For laboratory sample extraction through catheters, blood volume must be discarded prior to specimen collection to ensure the accuracy of the results.
ObjectivesTo analyse the discarded blood volume obtained through vascular catheters, according to type of catheter, professional experience in extraction and hospital in Adult Intensive Care Units (ICU) of the Balearic Islands.
MethodCross-sectional multicentre descriptive study. Conducted from April to December 2018. Field of study: Adult Intensive Care Units of the Balearic Islands. Population: 296 nurses. Sample: nursing professionals who answered the survey. Data collection instrument: ad hoc, anonymous and voluntary questionnaire. Variables studied: waste volume, type of catheter, sex, professional experience and hospital. Descriptive statistical analysis, standard deviation, coefficient of variation, and non-parametric tests: Kruskal-Wallis and Median test with an CI: 95%, using the SPSS vs20.0 programme.
Results142 surveys were obtained, 12 hospitals participated: 6 public and 6 private, 72.5% women and 27.5% men. The total mean volume discarded was 5.98 mL (± 3.01): peripheral venous catheter (CVP) 5.74 mL (± 2.85), arterial cannula 4.37 mL (± 2.93), peripheral access central catheter (PICC) 7.34 mL (± 3.03) and central venous catheter (CVC) 6.49 mL (± 2.99). The medians of waste volume vary greatly between the different ICUs (p < .001). Private hospitals discard larger volumes than public hospitals through CVP: 5.12 mL (±2.15) vs 6.99 mL (±2.80) (p = .023), CVC: 5.92 mL (±2.58) vs 7.93 mL (±1.71) (p = .026) and PICC: 6.77 mL (±2.73) vs 9.07 mL (±2.05) (p = .004).
ConclusionsThere is a great variability in the volume of blood discarded, it depends on the hospital. No association was found between the discarded blood and the other variables studied. More conservative extraction techniques should be used.
Para la extracción de muestras de laboratorio a través de catéteres, se debe desechar un volumen de sangre para garantizar la exactitud de los resultados.
ObjetivosAnalizar el volumen sanguíneo desechado obtenido a través de catéter vascular y relacionarlo con el tipo de catéter, la experiencia del profesional que realiza la extracción y el centro hospitalario, en las Unidades de Cuidados Intensivos (UCI) de adultos de les Illes Balears.
MétodoEstudio descriptivo multicéntrico transversal. Ámbito de estudio: Unidades de Cuidados Intensivos de adultos de les Illes Balears. Población: 296 enfermeras. Instrumento de recogida de datos: cuestionario ad hoc, anónimo y voluntario. Variables estudiadas: volumen de desecho, tipo de catéter, sexo, experiencia profesional y hospital. Análisis estadístico descriptivo, desviación estándar, coeficiente de variación, y pruebas no paramétricas: Kruskal -Wallis y prueba de la Mediana con un IC: 95%, mediante el programa SPSS vs20.0.
ResultadosSe obtuvieron 142 encuestas, participaron 12 hospitales: 6 públicos y 6 privados. 72,5% mujeres y 27,5% hombres. El volumen medio total desechado fue de 5,98 ml (±3,01): catéter venoso periférico (CVP) 5,74 ml (±2,85), cánula arterial 4,37 ml (±2,93), catéter central acceso periférico (PICC) 7,34 ml (±3,03) y catéter venoso central (CVC) 6,49 ml (±2,99). Las medianas de volumen de desecho fueron muy variables entre las diferentes ucis (p < 0,001). Los hospitales privados desechan mayores volúmenes que los públicos a través de CVP: 5,12 ml (±2,15) vs 6,99 ml (±2,80) (p = 0,023), CVC: 5,92 ml (±2,58) vs 7,93 ml (±1,71) (p = 0,026) y PICC: 6,77 ml (±2,73) vs 9,07 ml (±2,05) (p = 0,004).
ConclusionesExiste una gran variabilidad en el volumen de sangre desechado en función del hospital donde se realiza la extracción. No se ha encontrado asociación entre la sangre desechada y el resto de variables estudiadas. Se deberían utilizar técnicas de extracción más conservadoras.
What is known?
For laboratory sample extraction through catheters, blood volume must be discarded prior to specimen collection to ensure the accuracy of results. There is no standard recommendation in the literature on the volume to be discarded, which depends on factors such as the type of catheter, the extraction technique and the experience of the health professional taking the sample.
What does this paper contribute?
This study is aimed at raising awareness among nurses of the importance of using conservative blood collection techniques that reduce blood loss related to diagnostic laboratory tests.
Implications for practice
Determining variability in clinical practice will make it possible to analyse the possibilities for improvement in each care centre and to direct strategies to prevent iatrogenic anaemia and ensure patient safety.
Critically ill patients require blood to be taken frequently for diagnostic and therapeutic purposes. Catheters are a good resource for obtaining blood samples to minimise damage to the patient, preserve vein integrity and avoid continuous punctures that can cause pain and anxiety.1 Extraction via vascular catheters is common practice in Intensive Care Units (ICU) and venipuncture is used in very few cases,2 although it is the most reliable technique for taking blood samples. On the other hand, methods of discarding can have inherent risks due to contamination of the catheter, of the solutions that are being infused, which can alter the sample and therefore the blood results; they also increase the blood volume required for analytical sample testing.3
What is the indicated amount of discarded blood to obtain quality samples through vascular catheters? The Clinical and Laboratory Standards Institute (CLSI) recommend discarding twice the catheter’s dead space or purge volume. However, if anticoagulation therapy has been administered prior to coagulation tests, 6 times the dead space volume should be discarded.4 This is a complex issue, given the wide variety of catheters on the market. For this reason, as a general recommendation they stipulate discarding 5 mL in short catheters, and 11 mL for certain types of central venous catheters (CVC).4
The literature compares the validity of blood samples taken through different intravenous catheters and those obtained through venipuncture; they recommend discarding a volume of 3.5 mL, 5 mL or 10 mL.5–7 Other studies relate the type of catheter with the minimum discard volume to obtain reliable blood samples, in tunnelled catheters they recommend 9 mL and in non-tunnelled catheters 6 mL.8 These blood losses are especially relevant in patients admitted to intensive care areas. Some authors have analysed discard volumes in the critical patient, describing figures ranging from 28.5% (20 mL)9 to 40 % (31.6 mL) of total blood volume collected10 in the first 24 h from admission. There is no consensus in the literature consulted regarding the standard discard volume for collecting samples through a vascular catheter.
The different methods for obtaining blood samples through catheters include reinfusion, mixing or push-pull,2,11 and the most used is the discard method. The latter consists of discarding a certain amount of blood prior to taking the sample, by aspirating a volume of blood in order to clean the catheter of intravenous solutions or medication and thus avoid contamination or dilution of the sample.3,11 This method involves a loss of blood in addition to that required for determining analytical parameters, especially in environments such as ICUs where a high number of extractions are performed daily.10
There are studies comparing different techniques for obtaining samples through a catheter. Byrne12 contrasts the discard with the push-pull technique; he concludes that the push-pull method is suitable for blood sampling, as it provides reliable laboratory results and reduces blood loss. Other authors have analysed blood conservation devices; these are closed circuits that allow blood to be taken for laboratory testing through a catheter without first having to discard a volume, eliminating unnecessary blood loss.13,14 Page et al., in a literature review, conclude that these devices reduce iatrogenic blood loss, lowering the risk of developing anaemia and possibly the need for transfusion.13 Ideally, the minimum amount possible should be discarded to avoid blood loss while obtaining a quality sample.
Our line of research is blood loss related to analytical extractions in the critically ill patient. In 2016, we made a diagnosis of the situation at the Hospital Universitari Son Espases. We asked ourselves whether in other ICUs the discard blood volume prior to analytical extraction was as relevant as that obtained in our study.2,10 The variability of healthcare practice with regard to collecting blood samples results in substantial differences in the interventions of healthcare professionals and may lead to adverse events, such as the onset of iatrogenic anaemia secondary to repeated extractions. Discard blood volume varies according to the characteristics of the catheter used, the analytical parameters to be studied, the infusions before and at the time of extraction, the technique used and the professional performing the technique.
ObjectivesTo analyse discard blood volume prior to collecting the sample through a vascular catheter in ICUs of the Balearic Islands.
To relate discard blood volume with the vascular catheter used, the experience of the professional performing the extraction and the hospital.
MethodologyDesign: descriptive, cross-sectional, and multi-centre study.
Scope and study period: study carried out in ICUs of the Balearic Islands, both public and private, from April to December 2018.
The population comprised 296 nurses who were working in adult ICUs at the time of data collection in this Autonomous Community. The sample size of 142 was calculated to obtain a 95% confidence interval, an accuracy of 3%, and an estimated loss of 15%.
Data collection instrument: an ad hoc questionnaire was prepared using Google Drive, thus facilitating automatic data collection. The survey consisted of 7 multiple choice questions and one open question (Appendix B annex 1). We contacted the supervisors of all the hospitals in the Autonomous Community beforehand to present the project. A formal invitation was made offering voluntary participation in the study. An information poster was then sent out with the objectives, scope of study, methodology, name, and affiliation of the researchers to disseminate together with the form. The supervisors distributed the survey asking for nurses' disinterested, anonymous, and voluntary collaboration. The data collection was carried out simultaneously in all the collaborating centres during the months of May and June. Once the data had been analysed, the results from each collaborating centre were sent to their supervisor.
Data analysis: IBM SPSS® Statistics 2 was used for the data exploitation. Descriptive statistical analysis, by calculating percentages, mean, median, interquartile range, standard deviation, coefficient of variation and confidence interval (CI). A bivariate analysis between groups was performed using non-parametric tests: Kruskal-Wallis and median test with 95% CI.
Ethical aspects: the study was approved by the hospital's research committee. The participants were considered to have given their consent to take part on completing the questionnaire that they were sent. Information associated with the occupation of the participants was collected, but never concerning their identity. The application used (Google Drive) guarantees the anonymity of participants by removal from the Internet Protocol. The questionnaires were anonymous and confidentiality was guaranteed at all times in accordance with the Organic Law of 13 December on the Protection of Personal Data 15/1999 and the Organic Law on the Protection of Personal Data and Guarantee of Digital Rights 3/2018, of 5 December.
ResultsThe hospital care network in our community consists of 14 adult ICUs distributed over the islands of Mallorca, Menorca, and Ibiza; 12 participated in the study, 6 public and 6 private. A total of 142 surveys were obtained and the response rate was 48%; 72.5% were women.
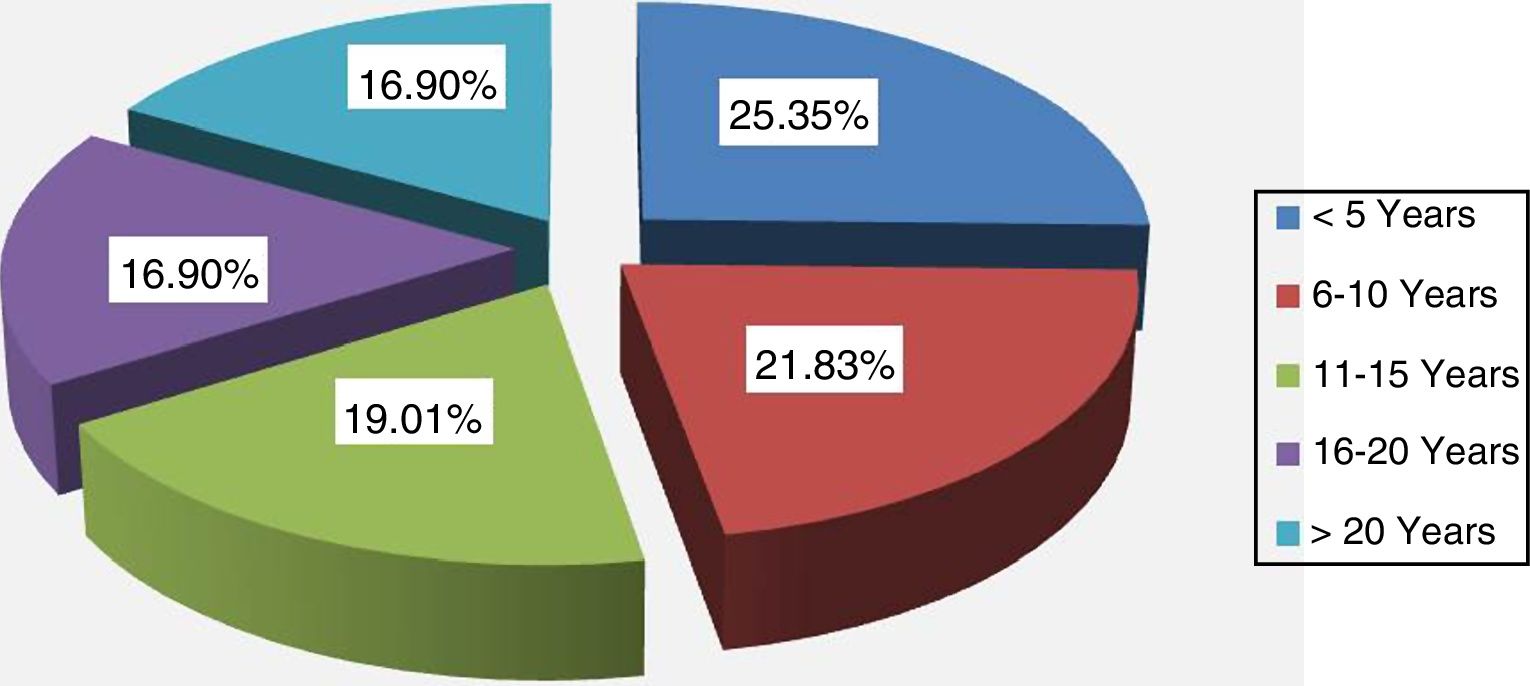
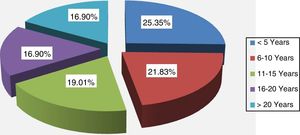
With regard to work experience, the majority group was <5 years (Fig. 1). Professional experience: more than 60% of the professionals working in public hospitals had professional experience >10 years, while in private hospitals the work experience was <10 years.
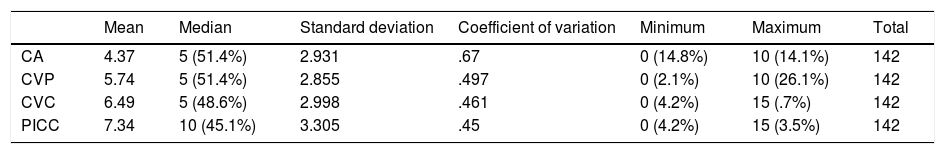
On analysing the results according to the type of catheter, the mean total volume was 5.98 ± 3.01 mL. The mean volume discarded (ml), the median, the standard deviation, the coefficient of variation and the range are shown in Table 1. The highest volumes corresponded to the CVC and PICC catheters with a mean of 6.49 ± 2.99 mL and 7.34 ± 3.30 mL, respectively. The medians in the AC, CVP and CVC were 5 mL, while in the PICC it was 10 mL. The ranges in AC and CVP were from 0 to 10 mL, and from 0 to 15 mL in the CVC and PICC.
Mean discard volume (ml) by catheter.
| Mean | Median | Standard deviation | Coefficient of variation | Minimum | Maximum | Total | |
|---|---|---|---|---|---|---|---|
| CA | 4.37 | 5 (51.4%) | 2.931 | .67 | 0 (14.8%) | 10 (14.1%) | 142 |
| CVP | 5.74 | 5 (51.4%) | 2.855 | .497 | 0 (2.1%) | 10 (26.1%) | 142 |
| CVC | 6.49 | 5 (48.6%) | 2.998 | .461 | 0 (4.2%) | 15 (.7%) | 142 |
| PICC | 7.34 | 10 (45.1%) | 3.305 | .45 | 0 (4.2%) | 15 (3.5%) | 142 |
No relationship was found between the sex variable and the amount of blood discarded: AC (p = .691), CVP (p = .909), CVC (p = .964) and PICC (p = .964).
No relationship was found between the sex variable and the amount of blood discarded: AC (p = .691), CVP (p = .909), CVC (p = .964) and PICC (p = .964).
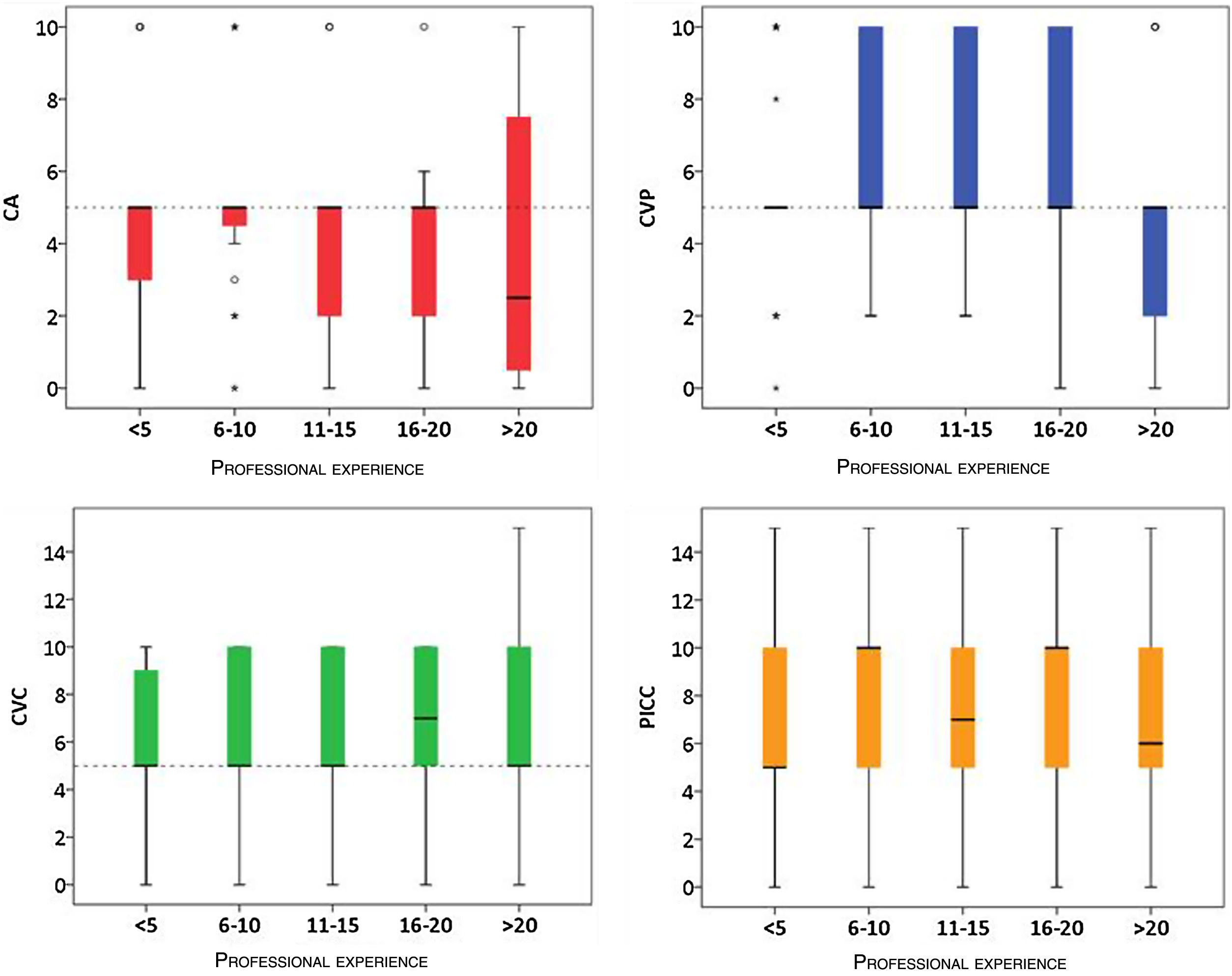
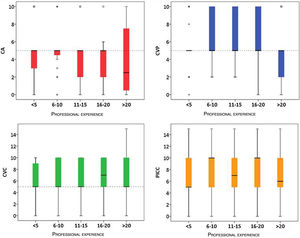
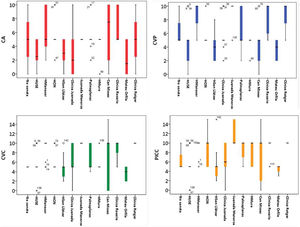
With regard to professional experience, no statistical relationship was found according to the catheter used: AC (p = .509), CVP (p = .598), CVC (p = .423) and PICC (p = .314). The median amount of blood drawn varied depending on the catheter used. Professionals with more than 20 years of experience discarded lower volumes in AC, the median being 2 mL, range 0−10 ml. In CVP the median was 5 mL, range 0−5 ml. In CVC, the median was 5 mL except in the 16–20 years group, which was 7 mL, the ranges were 0−10 in all groups, except in the >20 years group, which ranged from 0 to 15 mL. In PICC, the medians varied in each professional experience group, ranging from 0 to 15 mL in all groups (Fig. 2).
A low percentage of professionals used conservative techniques, in which the discard volume was equal to zero, 14.78% in the AC, 4.22% in the CVC, 2.11% in the CVP and 4.22% with the PICC.
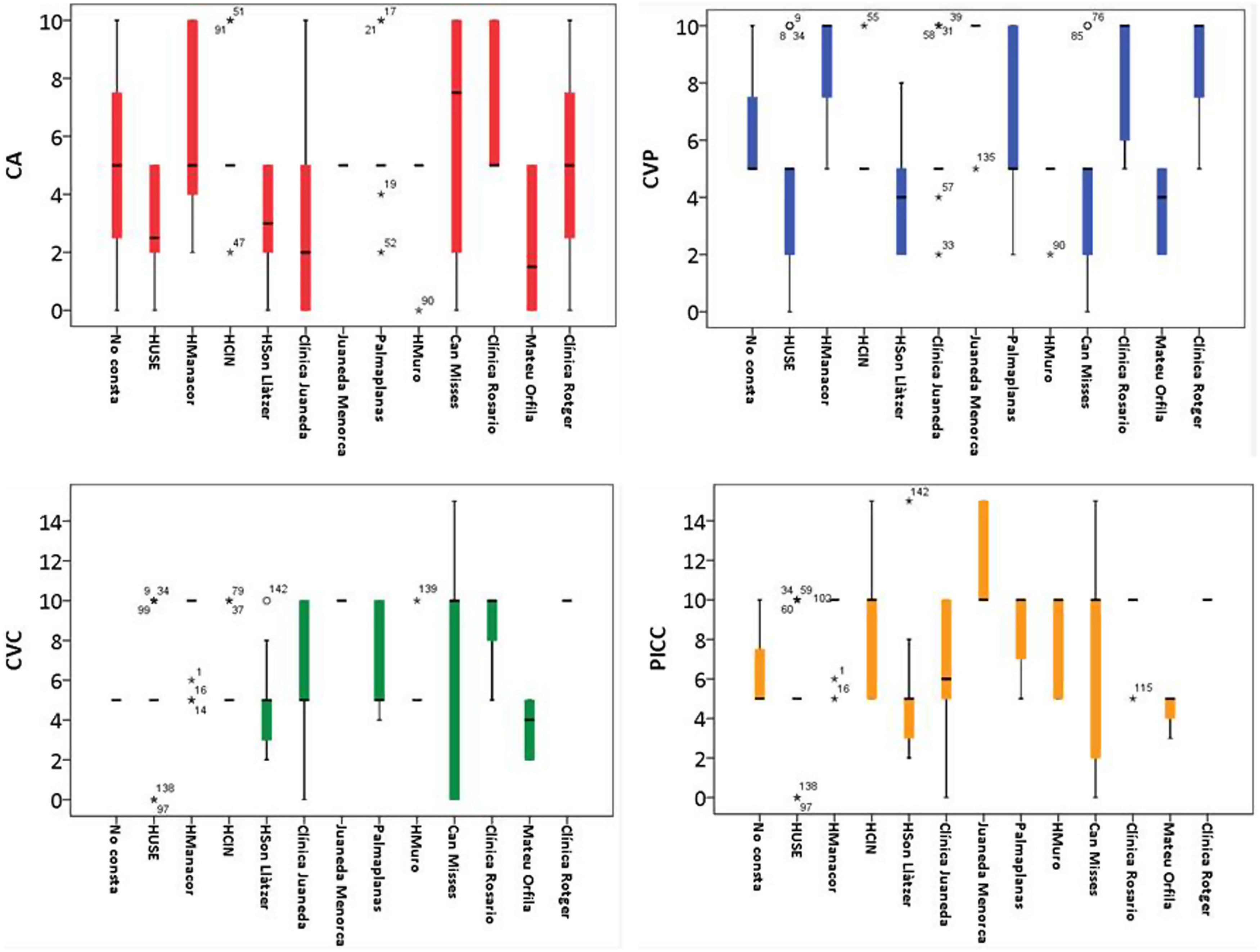
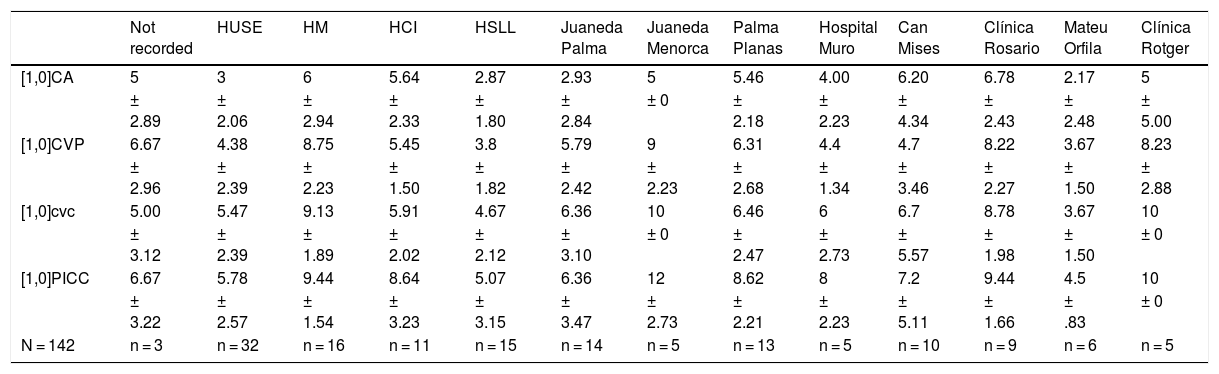
In relation to the centre where the extractions were performed, the results show that the hospital with the lowest discard volume was Hospital Mateu Orfila for all types of catheters (AC: 2.17 ± 2.17 mL, CVP: 3.67 ± 1.50 mL, CVC: 3.67 ± 1.50 mL, PICC: 4.50 ± .83 mL). Table 2 shows the mean and standard deviation of the discard volume (mL) according to the hospital and catheter used.
Mean discard volume (ml) by hospital.
| Not recorded | HUSE | HM | HCI | HSLL | Juaneda Palma | Juaneda Menorca | Palma Planas | Hospital Muro | Can Mises | Clínica Rosario | Mateu Orfila | Clínica Rotger | |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| [1,0]CA | 5 | 3 | 6 | 5.64 | 2.87 | 2.93 | 5 | 5.46 | 4.00 | 6.20 | 6.78 | 2.17 | 5 |
| ± 2.89 | ± 2.06 | ± 2.94 | ± 2.33 | ± 1.80 | ± 2.84 | ± 0 | ± 2.18 | ± 2.23 | ± 4.34 | ± 2.43 | ± 2.48 | ± 5.00 | |
| [1,0]CVP | 6.67 | 4.38 | 8.75 | 5.45 | 3.8 | 5.79 | 9 | 6.31 | 4.4 | 4.7 | 8.22 | 3.67 | 8.23 |
| ± 2.96 | ± 2.39 | ± 2.23 | ± 1.50 | ± 1.82 | ± 2.42 | ± 2.23 | ± 2.68 | ± 1.34 | ± 3.46 | ± 2.27 | ± 1.50 | ± 2.88 | |
| [1,0]cvc | 5.00 | 5.47 | 9.13 | 5.91 | 4.67 | 6.36 | 10 | 6.46 | 6 | 6.7 | 8.78 | 3.67 | 10 |
| ± 3.12 | ± 2.39 | ± 1.89 | ± 2.02 | ± 2.12 | ± 3.10 | ± 0 | ± 2.47 | ± 2.73 | ± 5.57 | ± 1.98 | ± 1.50 | ± 0 | |
| [1,0]PICC | 6.67 | 5.78 | 9.44 | 8.64 | 5.07 | 6.36 | 12 | 8.62 | 8 | 7.2 | 9.44 | 4.5 | 10 |
| ± 3.22 | ± 2.57 | ± 1.54 | ± 3.23 | ± 3.15 | ± 3.47 | ± 2.73 | ± 2.21 | ± 2.23 | ± 5.11 | ± 1.66 | ± .83 | ± 0 | |
| N = 142 | n = 3 | n = 32 | n = 16 | n = 11 | n = 15 | n = 14 | n = 5 | n = 13 | n = 5 | n = 10 | n = 9 | n = 6 | n = 5 |
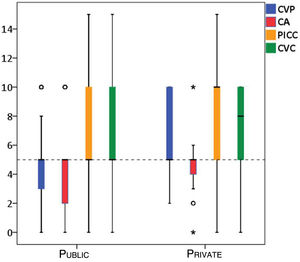
The median discard volumes between the ICUs of the different hospitals were very different (p < .001), as were the ranges. Fig. 3 shows the discard volume (ml) according to hospital and vascular catheter.
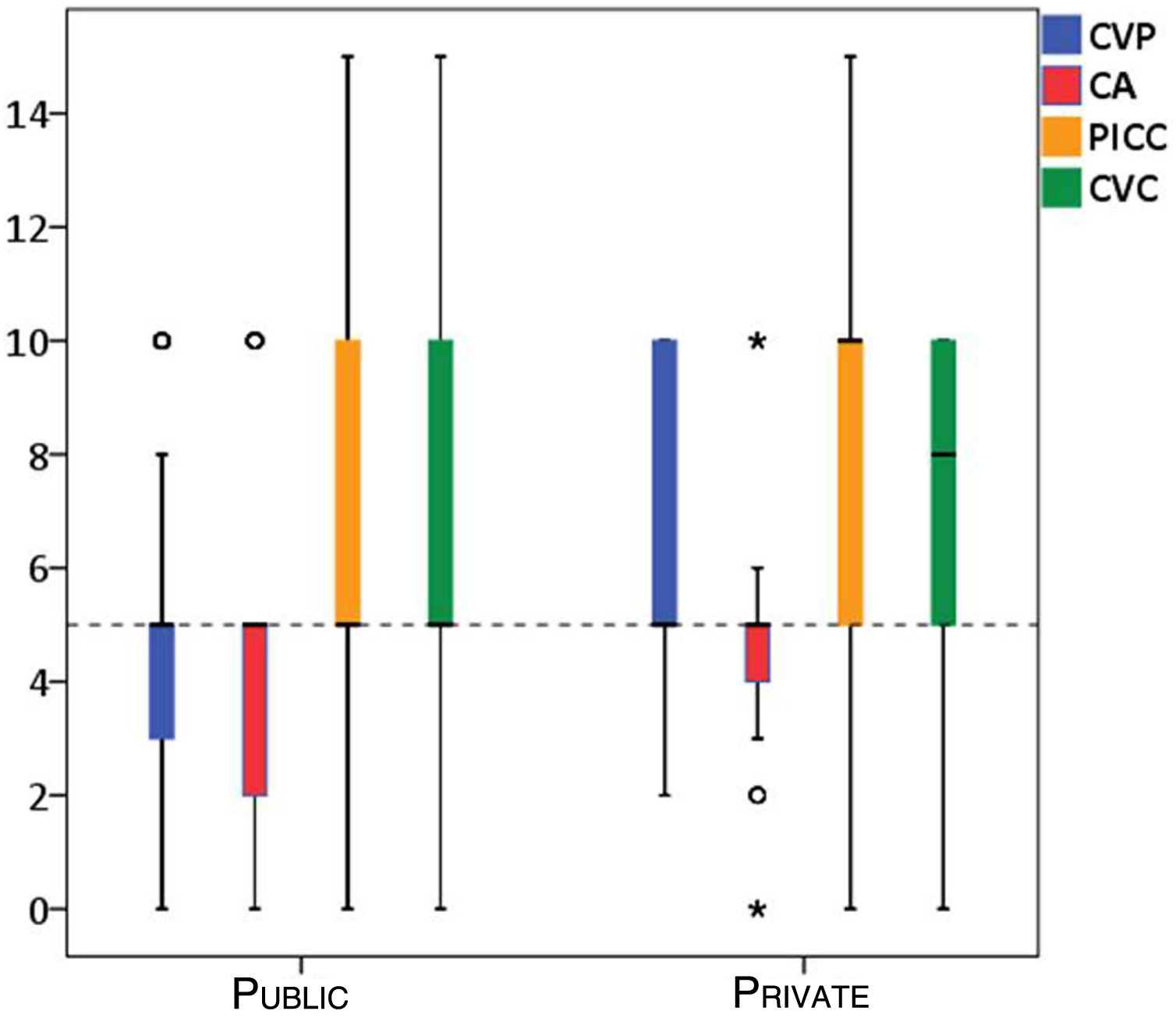
By grouping the hospitals into public or private, it was observed that the private hospitals discarded higher blood volumes than the public hospitals through CVP: 5.12 ± 2.15 mL vs. 6.99 ± 2.80 mL (p = .023), CVC: 5.92 ± 2.58 mL vs. 7.93 ± 1.71 mL (p = .026) and PICC: 6.77 ± 2.73 mL vs. 9.07 ± 2.05 mL (p = .004). In Fig. 4, it can be seen that the medians of all the catheters in public hospitals were 5 mL, while in private hospitals they were higher in CVC and PICC, as were the ranges.
DiscussionThe volume of blood discarded prior to obtaining samples through catheters was very inconsistent. The variables that influenced the volume discarded were the type of catheter used, the experience of the professional performing the technique and the hospital where the extraction was carried out. The Brazilian Society of Clinical Pathology and Laboratory Medicine for the collection of venous blood and the CLSI recommend discarding twice the volume of the dead space, i.e. the space between the intravascular end of the catheter and the port where samples are collected.3,4 This will depend on the catheter used and the length of the existing connections and extensions.
When analysing the results according to type of catheter, less blood was discarded when the extraction was done through arterial cannulas, followed by peripheral catheters, CVC and PICC. Discard volumes ranged from 0 to 15 mL. The most discarded volume was 5 mL, coinciding with the literature consulted.6,14 It was observed that the discard volume increased with longer catheters; this finding coincides with a study previously carried out in the ICU of the Son Espases University Hospital, in which the discard volume was compared with the type of catheter.2
In this study, the discard volume via AC ranged from 2.1 to 6.78 mL. Arias Rivera et al.15 carried out a comparative study of discard methods via AC; they concluded that 3 mL of discarded blood plus dead space is sufficient to obtain reliable results, except in the case of cephalin time, where they recommend 7.5 mL in addition to dead space, since they use pressurised systems with heparin for AC maintenance; however, they do not specify the dead space volume. Rickard et al.16 conclude that in order to obtain reliable results through AC it is sufficient to discard twice the dead space volume, between 2 and 4 mL. Tineo et al.17 corroborate the results of Rickard et al.,16 recommending discarding 2 mL, which in their study is equivalent to twice the dead space.
In CVPs, despite being small gauge catheters, the discarded volumes ranged from 3.67 mL to 9 mL, with 5 mL being the most discarded volume, higher than that recommended in the literature. Ortells-Abuye et al.5 compare the reliability of the results obtained from samples obtained through CVP vs. venipuncture. They conclude that there is agreement between most of the parameters studied, except for PCO2 and PO2, when the discard volume through CVP is 4 mL. Fincher et al.18 analysed the haemoglobin and potassium values in samples taken via CVP by discarding 3 mL before extraction vs. venipuncture; they found no difference in the results. Granados Gámez et al.19 compared samples extracted from CVP through which medication was administered discarding 3 mL beforehand and also obtained reliable results. Baker et al.20 conducted a similar study using 22 G-catheters; they report that 1 mL of discarded blood is sufficient to obtain reliable laboratory results.
For CVCs, average discard volumes ranged from 3.67 to 10 mL. The values recommended in the literature are also variable. Wyant and Crickman8 conclude that the optimal discard volume to avoid dilution or contamination is 9 mL in tunnelled catheters and 6 mL in CVCs. Cicolini et al.7 compare the analytical results obtained by venipuncture vs. previous discarding of 5 and 10 mL in CVC, in a sample of 20 patients without infusions and with continuous perfusions; they state that there are differences depending on the parameter studied, however, they do not explain whether the perfusions were stopped at the time of extraction. On the other hand, Villalta García et al.21 report that, in the blood samples taken from the proximal lumen of the 7 F triple-lumen central venous catheter, 20 cm in length, a discard volume of 2 mL without interrupting perfusions provides reliable results.
The PICC is the longest catheter with the largest dead space; mean discard volumes ranged from 4.50 mL to 12 mL. It was observed that this catheter has the greatest variability in discard volume. The results coincide with our previous study, this is the type of catheter where most is discarded, however, we have not found any further references in the literature.
If we analyse discard volumes by hospital, a great variability is observed, with discard volumes being higher in private hospitals.
It was observed that the professionals who worked in private centres and who responded to the survey had fewer years of professional experience than those who worked in public hospitals. A previous study related professional experience with discard volume, concluding that professionals with more experience tended to discard lower blood volumes.2 Perhaps this is why blood waste is higher in these hospitals.
The Infusion Nurses Society recommends, in order to reduce the amount of blood drawn and decrease blood volume due to phlebotomies, standardizing the procedure for taking blood, to avoid errors before the sample reaches the laboratory, to avoid unnecessary tests, to reduce the frequency of obtaining serial samples, to use smaller volume collection tubes, closed circuit systems without prior discard in venous and arterial lines, or the push-pull or mixing method to reduce the amount of discard to a minimum.1 Standardizing a minimum amount of discard could help reduce blood loss related to phlebotomy and decrease iatrogenic anaemia. Wyant and Crickman,8 in addition to standardizing discard volume, recommend using a checklist for obtaining blood samples.
The phenomenon of variations in practice can be observed from a population or individual perspective.22,23 From an individual perspective, patients with similar clinical situations are used to observe variability. There is a lot of clinical variability in discard volume prior to blood sampling. Even when working in the same setting, each professional uses different collection methods, including different instruments such as syringes or vacuum tubes of different sizes. Variability in clinical practice can have an impact on the quality of patient care, and therefore efforts should be made to unify criteria in clinical practice.
Within the limitations of this study, the low response rate obtained in May required the survey to be sent out again in June, thus extending the data collection time initially anticipated for the study. And even so, the response rate was lower than expected, which may have influenced the results obtained.
On the other hand, discard volume was studied without taking into account the extraction technique and whether there were protocols for obtaining blood samples in the collaborating centres, which may mean that discard volumes and the technique itself are protocolised and do not depend on the professional. In future studies it would be interesting to relate both variables to discard volume.
ConclusionsThere is great variability in the volume of blood discarded depending on the hospital where it is drawn. No statistical association was found between discarded blood and sex or professional experience, but there is a tendency for more experienced professionals to discard less blood. The discard volume from catheters is higher in private hospitals. All discard volumes were higher than those recommended in the literature, therefore there is room for improvement in all the centres investigated.
More conservative extraction techniques should be used to avoid iatrogenic anaemia. Standardizing clinical practice and adapting it to each institution would facilitate the phlebotomy process and ensure patient safety.
Conflict of interestsThe authors have no conflict of interests to declare.
We would like to thank all colleagues from the UCUs of the Balearic Islands for their participation in the data collection, and the supervisors for disseminating the project and questionnaire:
- -
José Vicente Val Pérez, Hospital Son Llatzer (Palma de Mallorca).
- -
Antonio Navas Ortega, Clínica Juaneda (Palma de Mallorca).
- -
Margui Torres Pons, Clínica Juaneda (Menorca).
- -
Rafael Santacasilda Caules, nurse supervisor of the ICU, Hospital Quirón Planas (Palma de Mallorca).
- -
Oscar Pérez Álvarez, Clínica Rotger (Palma de Mallorca).
- -
María García Montero, supervisor of the ICU of Policlínica Nuestra Señora del Rosario (Eivissa).
- -
Manuela Vila Rumbo, supervisor of the Intensive Care Unit of Hospital Can Misses (Eivissa).
- -
Juana María Gómez Arroyo, nurse at the Hospital Comarcal de Inca (Mallorca).
- -
José Luis Ferrer Perelló, Hospital Juaneda Muro (Mallorca).
- -
Hospital de Manacor (Mallorca).
- -
Ruth Fortuny Mercadal, Hospital Mateu Orfila (Menorca).
- -
Hospital Universitari Son Espases (Palma de Mallorca).
And Dr Juan Maria Raurich, for his unconditional support in the statistical analysis. Without all of the above this project would not have been possible.
Please cite this article as: Pérez-Juan E, Maqueda-Palau M. Análisis del volumen sanguíneo desechado para la extracción de analíticas en UCI. Enferm Intensiva. 2020;31:162–169.