1) To determine noise levels in two paediatric intensive care units (PICU) of a tertiary hospital and 2) to analyse whether these values comply with the current standards.
MethodObservational, descriptive and cross-sectional study carried out in two PICU with different infrastructure: bays separated by curtains and individual bedrooms. A PCE-999 sound level meter was used to determine noise levels, which were registered in decibels (dB). At the same time, an ad hoc data recording document was designed in which we differentiated between each unit (open concept or closed), time of recording.
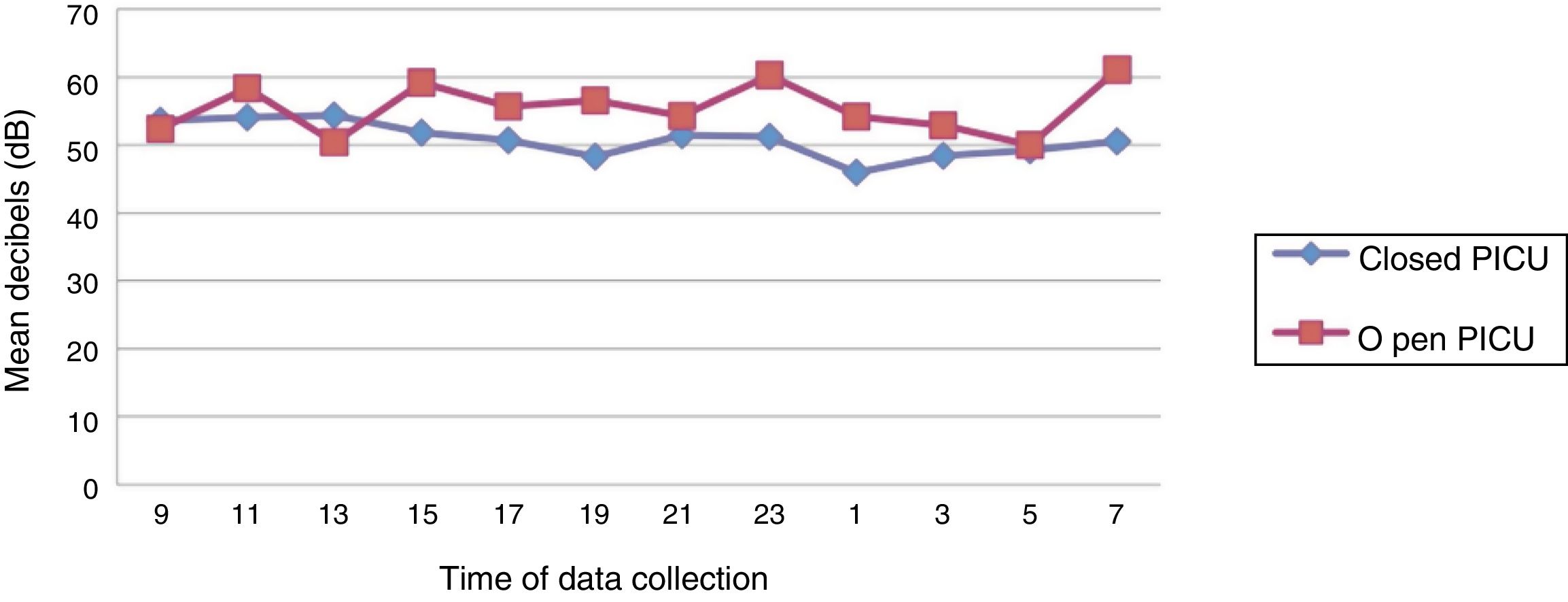
ResultsA total of 330 tests, 72 from open PICUs and 258 from closed PICUs were collected. The noise in the open PICU was 56.74 ± 3.61 decibels versus 50.36 ± 4.71 in the closed PICU, obtaining the highest levels during the morning.
DiscussionAs it occurs in other studies, noise levels exceed the allowed limits. At the same time, the main sources of noise in the PICU came from alarms, medical equipment, such as monitors or respirators, and conversations between health professional.
ConclusionsThis investigation has shown high levels of environmental noise in the two PICUs analysed. The data obtained indicate that the architectural concept of individual bedrooms may have an impact in decreasing this environmental input.
1) Determinar los niveles de ruido ambiental en dos unidades de cuidados intensivos pediátricos (UCIP) de un hospital pediátrico de tercer nivel asistencial y 2) analizar si dichos valores cumplen con la normativa actual.
MétodoEstudio observacional, descriptivo y transversal llevado a cabo en dos UCIP con infraestructura diferente: boxes separados por cortinas y habitaciones individuales. Se empleó un sonómetro PCE-999 tipo 2 para determinar el ruido ambiental y la unidad de medida registrada fue en decibelios (dB). A la vez, se diseñó un documento de recogida de datos ad hoc diferenciando entre unidad (abierta y cerrada), hora de registro.
ResultadosSe recogió un total de 330 determinaciones, 72 en la UCIP abierta y 258 en la de habitaciones individuales. El ruido ambiental que imperaba en la unidad de críticos abierta fue de 56,74 ± 3,6 decibelios versus 50,36 ± 4,7 en la de boxes individuales, observándose valores mayores en el turno diurno.
DiscusiónTal como sucede en otros estudios previos, se observa que el ruido que impera en la unidad excede los límites permitidos. Además, se coincide con el hecho de que las principales fuentes de ruido ambiental de la UCI provienen de las alarmas, la maquinaria, como monitores o respiradores y las conversaciones entre profesionales sanitarios.
ConclusionesTras la presente investigación, se ha podido constatar que los niveles de ruido ambiental que imperan en las dos Unidades de Cuidados Intensivos Pediátricos analizadas son elevados. Los datos obtenidos apuntan a que la organización arquitectónica de concepto cerrado puede tener un impacto a la hora de disminuir la generación de dicho input medioambiental.
Paediatric intensive care units (PICU) are independent hospital care areas that have been designed for the treatment of patients who, due to disease severity or potentially fatal conditions require comprehensive and continuous observation and intensive medical care by a team with specific competencies.1 Therefore, these units offer the latest technological and healthcare advances to the critical patient, because they need them for their immediate survival. In addition PICU have qualified staff to apply these technologies, and an infrastructure that facilitates the continuous care dynamics required by the critical patient.2–4
From all of the above, it is clear that intensive care units are areas exposed to high levels of ambient noise, especially from the equipment used to manage the critical patient (monitors, continuous infusion pumps for medication or enteral nutrition, etc.), and from the activity of healthcare personnel.5 Noise is an unwanted sound that causes an adverse psychological effect or discomfort on the listener.6 According to the World Health Organisation (WHO), physically there is no difference between sound and noise, as the brain works to make everything it perceives consistent through interpretation.7 Even so, noise pollution is, according to the WHO, one of the main health problems that affects all humans, but particularly those with impaired physical and/or psychological faculties, such as the critical paediatric patient.8 For all these reasons, continuous unwanted noise or sounds, such as that generated by machinery in critical areas, can lead to delirium, stress and discomfort, and have harmful effects such as sustained stress and risk for medication or care errors in healthcare personnel.9,10
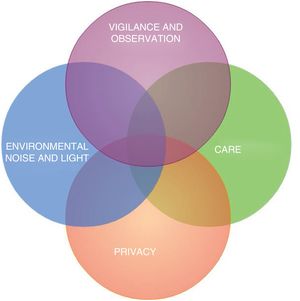
In this regard, the design of the PICU structure is an important aspect to consider, given that its interdependent characteristics (Fig. 1) directly influence the satisfaction of patients and their families and healthcare staff, and impact the applied critical care model.2 In general, intensive care units are structured as circular, square or rectangular in shape with a central station from which the haemodynamic situation and clinical progression of the critical patient is monitored. All patients are admitted to individual bedrooms, or separated by curtains, and are closely monitored.11
Aware of the importance of controlling the environmental noise that prevails in critical care units and the importance of making healthcare professionals aware of this fact, we decided to undertake a study in two PICUs of a tertiary level paediatric hospital with a different infrastructure to 1) determine environmental noise levels received by nursing staff and 2) analyse whether these levels complied with current regulations.
MethodType and place of studyAn observational, descriptive, and cross-sectional study was conducted in two PICUs of a tertiary paediatric hospital. Coinciding with a project to create and build a new critical area, and in order to improve the control and management of environmental noise, we decided to first undertake a descriptive study to determine this input in an open PICU.12 Later, after the new closed concept unit had been open for a year (this period was taken after subjectively observing with the healthcare staff how they were adapting to the new infrastructure, and to various changes in work dynamics [subdivision of patients by medical specialty, new software for recording vital signs, nursing care and dispensing drugs, etc.]), environmental noise levels were again tested.
The first PICU (open concept located on the fourth floor of the general children’s hospital building, had an overall area of approximately 500 m2, was circular in structure and comprised 14 beds (two individual bedrooms with a door and 12 open bays separated by curtains), which shared single nurse station. The second paediatric intensive care unit that we studied (closed concept), located on the third floor of the children’s hospital building, had an area of about 2.500 m2, comprised 24 individual bedrooms with a door divided into three spaces with their corresponding three nursing stations; two spaces comprised seven beds and the other 10. At this point, it is important to note we confirmed with the managers of the new PICU works that no insulation materials against environmental noise had been used.
The critical care units analysed care for patients with diverse diseases (respiratory, neurological, cardiological, nephrological, oncological and infectious), as well as postoperative patients.
Study periodThe environmental noise measurements in the open PICU were made consecutively for six days (from Monday to Saturday) in December 2016 12; in the closed concept unit, the measurements were made in the same way for 6 days in April 2019. In this regard, it is relevant to highlight that, although the data was recorded in different months, it was confirmed through the activity register that occupancy in both units was 100% at the time of the study; i.e., in the open PICU, at the time of recording, there were 14 patients, and 24 in the closed PICU.
Data collection instrumentsA class II sound level meter PCI-999 with an accuracy of 1.5 dB, previously validated and calibrated by the company from which it was purchased, was used to determine the environmental noise, registered in decibels (dB). At the same time, an ad hoc data collection document was designed differentiating between unit (open and closed), time of recording and amount of noise (recorded in absolute numbers and dB).
The benchmark values established by the American Academy of Paediatrics (AAP), the Environmental Health Committee and the World Health Organization (WHO) were taken into consideration.13 These organisations establish that environmental noise levels >45 decibels during the day and >35 during the night are harmful to patients.
Data collection procedureFirst, a team was formed from a nurse from each shift (day and night) with a minimum of 3 years’ experience in the management of paediatric critical patients. Both PICU followed the same work shifts (morning, afternoon, and night), although they were combined into two for the study (from 8:01 to 20:00 and from 20:01 to 8:00). These professionals were instructed in the use of the sound level meter used in this study, as well as in the process of data collection and the ad hoc document designed for recording data.
The environmental noise level was recorded on the ad hoc grid every two hours for 6 consecutive days (Monday to Saturday) in both units. It was decided to make the recording every 2 h because this was considered subjectively by the research team and because there was no sound level meter to record this noise continuously, to be the time when most care activities are carried out by the internal organisation of the department.
Given that the aim was to determine the level of environmental noise to which the nursing staff working in the two PICUs are subjected, this input was recorded at the nursing stations. In the case of the open PICU, it was determined in the single nursing station and, in the closed or individual bedrooms, it was taken simultaneously in each of the three nursing stations of the closed PICU. Since only one sound level meter was used, there was an interval of 45–60 s between the measurements at each nursing station in the closed PICU.
To prevent the care professional working when the noise was being measured from modifying their behaviour because they were being observed (Hawthorne effect), these recordings were carried out without the professional being aware of it. To do this, the researcher taking the environmental noise measurements placed the sound level meter in an area of the nursing station not visible to the other professionals.
This study was approved by the nursing management and the head of the unit where it was undertaken.
Statistical analysisThe numerical variables related to the dB of environmental noise were described using descriptive statistics of mean and standard deviation. We used the Wilcoxon test for two samples to compare the values of a numerical variable between paired simples. For two independent simples either the Mann–Whitney U-test or Student’s t-test was used, as appropriate. The data were considered statistically significant with a p < .05.
ResultsA total of 330 measurements of environmental noise were taken, 72 in the open PICU and 258 in the unit with individual bedrooms (86 measurements at each of the three nursing stations studied).
The environmental noise in the open critical unit was 55.45 ± 3.0 decibels12 versus the mean 50.80 ± 2.8 in the three nursing stations of the PICU with individual bedrooms (50.43 ± 5.8 in number 1; 51.99 ± 5.6 in number 2 and 49.94 ± 5.1 decibels in number three).
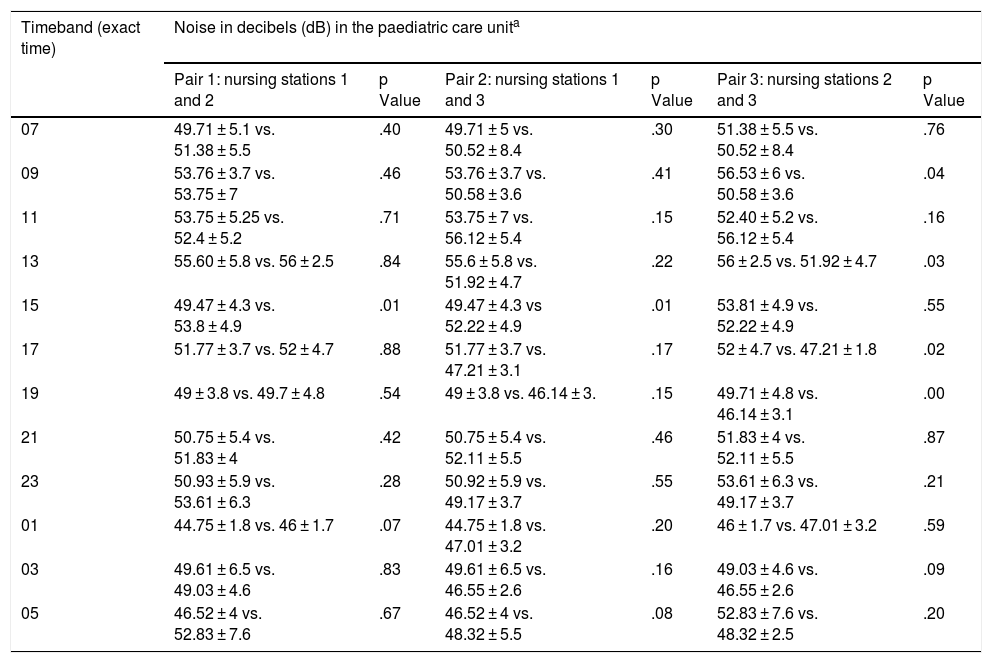
A comparative analysis was made between the three nursing stations of the closed PICU and statistical significance was obtained by comparing stations 1 and 2 (p = .01) and 2 and 3 (p = .00). In addition, this analysis was examined further taking the established recording timebands and statistical significance was observed when comparing station 1 with 2 and 3 in the 15:00 timeband (p = .01) and when comparing stations 2 and 3 at 9:00 (p = .04), 13:00 (p = .03), 17:00 (p = .02) and at 19:00 (p = .00), Table 1.
Mean environmental noise in decibels according to timeband and nursing station in the intensive care unit with individual bedrooms.
| Timeband (exact time) | Noise in decibels (dB) in the paediatric care unita | |||||
|---|---|---|---|---|---|---|
| Pair 1: nursing stations 1 and 2 | p Value | Pair 2: nursing stations 1 and 3 | p Value | Pair 3: nursing stations 2 and 3 | p Value | |
| 07 | 49.71 ± 5.1 vs. 51.38 ± 5.5 | .40 | 49.71 ± 5 vs. 50.52 ± 8.4 | .30 | 51.38 ± 5.5 vs. 50.52 ± 8.4 | .76 |
| 09 | 53.76 ± 3.7 vs. 53.75 ± 7 | .46 | 53.76 ± 3.7 vs. 50.58 ± 3.6 | .41 | 56.53 ± 6 vs. 50.58 ± 3.6 | .04 |
| 11 | 53.75 ± 5.25 vs. 52.4 ± 5.2 | .71 | 53.75 ± 7 vs. 56.12 ± 5.4 | .15 | 52.40 ± 5.2 vs. 56.12 ± 5.4 | .16 |
| 13 | 55.60 ± 5.8 vs. 56 ± 2.5 | .84 | 55.6 ± 5.8 vs. 51.92 ± 4.7 | .22 | 56 ± 2.5 vs. 51.92 ± 4.7 | .03 |
| 15 | 49.47 ± 4.3 vs. 53.8 ± 4.9 | .01 | 49.47 ± 4.3 vs 52.22 ± 4.9 | .01 | 53.81 ± 4.9 vs. 52.22 ± 4.9 | .55 |
| 17 | 51.77 ± 3.7 vs. 52 ± 4.7 | .88 | 51.77 ± 3.7 vs. 47.21 ± 3.1 | .17 | 52 ± 4.7 vs. 47.21 ± 1.8 | .02 |
| 19 | 49 ± 3.8 vs. 49.7 ± 4.8 | .54 | 49 ± 3.8 vs. 46.14 ± 3. | .15 | 49.71 ± 4.8 vs. 46.14 ± 3.1 | .00 |
| 21 | 50.75 ± 5.4 vs. 51.83 ± 4 | .42 | 50.75 ± 5.4 vs. 52.11 ± 5.5 | .46 | 51.83 ± 4 vs. 52.11 ± 5.5 | .87 |
| 23 | 50.93 ± 5.9 vs. 53.61 ± 6.3 | .28 | 50.92 ± 5.9 vs. 49.17 ± 3.7 | .55 | 53.61 ± 6.3 vs. 49.17 ± 3.7 | .21 |
| 01 | 44.75 ± 1.8 vs. 46 ± 1.7 | .07 | 44.75 ± 1.8 vs. 47.01 ± 3.2 | .20 | 46 ± 1.7 vs. 47.01 ± 3.2 | .59 |
| 03 | 49.61 ± 6.5 vs. 49.03 ± 4.6 | .83 | 49.61 ± 6.5 vs. 46.55 ± 2.6 | .16 | 49.03 ± 4.6 vs. 46.55 ± 2.6 | .09 |
| 05 | 46.52 ± 4 vs. 52.83 ± 7.6 | .67 | 46.52 ± 4 vs. 48.32 ± 5.5 | .08 | 52.83 ± 7.6 vs. 48.32 ± 2.5 | .20 |
vs. = versus.
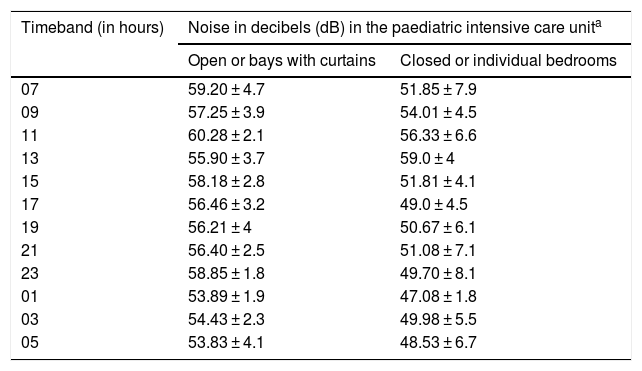
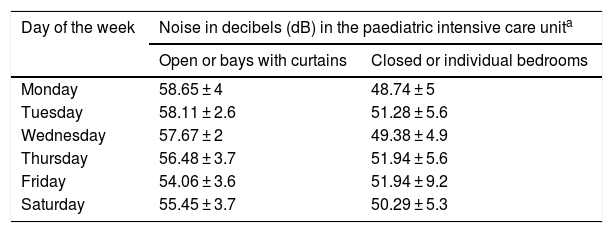
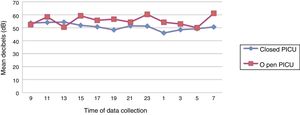
When comparing the mean environmental noise by unit and timeband, statistical significance was observed at 15:00 (p = .04), at 17:00 (p = .01), at 23:00 (p = .03) and at 01:00 (p = .00), Table 2 and Fig. 2. In turn, the data were grouped and analysed by day of the week (Table 3), and significant variations were observed when comparing Monday-Friday (p = .002), Monday-Saturday (p = .01), Tuesday-Friday (p = .001) and Wednesday-Friday (p = .01) in the open PICU and Monday-Tuesday (p = .05), Monday-Thursday (p = .06), Tuesday-Wednesday (p = .04), Wednesday-Friday (p = .01), Thursday-Saturday(p = .01) and Friday-Saturday (p = .02) in the closed PICU. Finally, the data were analysed by work shift, observing a mean 55.45 ± 3.0 dB during the day (from 8:01 to 20:00) versus 55.46 ± 1.1 at night (20:01 to 8:00) in the open PICU and 52.14 ± 1.45 during the day versus 49.46 ± 1.9 at night in the individual bedrooms. When comparing work shifts (morning and night) statistically significant differences were observed (p < .000).
Overall environmental noise levels in decibels according to timeband and PICU.
| Timeband (in hours) | Noise in decibels (dB) in the paediatric intensive care unita | |
|---|---|---|
| Open or bays with curtains | Closed or individual bedrooms | |
| 07 | 59.20 ± 4.7 | 51.85 ± 7.9 |
| 09 | 57.25 ± 3.9 | 54.01 ± 4.5 |
| 11 | 60.28 ± 2.1 | 56.33 ± 6.6 |
| 13 | 55.90 ± 3.7 | 59.0 ± 4 |
| 15 | 58.18 ± 2.8 | 51.81 ± 4.1 |
| 17 | 56.46 ± 3.2 | 49.0 ± 4.5 |
| 19 | 56.21 ± 4 | 50.67 ± 6.1 |
| 21 | 56.40 ± 2.5 | 51.08 ± 7.1 |
| 23 | 58.85 ± 1.8 | 49.70 ± 8.1 |
| 01 | 53.89 ± 1.9 | 47.08 ± 1.8 |
| 03 | 54.43 ± 2.3 | 49.98 ± 5.5 |
| 05 | 53.83 ± 4.1 | 48.53 ± 6.7 |
Overall environmental noise levels in decibels according to the day of the week and PICU.
| Day of the week | Noise in decibels (dB) in the paediatric intensive care unita | |
|---|---|---|
| Open or bays with curtains | Closed or individual bedrooms | |
| Monday | 58.65 ± 4 | 48.74 ± 5 |
| Tuesday | 58.11 ± 2.6 | 51.28 ± 5.6 |
| Wednesday | 57.67 ± 2 | 49.38 ± 4.9 |
| Thursday | 56.48 ± 3.7 | 51.94 ± 5.6 |
| Friday | 54.06 ± 3.6 | 51.94 ± 9.2 |
| Saturday | 55.45 ± 3.7 | 50.29 ± 5.3 |
As in other studies, we observed that the noise in the unit exceeds permitted limits.12,14–17 Even so, the infrastructure of the closed PICU with individual bedrooms appears useful in considerably controlling this environmental input. This hypothesis is also upheld by Delaney et al. in their review article on this problem.18
The data obtained in this study reveals that environmental noise levels are similar to other studies, such as a multicentre research study carried out in 6 critical care units that determined mean levels of 54.0 ± 2.4 dB,19 and another conducted in a PICU in Colombia, in which values were recorded of between 57.07 ± 3.07 and 65.72 ± 2.46 dB, with a maximum of 68.69 ± 3.57–79.06 ± 2.34 dB. This study also concludes that the highest levels of environmental noise were recorded during the morning and afternoon, with lower levels observed during the night and early morning.5 In our study, higher environmental noise levels were found in the morning shift only in the closed PICU, especially in some timebands that coincide with shift changes and ward rounds between nursing staff and between doctors or nurses.
In addition, our research study found significance when comparing noise levels at the beginning (Monday-Tuesday) and the end of the week (Friday-Saturday) in the case of the open PICU, which could be associated with the behaviour of healthcare professionals at the end of the working week (increase in conversations, activities in corridors, etc.), although this was not observed in the closed concept PICU. These results could not be compared because we found no similar research studies.
The main sources of noise that all healthcare staff working in an ICU must be aware of, according to the study conducted in 2013 in an adult cardiac ICU in Illinois by Stayt et al., are alarms (principal source of environmental noise in ICUs), medical equipment, such as monitors or respirators, conversations between nurses, drug trolleys, activities in corridors and opening and closing patients’ bedroom doors, the highest decibels being perceived in areas close to the nurses’ station.20 This was contrasted with the qualitative research study by Johansson et al. which adds to these inputs noise relating to healthcare (emergency or non-emergency) and conversations about the treatment and care of other patients21 and another study by Carrera-Hernández, et al.22 The fact highlighted by the above authors that the vast majority of noise input is concentrated in the care areas of the PICU is why we measured environmental noise in these nursing stations.
Despite the importance of controlling environmental noise, its assessment in critical areas is still insufficient. A study carried out by Escudero et al. in 2015 which analysed, among other aspects, the architectural and equipment characteristics of 135 ICUs throughout Spain (133 for adult patients and 2 for paediatric patients) revealed that only 2 of the adult units had an environmental noise meter, while 128 did not systematically monitor this input. Furthermore, there is a lack of evidence to confirm the best interventions to reduce noise, as well as the harmful effects that it has on the patient, such as reduction of sleep quality.18,23 Even so, a research study in which an initiative called quiet time was established achieved a reduction in environmental noise levels of between 10 and 15 dB, with a favourable qualitative perception by patients, families and care staff.24,25 This initiative, apart from educating with training and awareness raising among professionals on the importance of reducing environmental noise, providing healthcare staff with information on this input in real time through the installation of meters, focuses on limiting daily clinical activity to devote a specific time for patients to rest. In addition, it emphasises as possible solutions to this problem providing patients with earplugs and masks to mitigate the harmful effects of environmental factors of light and noise in the ICU. Therefore, as highlighted in the 2005 study by Christensen, intensive care unit staff need to be educated in the management and the harmful effects of environmental noise, as this knowledge is even more deficient among ICU staff.26
The main limitation of the present study is that it is single centre, and therefore further research is required that compares infrastructure and different work dynamics and environmental noise levels. Although we confirmed the correct calibration of the sound level meter with the company from which it was purchased, possible variability is another possible limitation of the study and the environmental noise could not be measured continuously. Another limitation to consider is that the environmental noise was measured in two PICUs that due to their structure differences were non-comparable. Furthermore, in the closed PICU, the measurements were carried out in the different nursing stations, and therefore the decibels obtained could be different to those actually perceived by the patient. Further research could seek to compare whether the noise in the care areas differs from that perceived by the patient at the bedside, especially in closed PICUs, and to identify noise sources and potential prevention measures.
ConclusionsAfter this research study, the environmental noise levels in the two paediatric intensive care units analysed were found to be high. The data obtained suggest that the concept of closed architectural organisation may have an impact in reducing this environmental input. However, because the noise levels were recorded at the nursing stations, further research should focus on determining noise levels at the patient’s bedside.
FundingThe first part of the research study, which includes the study conducted in 2016, was funded by Barcelona’s Fundación Enfermería y Sociedad del Colegio Oficial de Enfermeras y Enfermeros (Nursing and Society Foundation of the Official College of Nurses) in their 2016 call for research grants (PR-009/16).
Conflict of interestThe authors have no conflict of interest to declare.
Please cite this article as: Bosch-Alcaraz A, Fernández-Lorenzo R, Saz-Roy MA, Domínguez-Delso MC, Santaolalla-Bertolin M, Ferrer-Orona M, Alcolea-Monge S. Niveles de ruido ambiental en dos unidades de cuidados intensivos pediátricos con diferente infraestructura. Enferm Intensiva. 2020. https://doi.org/10.1016/j.enfi.2020.02.007