conducted in Spain. Specifically, 4 narrative reviews were found,12,23–25 one prospective, observational study,26 one integrative review,27 2 clinical practice guides,28,29 and 2 protocols.30,31 Outside our country only one exploratory qualitative study was found, conducted in Sweden32 and the clinical practice guide developed in Chile.33
Table of analysis and summary. Nursing care studies.
| Authors | Country | Study type | Outcome variables | Conclusion | Level of evidence |
|---|---|---|---|---|---|
| CEBM | |||||
| Recommendation | |||||
| Fernández Tuñas et al.12 | Spain | Narrative review | The nurse collaborates in the stabilisation of the neonate from the beginning. S/he prepares the necessary material and carries out the following care duties: respiratory support, setting up of hypothermal equipment and temperature sensors, clinical laboratory test extractions, cerebral monitoring, and changes to posture, haemodynamic monitoring, sedation. Maintains as much as possible a stimuli-free, relaxed ambiance | Nursing care requires trained professionals with specialised knowledge to carry out treatment and avoid complications. It is highly important for protocols to be made available to both medical and nursing staff | 5 |
| D | |||||
| Martínez and Rus23 | Spain | Narrative review | Nursing care is aimed at establishing treatment, maintaining the temperature, surveillance and control of vital signs, prevention of shivering, appropriate sedation, recognition of side effects and subsequent warming up. | The nursing staffs are the keystone in the development of specific care treatment. Training and continuous professional advancement for this care is required | 5 |
| D | |||||
| Arnáez et al.26 | Spain | Prospective, observational study | The multi-centre programme of comprehensive care of newborns with hypoxic-ischaemic encephalopathy established care to be provided throughout the whole hypothermal treatment, focusing on monitoring of vital signs and aEEG, temperature, breathing, haemodynamics, glycaemia, sedation and analgesia | Follow-up of the programme has ensured that newborns receive comprehensive care and establishing multi-centre programmes is therefore vital | 4 |
| C | |||||
| Macarro et al.27 | Spain | Integrative review | Nursing care objectives depend on each treatment phase. Cooling down must be early, prior to 6 h after birth. In the maintenance phase the main objectives is maintenance of target temperature and warming up, and monitoring of complications | The available evidence supports the use of therapeutic hypothermia and necessitates expert nurses and doctors who are trained, in addition to appropriate technological resources | 5 |
| D | |||||
| Parra and Cuesta24 | Spain | Narrative review | Nursing care will focus on the newborn depending on the treatment phase, particularly on temperature control, vital signs, breathing support, monitoring of signs of thermal stress, glycaemic control, diuresis, changes to posture and surveillance in the appearance of complications | Nurses play a decisive role in the establishment and maintenance of hypothermia. Also in the detection of signs and symptoms of early complications, contributing greatly to improving survival and reducing neurological sequelae | 5 |
| D | |||||
| Nassef et al.32 | Sweden | Exploratory qualitative study | Four aspects arise in parents during treatment: emotional spheres, adaptation to the new situation, moments of rebirth and change in approach to life and existence | Parents experience high levels of stress and use strategies to adapt. The nurses play an essential role in individual support, acting in defence of the interests of the parents with comprehensive care | 3b |
| B | |||||
| Casas et al.25 | Spain | Narrative review | Care starts with appropriate treatment, control and monitoring of the newborns, followed by preparation of all necessary material. After the cooling down, during maintenance and warming up the central temperature is controlled. Detection of the appearance of complications is made, control of vital signs, the aEEG, breathing support care. The nurse has to be familiar with the complementary tests, be trained and have specific knowledge. | The success of this treatment requires efforts by an interdisciplinary team with strict vigilance and monitoring, particularly from nurses. For this, it is important to create protocols for achieving satisfactory outcomes | 5 |
| D | |||||
| Chirinian and Mann15 | United states | Narrative review | Nursing care depends on each of the treatment phases, focused on temperature control and the monitoring of vital signs. Apart from basic dare required, they are aimed at the early detection of complications | A safe treatment which requires specific knowledge by nurses for carrying out specialised care | 5 |
| D |
aEEG: the amplitude integrated electroencephalography; CEBM: Centre for Evidence-Based Medicine, Oxford.
Analysis and summary. Nursing care protocols and guidelines.
| Authors | Country | Study type | Outcome variables | Conclusion | Level of evidence |
|---|---|---|---|---|---|
| GRADE Recommendation | |||||
| Workgroup of the clinical practice guideline on perinatal hypoxic-ischaemic encephalopathy in the newborn28 | Spain | Clinical practice guideline | Guideline for the treatment of newborns with hypoxic-ischaemic encephalopathy on a national level. Consensus on the resuscitation used with 21% oxygen compared with higher concentrations, avoiding hypocapnia and hypoglycaemia. Use of level III specialized units, individualised follow-up and end-of-life care and appropriateness of therapeutic efforts, treatment of electric seizures, diagnostic and prognostic tests. Guidelines for mothers and fathers, inclusion of them in pain control and comfort, transfer of the mother to the same centre, information, care | Importance of carrying out treatment in specialised neonatal units with trained professionals and an interdisciplinary team. Importance of having a clinical practice guideline to ensure quality care, focusing on the family and extending to offering lend-of-life care | High |
| Strong | |||||
| Jerez-Calero et al.31 | Spain | Protocol | Nursing care aimed at the preparation of all material and care for the newborn: changes to posture, monitoring, information to the parents, channelling of vein access, minimising manipulations and light and sound stimuli. In the cooling phase positioning equipment and temperature sensors. In maintenance reducing stimuli, maximising asepsis, surveillance, monitoring, control of blood, glycaemia, proximity of parents. In warming up, monitor the appearance of seizures, remove the hypothermal equipment and continue with general care of the critically ill child. | Nurses play a decisive role for newborns treated with hypothermia, which requires training programmes and nursing care protocols | High |
| Strong | |||||
| Alberola et al.30 | Spain | Protocol | Initiation of care with the preparation of equipment, haemodynamic monitoring, cerebral NIRS monitor and aEEG, catheter channelling. Once cooling down has taken place temperature and changes to posture controls carried out. Management of breathing, early detection of seizures, laboratory test extractions, sedation and individualised feeding. Helping with complementary examinations | Protocol application is essential for providing adequate care depending on each one of the treatment phases and for the detection of complications | Moderate |
| Strong | |||||
| Novoa et al.33 | Chile | Clinical practice guideline | Guide for the treatment of newborns with hypoxic-ischaemic encephalopathy in Chile. Consensus on care: temperature control, heart rate and blood pressure, careful follow-up of adverse effects and appearance of complications, management of vascular accesses, administration of medication, monitoring | The treatment should be carried out in a tertiary hospital with neonatal ICU, with trained doctors and nurses, an interdisciplinary team and standardized protocols | High |
| Strong | |||||
| Blanco et al.29 | Spain | Clinical practice guideline | Standardisation of the management of newborns with hypoxic-ischaemic encephalopathy treated with induced hypothermia in Spain. Care begins with transfer to centres of reference. Care recommendations are: central temperature control, preparation of the hypothermal equipment, aEEG monitoring, and temperature maintenance in each phase, breathing support care, laboratory testing, haemodynamic control, treatment of epileptic seizures, nutrition and fluid replacement therapy of the child. | Treatment has changed the prognostic of the newborns thanks to the extension of care provided for them. To continue improving their neurodevelopment, follow-up of all the children treated must be undertaken. | High |
| Strong |
aEEG: the amplitude integrated electroencephalography; GRADE: Grading of Recommendations, Assessment, Development and Evaluation; NIRS: monitor near infrared spectroscopy cerebral.
Regarding the methodological quality of the 13 studies reviewed, it was observed that there was a higher level of evidence and degree of recommendation in the 3 clinical practice guidelines28,29,33 and in the 2 protocols included.30,31
The results obtained show that nursing care, during hypothermia treatment may be classified into 3 major blocks:
- -
General care for the stabilisation of the newborn.
- -
Preparation of the material and administration of medical guidelines.
- -
Emotional support to the family.
In most studies reviewed,12,15,23–27,29–31,33 nursing care is described, depending on each of the treatment phases, mainly focusing on temperature control and the monitoring of vital signs.
A narrative review, undertaken by Fernández Tuñas et al.,12 described the care shown by nurses during treatment. These professionals help to stabilise the neonate during the whole process, provided respiratory support care, cerebral monitoring and the surveillance of haemodynamic stabilisation.
According to Macarro et al.,27 the main aim of nursing care is the maintenance of the target temperature during the maintenance phase and the monitoring of complications in the warming up phase. Casas et al.25 underline that the success of this treatments requires an effort from the whole interdisciplinary tam, with strict monitoring and vigilance, particularly from the nurses.
In 2 of the studies conducted in Spain12,31 it is notable that the nursing intervention also has to aim at providing a relaxed and stimulus-free environment. Jerez-Calero et al.31 recommend reducing manipulations and minimising ambient light and sound stimuli.
Preparation of the material and administration of medical treatmentSeveral studies indicate that the nurses are in charge of the preparation of all the necessary material for treatment initiation (hypothermia equipment and monitors for haemodynamic and neurological surveillance).12,25,29–31 Alberola et al.30 highlight the need to prepare the haemodynamic monitoring equipment, the amplitude integrated electroencephalography (aEEG), the near infrared spectroscopy cerebral monitor (NIRS) and all the necessary material for channelling catheters.
Regarding the administration of medical treatment, several studies highlight the importance of preparation and control of sedation during the whole process,12,29,30 especially those specific to glycaemic control.24,26,28,31 The Spanish guide for the treatment of newborns with HIE28 advises the avoidance of hypocapnia and hypoglycaemia.
Alberola et al.30 indicate that the extraction of samples for the laboratory, sedation, individualised feeding and collaboration in complementary examinations form part of the nursing care during hypothermia treatment.
Emotional support to the familyA qualitative study conducted in Sweden by Nassef et al.32 to the parents of neonates with hypothermia treatment describes the emotional aspects and times of stress they suffer from due to the condition of their children. The authors concluded that the nurses play an essential role providing individual support to the parents.
In Spain, Jerez et al.31 and the clinical practice guide edited by the Minister of Health, Social Services and Equality and the Agència de Qualitat i Avaluació Sanitàries de Catalunya (AQuAS)28 all stress the importance of the nurses encouraging the parents to get close to their children. Specifically, this document contains an appendix with a guide for mothers and fathers, with recommendations for family and newborn care. The parents are included in providing comforting care for their child, with better contact through the mother moving to the same centre and stressing the importance of appropriate therapeutic support, if the situation requires it.
DiscussionThe results of this review show that nursing care during the treatment of hypothermia focuses on 3 basic pillars: general care for the stabilisation of the newborn, preparation of all necessary material and the administration of medical guidelines throughout the process (drugs, extraction of samples, fluid therapy, etc.), and emotional support to the family.
General care for the stabilisation of the newbornMost studies coincide in that care of the newborn, during treatment of hypothermia, will be focused on their stabilisation. These are mostly based on: temperature control and the monitoring of vital signs,12,23–27,29–31,33 cerebral monitoring and sedation-analgesia management,12,26,30 control of diuresis24 and changes to posture.12,24 Two studies underline that nursing intervention should also be aimed at providing a relaxed and stimuli-free ambiance.12,31 Most authors coincide that surveillance throughout treatment must be maintained to detect any complications in good time.15,23–25,27–31,33 The most prevalent are: changes in coagulation, risk of thrombosis, sinus bradycardia, hyperglycaemia, reduction of metabolism and oliguria and anuria, as hypothermia promotes tissue fluid retention.12
When caring for the preterm or ill newborn there is the added risk of their particular complexity, their low weight and their vulnerability. They have fewer physiological resources to shore up against damage or complications from the pathologies they are suffering from and from their treatments. The need for a greater number of invasive procedures and the administration of certain drugs increases the risk of complications.1 As a result, these patients with HIE require strict monitoring during the treatment phases. Control and monitoring of the newborn must be practised by the interdisciplinary team, and especially the nurse who is continuously present, as indicated by several authors.15,24,25,31
Preparation of the material and administration of medical guidelinesPractically all studies concur that it is nurses who are responsible for the preparation of everything that is required for treatment, i.e. the material for respiratory support, channelling of veins and arteries, hypothermia equipment, temperature sensors, etc.12,23,25,29–31
In addition to the administration of drugs and fluid replacement therapy, several authors also highlight glycaemic control and clinical laboratory tests extraction required throughout the process as part of care.12,24,26,28,30,31
Several authors state that the nursing interventions and activities are essential in the treatment of hypothermia.15,16,31 The preparation and administration of drugs and the application of some procedures require professionals of a high level of specific knowledge and experience.1 As a result, with the incorporation of these professionals to the interdisciplinary team, effective treatment is guaranteed and complications are avoided.12,23,24,27
Emotional support to the familyThe study conducted in Sweden confirmed the effectiveness of nurses in offering support to the parents of newborns, with hypothermia treatment, who were suffering from high levels of stress.32
Along these same lines, in Spain, 2 studies reported the importance of the nurses in encouraging parents to approach their children, including them in treatment, offering them information and emotional support throughout the process.28,31 In the care of newborns, recommendations from Care Centred on the Development and family (CCD) were followed. These are based on the philosophy that encompasses the concepts of dynamic interaction between the newborn, the family and the environment. They are applied during the neonatal period, in an attempt to optimise both the macro ambiences (noises, lights…) and the micro ambiance (posture, manipulations, pain….) in which the child develops. The family is involved to enhance their role as the main carer of the neonate in an active and continuous manner. The family and the newborn is recognized as a unit and should therefore form part of the nursing care and competences.1,34,35
Although it was not the aim of this study, in most articles the need for nurses to receive specialised and specific training is highlighted. The authors emphasize the need to work with protocols and guidelines to improve the care offered to neonates treated with hypothermia.12,15,23,25–27,30,31,33
LimitationsLow levels of evidence and recommendations from the majority of studies on nursing care are notable. Although this is a major limitation it also creates an opportunity to open new lines of investigation to demonstrate the effectiveness of care and the benefits it has on the newborn and their family. To do this, research studies in care with high levels of evidence and recommendation are required to ensure quality nursing care.
ConclusionsNursing care is essential in therapeutic hypothermia treatment. These professionals offer comprehensive care that embraces both the newborn and their family. The aim of neonate care is haemodynamic stabilisation throughout the process, the preparation of necessary material and the administration of treatments and clinical guidelines. To do this, the training and specialisation of these professionals, together with the creation of protocols and clinical guidelines, are essential for carrying out hypothermia treatment with the maximum possible efficaciousness and safety.
FinancingThis research did not receive any type of financing.
Conflict of interestsThe authors have no conflict of interests to declare.
Please cite this article as: Solaz-García ÁJ, Sáenz-González P, Borrás Vañó MJ, Montejano-Lozoya R. Cuidados enfermeros a neonatos con encefalopatía hipóxico-isquémica en hipotermia terapéutica. Revisión bibliográfica. Enferm Intensiva. 2021;32:88–99.