To identify the importance of the needs of family members of patients in an intensive care unit (ICU).
MethodDescriptive, comparative and cross-sectional study based on a secondary data analysis of 251 relatives of ICU patients at a university hospital in Santiago, Chile. Using non-random sampling, the ‘Critical Care Family Needs Inventory’ was used to establish the family needs, as well as a sociodemographic questionnaire that included: age, gender, educational level, patient relationship and previous ICU experience. A descriptive statistical analysis, Student's t-test and ANOVA were performed.
ResultsThe most important family needs related to the dimensions of ‘security’ (mean=3.90) and ‘information’ (mean=3.76), while those of minor importance with ‘support’ (mean=3.09). In the latter, differences were observed at an older age (p<0.05), an educational level (p<0.001) and relationship with the patient (p<0.05).
ConclusionsThe most relevant needs for family members in the ICU are related to safety and information. Less important needs are influenced by certain sociodemographic variables. Identifying the degree of importance of family needs will allow the health team to improve its relationship with families in ICUs.
Identificar el grado de importancia de las necesidades de los familiares de pacientes en una unidad de cuidados intensivos (UCI).
MétodoEstudio descriptivo, comparativo y transversal realizado a partir de un análisis secundario de datos de 251 familiares de pacientes de una UCI en un hospital universitario en Santiago, Chile. Utilizando un muestreo no aleatorio se aplicó el instrumento Critical Care Family Needs Inventory para conocer las necesidades familiares, además de un cuestionario sociodemográfico que incluyó: edad, género, nivel educacional, relación con el paciente y experiencia previa en UCI. Se realizó análisis estadístico descriptivo, prueba t de Student y ANOVA.
ResultadosLas necesidades familiares más importantes se relacionaron con las dimensiones de «seguridad» (X¯=3,90) e «información» (X¯=3,76), mientras que las de menor importancia se relacionaron con la de «apoyo» (X¯=3,09). En esta última, se observaron diferencias a mayor edad (p < 0,05), nivel educacional (p < 0,001) y relación con el paciente (p < 0,05).
ConclusionesLas necesidades más relevantes para los familiares en la UCI se relacionan con la seguridad e información. Las necesidades de menor importancia están influidas por ciertas variables sociodemográficas. La identificación del grado de importancia de las necesidades familiares permitirá al equipo de salud mejorar su relación con las familias en las UCI.
The admission of a loved one to an intensive care unit is a stressful event for the patient as well as their family. In this context, family members experience specific needs which, if they are identified and satisfied, may reduce the psychological burden of this experience.
This study is the first report on critical patient family needs in a Spanish-speaking country in Latin America. Its results confirm the importance of aspects connected with information delivery, regardless of the cultural and sociodemographic context of the family members studied. It also sets a challenge for nurses who work in intensive care units, as they should establish effective communication with the family members of critical patients in a context in which there is a high demand for care.
Implications of the studyThis study has made it possible to identify the most important needs of family members of the patients in an intensive care unit in a teaching hospital. In terms of care, the needs of family members must be detected using validated questionnaires on their opinions and those of the healthcare team. This way the resulting knowledge is made available for use by critical healthcare managers and administrators, so that they can develop and apply quality indicators associated with satisfying the needs of family members. In this way the needs of critical patients’ families will become an area of research that should continue to be developed, by studying interventions that improve communication with the care team, regular assessments of their degree of satisfaction or awareness of the degree to which health institutions are prepared to consider this subject as a priority.
Within hospitals, intensive care units intensive care units (ICU) are characterised by their high level of complexity, due to the severity of their patients and the supporting therapies they use. The complexity of care here therefore arises not solely in terms of care for the patient, as it is affected by the impact on the family of a loved one being admitted to an ICU.
In general, hospitalisation in an ICU is associated with high levels of anxiety, stress and depression in family members. This may even last for 3 months after the discharge of the patient.1 The family members of ICU patients at a high risk of dying have been observed to suffer a high prevalence of feelings of fear, anxiety, depression and sadness.2 Likewise, in a longitudinal study it was found that after one year up to 43% of the family members of patients who had been in an ICU presented high levels of depressive symptoms. In the majority of cases these tend to fall over time, while in 16% of family members they remained high.3 Similarly, the prevalence of post-traumatic stress in the family members of ICU patients stands at from 13% to 56%, and it is higher in the family members of adult patients,4 while in Chile it reaches 23% in some studies.5
This is a complex scenario in which critical patients’ families experience a range of needs, of which the most important are associated with information and security. Most particularly, receiving honest answers from the care team, knowing the prognosis of the patient and feeling that staff are concerned about the patient have been said to be the most important. On the contrary, needs connected with supports and comfort, most especially spiritual support, are reported to be relatively less important.6 The first reports date from 1976, when the North American nurse Nancy Molter investigated the characteristics of these needs and their importance for families.7 Subsequently, in 1986 and together with Jane Leske they prepared the first version of the questionnaire Critical Care Family Needs Inventory (CCFNI). This is currently the most widely used instrument to detect and rank the needs of ICU patient families.8
However, in spite of having an instrument that was specially created to identify the needs of family members, some reports state that healthcare teams incorrectly identify the most important needs of the family. This is the case for nurses,9,10 doctors11 and other health professionals.12 There is now literature on research into the needs of critical patients’ families in several countries. In 2012, Chatzaki et al.,13 in a rural zone in Greece, found that the most important needs relate to security, and that these are independent of family member sociodemographic factors. Similarly, Chien et al.14 found no differences in the degree of importance of needs regarding age, educational level or relationship with the patient. On the other hand, in the United States, Obringer et al.15 found that the least important needs of family members were those connected with the dimension of support.
Given that the results obtained show that family members prioritise their needs differently, and that in some cases they are related to social and cultural needs,6 it is necessary to examine them in a particular way in each geographical and clinical context. Thus in Latin America a limited number of studies have been performed on the needs of ICU patients’ families. In 2007, research in Brazil by Freitas et al.16 showed that approximately 90% of the needs covered by the CCFNI were considered to be important or very important by the family members of patients in private and public health institutions there. Meanwhile in Chile no studies have been published on the needs of critical patients’ families. This study aims to identify the most important needs of the family members of patients hospitalised in the ICU of a university hospital in Santiago, Chile. Additionally, it also aims to analyse the relationship between the sociodemographic characteristics of family members and the degree of importance of the dimensions covered by the CCFNI. This is expected to show the needs and expectations of these family members, supplying information that makes it possible for healthcare teams to improve their experience during hospitalisation in an ICU.
MethodDesignThis descriptive, comparative transversal study was based on secondary analysis of Spanish validation process data corresponding to the CCFNI instrument. It was undertaken in a university hospital in Santiago, Chile.17
AreaThis study was performed in an ICU of a teaching hospital in the Metropolitan Region of Santiago, Chile. The ICU in the study has 2 units (medical and surgical), each one of which has 16 beds and a habitual ratio of nurses of from 1:2 to 1:3 beds. The visiting time in the unit lasts for 6h (13:00–19:00) and it is during this time that the family is informed every day about the condition of the patient.
SubjectsThe population studied consisted of all of the family members of the critical patients admitted during the period from July to September 2014. The size of the sample (n=251) was determined by means of sampling by convenience, using at least 5 subjects for each item of the original instrument.18 The inclusion criteria were: age over 18 years old, educational level equal to or higher than the 8th year of basic education, being a direct family member of a patient, having visited the patient at least once during their stay in the ICU, and that patients had to have been hospitalised for longer than 48h in the ICU.
VariablesThe chief variable studied was the degree to which the needs of family members were important, and these were identified by means of the CCFNI questionnaire. The other variables in the study were: age (years), sex (male/female), educational level (primary, secondary, technical college or university), relationship with the patient (father/mother, son/daughter, spouse, brother/sister or other) and previous experience in an ICU (yes/no).
Data gatheringThe CCFNI questionnaire is composed of 45 items with answers on a Likert scale from 1 (not important) to 4 (very important). They are grouped in 5 dimensions: security, support, information, comfort and proximity.7 It also includes a final item in which family members are able to freely express any needs they consider to be relevant and which are not included in the questionnaire. The psychometric properties of the original version of the CCFNI were evaluated in 1991, when it obtained an internal consistency for the general scale of α=0.92.7 In this Spanish validation study of the CCFNI it retained all of the items in its original version, with minimum linguistic adjustments to adapt it to Chilean culture, obtaining a factorial structure with 2 dimensions.17 The original structure of the CCFNI was considered for the purposes of this study, calculating the internal consistency of its 5 dimensions and obtaining acceptable levels of reliability for the dimensions of support (α=0.89), security (α=0.66), proximity (α=0.74), comfort (α=0.74) and information (α=0.72). A sociodemographic questionnaire was also applied, including: age, sex, educational level, relationship with the patient and previous experience in an ICU.
The questionnaires were given personally to family members during visiting times by previously trained research assistants. The family members signed the informed consent document beforehand. The data gathering period included the months of July, August and September 2014.
Data analysisFrequency and percentage tables were used to analyse the sociodemographic variables, while descriptive statistics were used to measure the degree to which needs are important. Analysis of the differences between the dimensions of the CCFNI and the sociodemographic variables corresponding to the family members used the Student t-test and ANOVA. The needs expressed in item number 46, for open answer, were classified in one of 6 categories according to the observed results: communication, atmosphere, psychological support, interaction with the healthcare team, visiting times and others. The criterion for rejection of the null hypothesis was a value of p 0.05. All statistical analyses were performed using SPSS Statistics v.18 statistical software.
Ethical considerationsThe original study was approved by the Ethics Committee of the Faculty of Medicine of the Pontificia Universidad Católica de Chile and the health institution where the study took place. In a similar way, the ethical aspects of the study took into account the 7 requisites established by Emanuel et al.19 for a study to be ethical. All of the subjects agreed to take part in the study by signing the informed consent document.
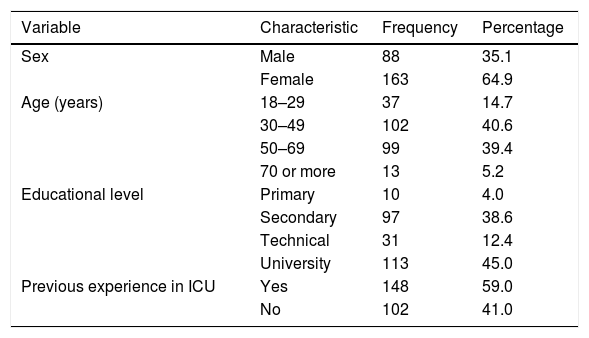
ResultsSociodemographic variablesOf the 251 patient family members surveyed, Table 1 shows that 64.9% were women and that more than 80% were aged from 30 to 69 years old. On the other hand, 45.0% stated that they had studied at university and 59.0% said that they had previous experience of a family member being admitted to an ICU.
Distribution of the sociodemographic characteristics of ICU patients’ family members.
| Variable | Characteristic | Frequency | Percentage |
|---|---|---|---|
| Sex | Male | 88 | 35.1 |
| Female | 163 | 64.9 | |
| Age (years) | 18–29 | 37 | 14.7 |
| 30–49 | 102 | 40.6 | |
| 50–69 | 99 | 39.4 | |
| 70 or more | 13 | 5.2 | |
| Educational level | Primary | 10 | 4.0 |
| Secondary | 97 | 38.6 | |
| Technical | 31 | 12.4 | |
| University | 113 | 45.0 | |
| Previous experience in ICU | Yes | 148 | 59.0 |
| No | 102 | 41.0 |
ICU: intensive care unit.
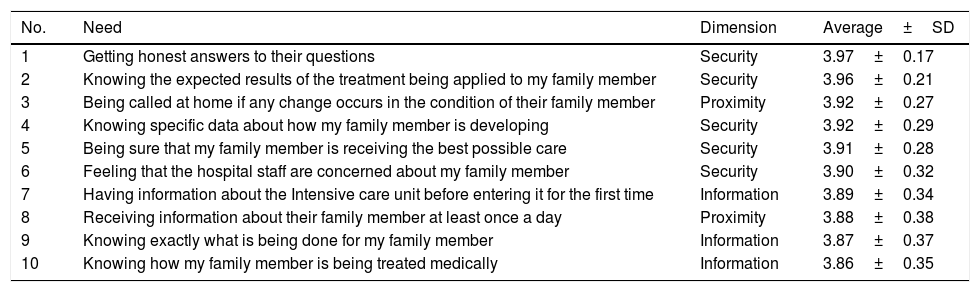
The majority of the most important needs mentioned by family members are grouped in the security dimension (X¯=3,90; DE=0.18), followed by the dimensions of information (X¯=3,76; DE=0.27), proximity (X¯=3,60; DE=0.36) and support (X¯=3,09; DE=0.28). More particularly, Table 2 shows the 10 most important needs, of which “receiving honest answers to my questions” (X¯=3,97; DE=0.17) is in first place. It is followed by “what the expected results are of the treatment that is being applied to their family member” (X¯=3,96; DE=0.21). Both of these needs belong to the dimension of security, while “being called if any change occurs in the condition of their family member” (X¯=3,92; DE=0.97), is included in the dimension of proximity.
Average and standard deviation of the 10 most important needs for ICU patients’ family members, according to the CCFNI.
| No. | Need | Dimension | Average±SD |
|---|---|---|---|
| 1 | Getting honest answers to their questions | Security | 3.97±0.17 |
| 2 | Knowing the expected results of the treatment being applied to my family member | Security | 3.96±0.21 |
| 3 | Being called at home if any change occurs in the condition of their family member | Proximity | 3.92±0.27 |
| 4 | Knowing specific data about how my family member is developing | Security | 3.92±0.29 |
| 5 | Being sure that my family member is receiving the best possible care | Security | 3.91±0.28 |
| 6 | Feeling that the hospital staff are concerned about my family member | Security | 3.90±0.32 |
| 7 | Having information about the Intensive care unit before entering it for the first time | Information | 3.89±0.34 |
| 8 | Receiving information about their family member at least once a day | Proximity | 3.88±0.38 |
| 9 | Knowing exactly what is being done for my family member | Information | 3.87±0.37 |
| 10 | Knowing how my family member is being treated medically | Information | 3.86±0.35 |
CCFNI: Critical Care Family Needs Inventory; SD: standard deviation; ICU: intensive care unit.
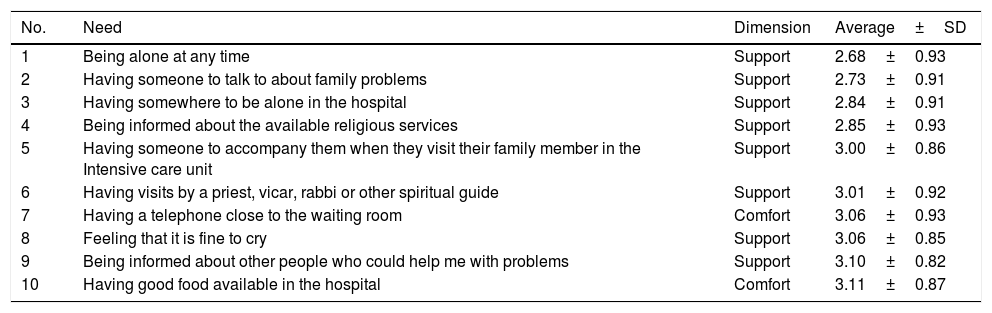
Table 3 shows that the majority of needs evaluated as less important are concentrated in the support dimension. “Being alone at any time” (X¯=2,68; DE=0.93) and “Having someone to talk to about family problems” (X¯=2,73; DE=0.91) scored the lowest.
Average and standard deviation of the 10 least important needs for ICU patients’ family members, according to the CCFNI.
| No. | Need | Dimension | Average±SD |
|---|---|---|---|
| 1 | Being alone at any time | Support | 2.68±0.93 |
| 2 | Having someone to talk to about family problems | Support | 2.73±0.91 |
| 3 | Having somewhere to be alone in the hospital | Support | 2.84±0.91 |
| 4 | Being informed about the available religious services | Support | 2.85±0.93 |
| 5 | Having someone to accompany them when they visit their family member in the Intensive care unit | Support | 3.00±0.86 |
| 6 | Having visits by a priest, vicar, rabbi or other spiritual guide | Support | 3.01±0.92 |
| 7 | Having a telephone close to the waiting room | Comfort | 3.06±0.93 |
| 8 | Feeling that it is fine to cry | Support | 3.06±0.85 |
| 9 | Being informed about other people who could help me with problems | Support | 3.10±0.82 |
| 10 | Having good food available in the hospital | Comfort | 3.11±0.87 |
CCFNI: Critical Care Family Needs Inventory; SD: standard deviation; ICU: intensive care unit.
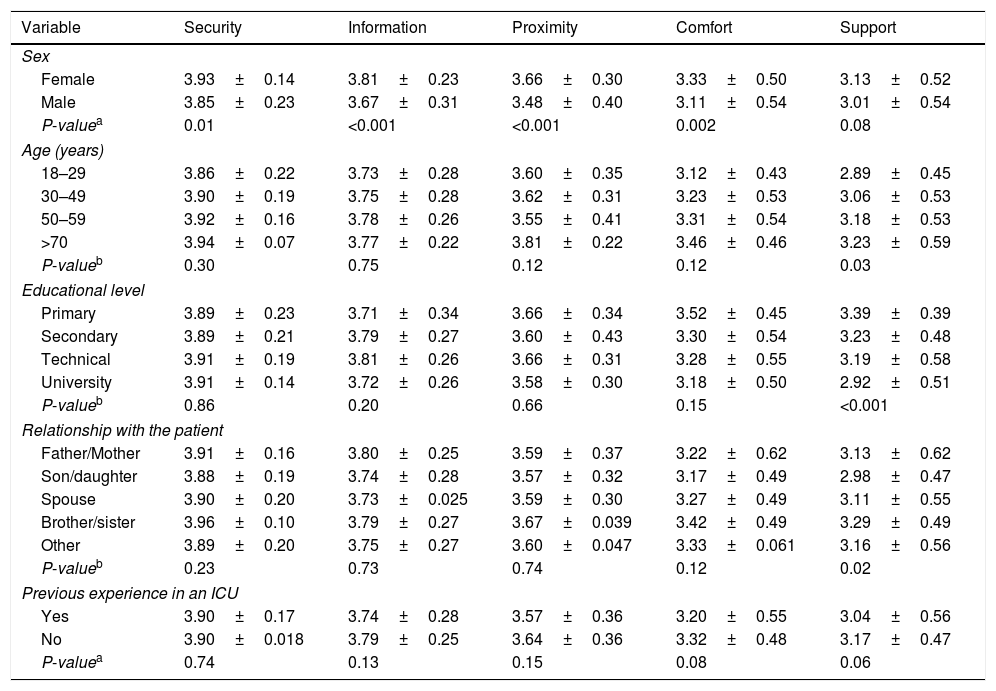
Table 4 shows the differences in the level of importance of the CCFNI dimensions according to family sociodemographic variables. The women assigned greater importance to their needs in all of the dimensions, particularly in those of information and proximity (p<0.001). Significant differences were only found in the support dimension for age, educational level and relationship with the patient. In this dimension the youngest family members (p=0.03), those with a higher level of education (p=0.001) and patients’ children (p=0.02) assigned less importance to these needs. No differences were detected between family members with or without prior experience in an ICU.
Average, standard deviation and differences between the scores of the CCFNI dimensions, according to sociodemographic variables.
| Variable | Security | Information | Proximity | Comfort | Support |
|---|---|---|---|---|---|
| Sex | |||||
| Female | 3.93±0.14 | 3.81±0.23 | 3.66±0.30 | 3.33±0.50 | 3.13±0.52 |
| Male | 3.85±0.23 | 3.67±0.31 | 3.48±0.40 | 3.11±0.54 | 3.01±0.54 |
| P-valuea | 0.01 | <0.001 | <0.001 | 0.002 | 0.08 |
| Age (years) | |||||
| 18–29 | 3.86±0.22 | 3.73±0.28 | 3.60±0.35 | 3.12±0.43 | 2.89±0.45 |
| 30–49 | 3.90±0.19 | 3.75±0.28 | 3.62±0.31 | 3.23±0.53 | 3.06±0.53 |
| 50–59 | 3.92±0.16 | 3.78±0.26 | 3.55±0.41 | 3.31±0.54 | 3.18±0.53 |
| >70 | 3.94±0.07 | 3.77±0.22 | 3.81±0.22 | 3.46±0.46 | 3.23±0.59 |
| P-valueb | 0.30 | 0.75 | 0.12 | 0.12 | 0.03 |
| Educational level | |||||
| Primary | 3.89±0.23 | 3.71±0.34 | 3.66±0.34 | 3.52±0.45 | 3.39±0.39 |
| Secondary | 3.89±0.21 | 3.79±0.27 | 3.60±0.43 | 3.30±0.54 | 3.23±0.48 |
| Technical | 3.91±0.19 | 3.81±0.26 | 3.66±0.31 | 3.28±0.55 | 3.19±0.58 |
| University | 3.91±0.14 | 3.72±0.26 | 3.58±0.30 | 3.18±0.50 | 2.92±0.51 |
| P-valueb | 0.86 | 0.20 | 0.66 | 0.15 | <0.001 |
| Relationship with the patient | |||||
| Father/Mother | 3.91±0.16 | 3.80±0.25 | 3.59±0.37 | 3.22±0.62 | 3.13±0.62 |
| Son/daughter | 3.88±0.19 | 3.74±0.28 | 3.57±0.32 | 3.17±0.49 | 2.98±0.47 |
| Spouse | 3.90±0.20 | 3.73±0.025 | 3.59±0.30 | 3.27±0.49 | 3.11±0.55 |
| Brother/sister | 3.96±0.10 | 3.79±0.27 | 3.67±0.039 | 3.42±0.49 | 3.29±0.49 |
| Other | 3.89±0.20 | 3.75±0.27 | 3.60±0.047 | 3.33±0.061 | 3.16±0.56 |
| P-valueb | 0.23 | 0.73 | 0.74 | 0.12 | 0.02 |
| Previous experience in an ICU | |||||
| Yes | 3.90±0.17 | 3.74±0.28 | 3.57±0.36 | 3.20±0.55 | 3.04±0.56 |
| No | 3.90±0.018 | 3.79±0.25 | 3.64±0.36 | 3.32±0.48 | 3.17±0.47 |
| P-valuea | 0.74 | 0.13 | 0.15 | 0.08 | 0.06 |
CCFNI: Critical Care Family Needs Inventory; ICU: intensive care unit.
Finally, the open question was answered by 15.6% of family members. They mentioned a total of 58 needs apart from those contained in the CCFNI. The majority of these needs were in connection with communication (22.4%) and the atmosphere and infrastructure of the unit (22.4%). Lower percentages were about needs associated with psychological support (12.1%), family interaction with the healthcare team (17.2%), visiting times (10.3%) and other matters (15.5%).
DiscussionThis is the first study of the needs of family members of patients hospitalised in an ICU in Chile using a widely used instrument like the CCFNI.
The results of this research are similar to those of previous studies, in which the needs in the dimensions of security and information are the most important for the family members of ICU patients,13,14,20 while needs associated with support or comfort are the least important.9,13,21,22 In some studies it was particularly observed that proximity17 is the second most important dimension, and it was even said the be the most important one in some studies.21
Specific analysis of the needs in different dimensions showed that the need for “honest answers to questions” was also identified as the most important one by other authors,14,15,23,24 and it was in the first 5 places in other studies.9,21,25,26 Likewise, “what the expected results of the treatment being applied to my family member” was found to be in the first 3 places.14,15,25 These findings suggest that needs associated with the delivery of information are found important by all ICU patient family members. In spite of this, the quality and quantity of information received by families in an ICU is not always appropriate. A study in France found that 54% of family members did not understand the diagnosis, prognosis or treatment when they were informed by a doctor.27 Moreover, if the first formal meeting lasts for less than 10min and if no informative booklet is delivered, these are identified as factors associated with insufficient comprehension of the information. The delivery of informative material has therefore been shown to be associated with better understanding of the patient prognosis as well as therapeutic procedures.28 Communication with the healthcare team may thereby help to improve understanding of the situation by the family and there reduce their emotional burden.25 On the other hand, given their training and closeness to family members ICU nurses are in a preferential position to detect and satisfy the needs of family members6: however, some barriers are thought to hinder effective communication. These include lack of time, the lack of a place for private conversation, wishing to avoid conflict with the medical team and disagreement with medical treatment plans.29
Although needs for support are classified by family members as less important, some of these needs score 3 or more. This implies that the dimension or need is still important for the family, although to a lesser extent. A recent systematic review of questionnaires designed to evaluate the needs and degree of satisfaction of ICU patients’ families, it was proposed that these instruments should use broader Likert's scales from 1 to 7 points, for example. This would make it possible to optimise the depth of answers and the sensitivity of the construct evaluated.8
The dimension of support in the CCFNI includes needs associated with resources and support systems or structures.7 Although these are less important than other factors, they may be a source of satisfaction for families. For example, on analysing the effect of changing the physical environment of an ICU, a significant increase in family satisfaction was found when an old windowless 32 bed ICU with 12m2 per bed was changed for a new one with 36 individual rooms each measuring 25m2 and with large windows.30 Although some authors state that meeting the needs of family members in an ICU is not synonymous with satisfaction, and that on the contrary, not meeting their needs leads to dissatisfaction,31 this is only true when the real importance that a family assigns to their needs is unknown. Thus properly identifying family needs will make it possible for healthcare teams to prioritise satisfying the most important ones, according to the available resources and organisational priorities. The use of management tools such as importance-relevance analysis,32 which compares the importance of a need with the degree to which it is satisfied, may make it possible to know which of the most important needs are not currently satisfied.
Regarding the influence of sociodemographic variables, the fact that the women consider their needs to be more important agrees with other studies.14,33 Similarly the higher proportion of women in our sample is also in agreement with the literature,14,34 at this proportion even reaches 88% in some studies.24 These differences in gender regarding the ranking of the majority of needs makes it necessary, in those ICUs where women form the highest proportion of family members, to evaluate the possibility of implementing differentiated strategies to satisfy their most important needs.
The age of family members in our sample was similar to the age reported by other authors,20,35 while in Asian families populations 25% younger than is the case in Chile are described.14,20,26 Children are the predominant family relationship with the patient in this study, while in the literature the percentage of children is said to run from 33.2%14 up to 82.5%.22 The relationship between age and the dimensions in the CCFNI is a challenge for ICUs, particularly in terms of the needs for support and comfort. In the case of older family members these dimensions include basic needs which are highly important for older people, such as access to a toilet and telephone or the availability of food. A study performed in Germany only describes a relationship between age and needs within the comfort dimension.33 On the other hand, the importance of certain elements such as spirituality or religiosity in the support dimension may be explained by the fact that they are associated with higher levels of happiness, quality of life and mental health in this age group.36,37
The fact that family members with a higher level of education consider the information dimension to be less important may be explained by their better comprehension of the information they receive. This means that they feel less need for other aspects involved in the process of communicating with the healthcare team. In terms of the support and comfort dimensions, a lower educational level may be associated with lower income, and this would imply assigning greater importance to these needs in comparison with better educated family members.
Finally, a relevant proportion of family members in this research (15.6%) mentioned additional needs apart from those described in the CCFNI. Although this result is similar to those reported in other studies,13,22 the literature reports few studies in which additional needs were observed.20 Nevertheless, in our study many of these “new needs” correspond to remarks associated with evaluation of the care received, and this makes it necessary to optimise the channels of communication with families, so that they are able to express their concerns appropriately.
Although this is the first report of the use of the CCFNI in our country, our study has some limitations. Firstly, it was undertaken in a single private ICU, so that it is not necessarily possible to extrapolate its results to other hospitals. Additionally, the private nature of the ICU studied means that some factors should be taken into account when interpreting our results. In a study that compared the needs of family members in public and private hospitals, significant differences were detected in how they ranked their needs.16 Lastly, the socioeconomic level of family members was not evaluated. Doing so may have helped to create a more complete picture in connection with the ranking of the needs that were evaluated.
ConclusionIn this first study to be conducted in Chile, the most important needs for critical patients’ families connect mainly with aspects of communication with the healthcare team. These involve not only the type of information that is delivered by also how this takes place. It was also found that the sociodemographic variables of family members influences the majority of the needs they classify as less important, and these should be taken into consideration in the same way.
Future lines of research in this area should centre on developing strategies that make it possible to improve communications between the healthcare team and critical patients’ families. Similarly, only being aware of family needs is not enough, so that it is fundamental to evaluate the degree to which they are satisfied. Finally, exploring the degree to which health institutions are disposed to identify and satisfy these needs could become a key aspect in making hospitalisation in an ICU a less traumatic experience.
Ethical disclosuresProtection of human and animal subjectsThe authors declare that the procedures followed conform to the ethical norms of the responsible human experimentation committee, the World Medical Association and the Helsinki Declaration.
Confidentiality of dataThe authors declare that they followed the protocols of their centre of work regarding the publication of patient data.
Right to privacy and informed consentThe authors obtained the informed consent of the patients and/or subjects referred to in the paper. This document is held by the corresponding author.
FundingThis study was supported by the Nursing School Research Directorship of the Pontificia Universidad Católica de Chile by means of the research grant “Integración Docente Asistencial (IDA)” 2013.
Conflicts of interestThe authors have no conflict of interests to declare.
We would like to thank all of the critical patients’ family members who generously took part in this study.
Please cite this article as: Padilla-Fortunatti C, Rojas-Silva N, Amthauer-Rojas M, Molina-Muñoz Y. Necesidades de los familiares de pacientes críticos en un hospital académico de Chile. Enferm Intensiva. 2018;29:32–40.