The semirecumbent position is a widespread recommendation for the prevention of pneumonia associated with mechanical ventilation.
AimsTo identify the time of elevation of head of bed for patients under mechanical ventilation and the factors related to such elevation in an intensive care unit.
Materials and methodsAn observational, descriptive cross-sectional study. Conducted in an intensive care unit of a tertiary hospital from April to June 2015. The studied population were mechanically ventilated patients. Daily hours in which patients remained with the head of the bed elevated (≥30°), socio-demographic data and clinical variables were recorded.
Results261 head elevation measurements were collected. The average daily hours that patients remained at ≥30° was 16h28′ (SD±5h38′), equivalent to 68.6% (SD±23.5%) of the day. Factors related to elevations ≥30° for longer were: enteral nutrition, levels of deep sedation, cardiac and neurocritical diagnostics. Factors that hindered the position were: sedation levels for agitation and abdominal pathologies. Sex, age and ventilation mode did not show a significant relationship with bed head elevation.
ConclusionsAlthough raising the head of the bed is an easy to perform, economical and measurable preventive measure, its compliance is low due to specific factors specific related o the patient's clinical condition. Using innovations such as continuous measurement of the head position helps to evaluate clinical practice and allows to carry out improvement actions whose impact is beneficial to the patient.
La posición semiincorporada es una recomendación generalizada para la prevención de la neumonía asociada a ventilación mecánica.
ObjetivoIdentificar el tiempo de elevación de la cabecera de la cama del paciente sometido a ventilación mecánica y los factores del paciente relacionados con dicha elevación en una unidad de cuidados intensivos.
Material y métodosEstudio observacional, descriptivo y transversal. Realizado en una unidad de cuidados intensivos en hospital terciario, entre abril y junio de 2015. La población estudiada fueron pacientes con ventilación mecánica. Se registraron las horas diarias que los pacientes permanecían con el cabezal elevado (≥30°), datos sociodemográficos y variables clínicas.
ResultadosSe recogieron 261 mediciones de elevación de cabezal. La media de horas diarias en que los pacientes permanecieron a ≥ 30° fue de 16h28′ (DE±5h38′), equivalente al 68,6% (DE±23,5%) del día. Factores relacionados a elevaciones ≥ 30° durante más tiempo fueron: llevar nutrición enteral, niveles de sedación profunda, diagnósticos cardíacos y neurocríticos. Factores que dificultaban la posición fueron: niveles de sedación de agitación y patologías abdominales. Sexo, edad y modalidad ventilatoria no obtuvieron relación significativa en elevaciones de cabezal.
ConclusionesA pesar de que elevar el cabezal es una medida preventiva fácil de realizar, económica y medible, su cumplimiento es bajo, existiendo factores específicos del estado clínico del paciente relacionados con dicho cumplimiento. Utilizar innovaciones como la medición continua de la posición del cabezal ayuda a evaluar la práctica clínica y permite llevar a cabo acciones de mejora cuyo impacto sea beneficioso para el paciente.
PAMV is the ICU-acquired infection that has the highest rate of morbimortalidad. The semirecumbent position is a preventative measure against PAMV that is economical, easy to perform and measurable. Nevertheless, there is a low rate of compliance with this measure, which is recommended by national and international bodies. This work adds to the knowledge of healthcare staff on the factors related with raising the head of the bed of mechanically ventilated patients, describing the level of compliance based on national and international recommendations.
Implications of the studyTo identify compliance or failure to comply with the widespread recommendation to raise the head of the bed in case of mechanically ventilated patients, as well as associated factors, will make it possible to evaluate this practice and gain more in-depth knowledge of the phenomenon, while also establishing measures to improve it. This study also applies a new measurement methodology which takes the time the head is raised into account, increasing its accuracy regarding what is actually done with patients. Based on this study, it is also possible to detect the need for training or to increase knowledge about the specific preventative measures used in critical patient care.
Pneumonia associated with mechanical ventilation (PAMV) is the second most common hospital infection after urinary tract infection caused by the bladder catheter,1,2 and it is the most severe of the infectious complications that patients admitted to an intensive care unit (ICU) may suffer.3–5
Different scientific associations, groups of experts and healthcare agencies have analysed the methods that have proven to be effective in preventing the appearance of PAMV, and they have drawn up recommendations based on this2,6–8 in the form of packages of measures or “care bundles”. The preventative measure consisting of “raising the head of the bed” is common to all of these national and international guides and recommendations.2,6–9 They therefore indicate or recommend keeping the head of the bed of a mechanically ventilated patient at 30–45° to prevent aspiration of the stomach contents and/or oropharynx and thereby prevent PAMV. Even the Joint Commission recognised this as one of the core practices in the improvement of critical patient care.10
On the other hand, although many bodies agree on the need to keep the head of a ventilated patient's bed raised, fewer of them have openly published details of how to evaluate compliance with this measure. In Spain the SEMICYUC together with the SEEIUC drew up a document titled Quality Indicators.11 This states that the desirable standard level of compliance stands at 97% for the semirecumbent position (at an angle of 30° or more). The other body to have done so is the American Association of Critical-Care Nurses (AACN), which in “Practice Alert: ventilator associated pneumonia”6 states that if compliance with raising the head of the bed is at less than 90% of the sample, then plans for improvement must be prepared. In any case, based on proven scientific evidence the SEMICYUC as well as the AACN have agreed on similar standards of compliance, and they offer us tools so that we can evaluate our clinical practice.6,11
In spite of the recommendations there is a low level of compliance with the semirecumbent position, as is shown in many published works.10,12–16 Hiner et al.10 undertook a study to check on how nurses perceived a bed head angle of 30° or more in beds that do not automatically display the angle. Although 95% of the interviewees were aware of this preventative measure, approximately 50% of the nurses were unable to base their opinion solely on observation of the head of the bed, i.e., “at a glance”, to leave the head of the bed at a recommended angle, given that they underestimated it. This problem in calculating the height of the head of the bed now has a possible solution. Many critical patient units have beds that automatically measure the angle at which the head is raised. This is usually visible in the bedrails and therefore aid the nurse to keep to the recommended standard. However, many studies undertaken using this display on beds show that the contrary is the case. For example, Elorza Mateos et al.16 in a multipurpose ICU checked MV patient bed head angles 3 times a day. They found that in 76.4% of the checks the angle was lower than 30°, while the average elevation in all of the checks was 19.8° (SD 8.7°). Hanneman and Gusick,13 in a multicentre study in 9 ICU checked the heads of beds at certain times of day in the different nursing shifts and found that their average angle was 23° (SD 12°) for the patients with an orotracheal tube. In another multicentre study Rose et al.15 using 3 checks per day of MV patients obtained almost identical results to those of Hanneman et al., with an average elevation of the head of beds of 23.8° (SD 12.2°). On the other hand, Rose et al. state that the variables associated with a higher degree of bed head raising are patients fed through a nasogastric tube (NGT) and those in the weaning phase. The study by Lyerla et al.17 agrees with Rose et al. that higher elevations of the head of the bed were observed patients in MV with enteral feeding (EF), in the weaning phase or with a pulmonary diagnosis, although the standard was not attained in the majority of cases. Even so, we are able to think that having a NGT for EF could be a predictive factor for raising the head of the bed. However, Grap et al.18 found no significant differences between patients fed using a NGT or the type of NGT they were fitted with.
Another aspect on which studies differ is how data on bed head raising were gathered. Some of them make several observations per day, while others record the position continuously. Wolken et al.19 remark on how important this is in a study that compares cross-sectional cuts or intermittent observations with continuous records of bed head angle in an ICU with 24 beds fitted with automatic angle detectors in the bed rails. In cross-sectional or intermittent checks (recording the angle of bed heads once per shift) compliance is over-estimated in comparison with continuous records, at 25% more. I.e., intermittent measurements do not ensure that the heads of beds have kept at a certain angle during most of the day, given that there is not continuous measurement. Otherwise expressed, with the intermittent measurement method it is impossible to know the elevation of the head of a patient's bed between observations. In 2014 Del Cotillo and Valls Matarín14 made a continuous record of the angles of heads of beds using the automatic angle detector included in the beds of a multipurpose ICU. They found that the actual average time during which patients’ heads of bed were at or above an angle of 30° only amounted to 14h of the day (SD±5h), which is equivalent to 63% of the total day. This is closer to the real treatment of patients, and they underline that during one third of the day patients bed head are at an angle of below 30° for no justified reason.
The lack of adherence to this recommended standard is therefore surprising. Raising patients’ heads is a low-cost measure that is easy to implement, and the necessary material is available (beds with automatic angle indicators). When put into practice it reduces the risk for PAMV, especially those patients fed through a NGT.12,18,19 The chief aim of this study is to identify the length of time that the heads of beds of patients with mechanical ventilation are raised, and the factors associated with this elevation in a multipurpose intensive care unit.
Material and methodThis is an observational, descriptive and cross-sectional study, undertaken in a multipurpose 16 bed ICU in a tertiary hospital. Data were gathered from April to June 2015. This study was reviewed and approved by the Research Ethics Committee of the said hospital.
The study population was composed of the patients in the said unit who were subject to mechanical ventilation and complied with the following inclusion criteria: aged 18 years old or above and connected to MV for more than 24h. The exclusion criteria were: contraindication for raising the head of the bed by 30° or more, i.e., cases of prone position, unstable vertebral fractures, unstable pelvic fracture and/or contraindications due to the order of a doctor; patients who combined phases of MV disconnection; patients who at some time had left the ICU for procedures such as: complementary tests (CAT, magnetic resonance imaging, etc.) or for surgery (tracheotomy, to fit a pace maker, etc.); patients who sat in chairs; patients subjected to limited therapeutic effort who were expected to die immediately or within a few hours.
Non-probabilistic consecutive sampling was used to select the sample. The GRANMO20 program was used to calculate the sample size, based on the objective of elevation of the head of beds, giving rise to 259 observations.
The dependent variable was “compliance with the recommended elevation (≥30°) of the head of the bed”. Each observation recorded the hours of elevation of the head of the bed (in numerical format h:min per day).
The independent variables, including sociodemographic ones and those connected with the clinical situation of the patient were: age, sex, main medical diagnosis, type of MV, level of sedation (measured using the SAS21 scale, as this is the one used in the said) and enteral feeding (EF) (nutritional support for continuous infusion through a tube directly into the gastrointestinal tract). It has to be said that the level of patient sedation may change during the day, as may the type of MV (although less often), so that the SAS level which predominated on a day was recorded on the patient's record graph; likewise, the type of MV under which a patient passed the majority of the day was recorded.
An Excel-type spreadsheet notebook was prepared to record data, including independent variables and the dependent variable.
The time during which bed heads were raised was obtained from the data of the electronic screen included in the rail of the Hill-Rom® Total Care P1900 bed; all of the 16 beds in the unit correspond to this model. In the main rail, which contains an electronic screen, the bed software displays the exact degrees of elevation, although only the time is automatically recorded (in h:min format) during which the head remains raised at 30° or more; after 24h it starts to record again. The upper rail of the bed contains a transporter that is able to measure degrees of elevation from −15° to 80°; the value “30°” is marked more intensely and is used as a visual reference.
The data gathering procedure. To record the patient variables the data recorded in the graph associated with each patient were used, for sociodemographic data as well as their situation. The said data were taken from the graph of the previous day, and they were used to ensure that the patient fulfilled the set selection criteria, for example that they had not had to leave the unit for any complementary tests. During the data gathering period a single patient could be observed for several days, collecting data on their clinical situation as well as the duration of elevation of the head of the bed.
The software of the Hill-Rom® Total Care P1900 bed was used to measure the duration of elevation of the head of the bed, as this automatically records the time during which the head was raised at 30° or more in the h:min format. These data were recorded every 24h, so that it was possible to quantify the total number of hours per day that the head of the bed had been raised by ≥30°. Although other methods for observing the elevation of the head of the bed exist, such as the intermittent method, it was decided to use continuous measurement.
Data were gathered every day during the afternoon, and the data corresponding to the day before were always recorded. The main researcher (MR) was the only person who gathered data. During the data gathering period, the MR worked in the ICU as a nurse on the afternoon shift. To prevent distortion of the data, data from the patients under the care of the MR were excluded on the days the MR worked. During data gathering the MR did not reveal why the observations and data recording were undertaken, to restrict any bias arising from a possible modification in the usual established care practices. It should be pointed out that the MR has been a member of the “Respiratory insufficiency and MV” workgroup in the said ICU since 2008. This group, and therefore the MR in this study, undertakes different data gathering exercises throughout the year, one of which covers the raising of the heads of beds. The staff of the ICU studied are therefore familiar with this group, and direct or indirect observations of their clinical practice are therefore normal for them. The ICU studied has been a member of the Pneumonia Zero7 project since 2011.
Data analysisAbsolute and relative frequency were used to describe the qualitative variables. Quantitative variables were described using their average and standard deviation, or their average and a minimum and maximum.
The Mann–Whitney non-parametric test was used for bivariant analysis of the variables of sex, ventilation mode and the administration of EF by NGT, while the Kruskal–Wallis test was used for medical diagnosis and level of sedation. If the latter test was found to be significant, comparisons were undertaken according to categories using the Mann–Whitney test.
Finally multivariant analysis using lineal regression was performed, including the significant variables and the time at correct elevations as the response variable.
Statistical significance was considered to have been attained when P=<0.05.
Version 21.0 of the SPSS program was used to process and analyse the data.
ResultsA total of 261 measurements of bed head elevation were recorded.
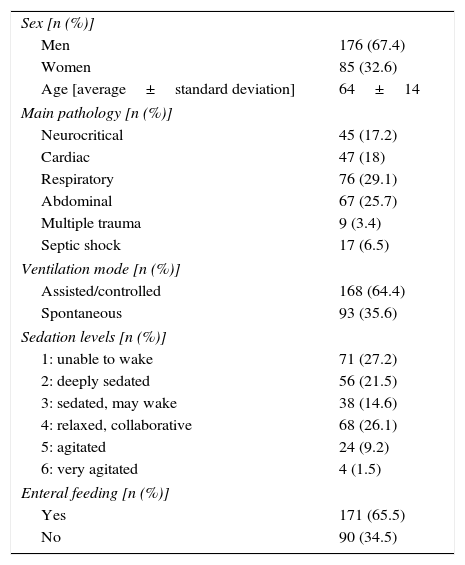
Table 1 shows the descriptive analysis of the observed variables. The medical diagnosis stands out here, as the majority of diagnoses involved pulmonary (29.1%) or abdominal (25.9%) pathology; more than half of the sample (64.4%) were in assisted/controlled ventilation mode (volume control, pressure control, pressure-regulated volume control). Another finding is that 65.5% of the study population were fed continuously by EF through a NGT. Although all of the other patients were fitted with a NGT, this was not used to feed them.
Characteristics of the study sample (n=261).
| Sex [n (%)] | |
| Men | 176 (67.4) |
| Women | 85 (32.6) |
| Age [average±standard deviation] | 64±14 |
| Main pathology [n (%)] | |
| Neurocritical | 45 (17.2) |
| Cardiac | 47 (18) |
| Respiratory | 76 (29.1) |
| Abdominal | 67 (25.7) |
| Multiple trauma | 9 (3.4) |
| Septic shock | 17 (6.5) |
| Ventilation mode [n (%)] | |
| Assisted/controlled | 168 (64.4) |
| Spontaneous | 93 (35.6) |
| Sedation levels [n (%)] | |
| 1: unable to wake | 71 (27.2) |
| 2: deeply sedated | 56 (21.5) |
| 3: sedated, may wake | 38 (14.6) |
| 4: relaxed, collaborative | 68 (26.1) |
| 5: agitated | 24 (9.2) |
| 6: very agitated | 4 (1.5) |
| Enteral feeding [n (%)] | |
| Yes | 171 (65.5) |
| No | 90 (34.5) |
The average number of hours per day that patients remained at ≥30° elevation of the head of their beds was 16h28′ (SD±5h38′). This is equivalent to 68.6% (SD±23.5%) of the total day.
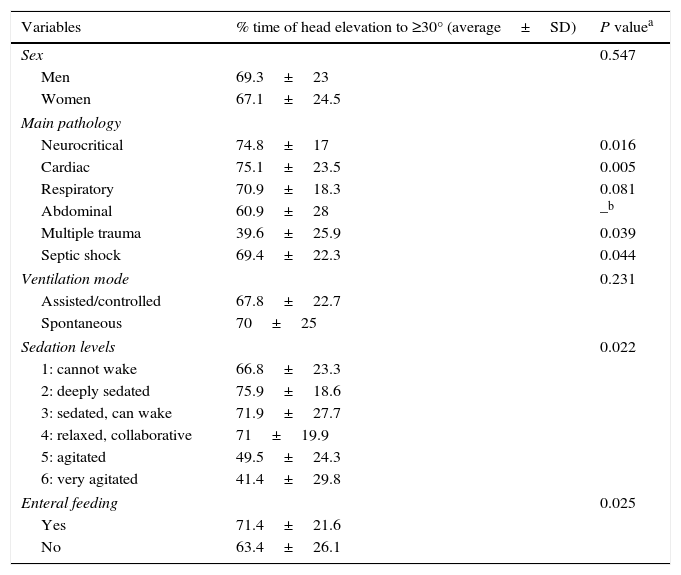
The bivariant analysis of the patient variables observed and elevation of the head of their bed is shown in Table 2. No significant differences were found according to patient sex. The average time that the heads of the beds of female patients was elevated to ≥30° was 67.1% of the total day, while for the men the corresponding figure was 69.3%. Nor was age associated with raising the head of the bed. Respecting medical diagnosis and bed head elevation, significant differences were only found for abdominal pathology and multiple trauma, as these were associated with a shorter time per day with correct elevation of the head of the bed. The pathologies in which the head of the bed was raised to ≥30° for the longest time were, in this order, cardiac, neurocritical and respiratory pathologies, without any significant differences between them. Ventilation mode led to no significant differences between groups: in spontaneous mode the patients spent an average of 70% of the day in elevations ≥30°, while in assisted or controlled mode the corresponding percentage was 67.8%. Lower levels of SAS, i.e., the most sedated patients, spent longer times in correct bed head positions. Significant differences were found between the extreme levels of SAS, i.e., between SAS 1 and 2 (cannot wake; deeply sedated) and SAS 5 and 6 (agitated; very agitated). There was also a significant difference between SAS 3 and 4 (sedated, can awake; relaxed, collaborates) and SAS 5 and 6. On the other hand, no significant differences were found between SAS 1 and 2 and SAS 3 and 4. Receiving EF continuously through a NGT was found to be a factor that significantly favours raising of the head of the bed in comparison with those patients with a NGT but who were not fed through it.
Association between patient factors and compliance with bed head raising.
| Variables | % time of head elevation to ≥30° (average±SD) | P valuea |
|---|---|---|
| Sex | 0.547 | |
| Men | 69.3±23 | |
| Women | 67.1±24.5 | |
| Main pathology | ||
| Neurocritical | 74.8±17 | 0.016 |
| Cardiac | 75.1±23.5 | 0.005 |
| Respiratory | 70.9±18.3 | 0.081 |
| Abdominal | 60.9±28 | –b |
| Multiple trauma | 39.6±25.9 | 0.039 |
| Septic shock | 69.4±22.3 | 0.044 |
| Ventilation mode | 0.231 | |
| Assisted/controlled | 67.8±22.7 | |
| Spontaneous | 70±25 | |
| Sedation levels | 0.022 | |
| 1: cannot wake | 66.8±23.3 | |
| 2: deeply sedated | 75.9±18.6 | |
| 3: sedated, can wake | 71.9±27.7 | |
| 4: relaxed, collaborative | 71±19.9 | |
| 5: agitated | 49.5±24.3 | |
| 6: very agitated | 41.4±29.8 | |
| Enteral feeding | 0.025 | |
| Yes | 71.4±21.6 | |
| No | 63.4±26.1 | |
The significant variables were considered last, and multivariant analysis was used for level of sedation, EF administration and the medical diagnoses of neurocritical, cardiological, respiratory, abdominal, multiple trauma and septic shock pathology. Lineal regression analysis showed that some variables disappeared from the model. As a result of this we found that on the one hand patients with abdominal pathologies and no EF remained in correct positions of head elevation for shorter times; on the other hand, the most heavily sedated patients remained in correct positions (≥30°) for longer.
DiscussionAnalysis of the results indicates that compliance with the recommended standard of “elevation of the head of the bed by from 30° to 45°” in MV patients is relatively low, and that specific factors about the clinical state of patients are associated with this practice, such as deep sedation or abdominal pathologies.
Compliance with the standard and the time patients remain in a semirecumbent positionThe SEMICYUC11 recommendation of “semirecumbent position in patients with MV” sets the standard at 97% compliance. Taking this reference into account, the level of compliance in our study population amounted to 68.7%, which can be said to be a long way from the recommended standard. If we take the reference of the AACN6 as the standard, we are not close to this level of compliance either, given that it recommended compliance with the measure in 90% of all the cases observed.
One fact that may justify this difference is that these standards are set on the basis of a certain way of gathering data and a formula for determining compliance that differs from the one just in our study. I.e., while these bodies state that they check head of bed elevation three times a day or at certain times of day, our study counts the hours per day during which the head of a patient's bed remains at ≥30°. These are therefore two different ways of determining compliance with head of bed elevation. As Wolken et al.19 point out, taking intermittent measurements overestimates compliance by about 25%. In this study it was decided to gather data continuously, as this seems to be closer to actual clinical practice. It is also the case that it was possible to use this data-gathering method as the unit was equipped with beds that had the necessary technology. Taking this exception into account, in other published studies that used the intermittent method low compliance with the standard was also detected, varying from 22% to 44% compliance for elevations of ≥30°.15–17,22,23 Thus although it does not attain the standards set by the SEMICYUC and the AACN, in this study the percentage of compliance is far higher than those detected in others.
In the 261 measurements made, patients were kept for an average of 16h28′ (SD±5h38′) per day with the head of the bed at an elevation of at least 30°. Only one study, by Del Cotillo and Valls Matarín14 was found that measured this using the same real time method. These authors also used a model of Hill-Rom® bed very similar to the one used in our study. In their 172 records they found an average of 14h (SD±5h) of patients who remained with the head of their beds elevated correctly, and these results are very similar to ours. In agreement with Del Cotillo et al., we found that patients did not fulfil the semirecumbent position recommendation during approximately one third of the day.
Elevation of the head of the bed and patient sex and ageNeither sex nor age are associated with the elevation of the head of the bed. Studies such as the one by Rose et al.15 find no relationship between patient age and the degree of elevation of the head of the bed.
Elevation of the head of the bed and receiving enteral feedingReceiving EF continuously through a NGT is a factor that is significantly associated with obtaining the recommended elevation of the head of the bed. Other previous studies also found that the heads of the beds of patients receiving EF are significantly more elevated. This may be due to the fact that nurses checking that the patient is receiving food makes them more aware of the risks of regurgitation and broncoaspiration, so that they increase the degree by which the bed head is raised. The study by Rose et al.15 is an example of this. It was a multicentre study with a sample of 2112 measurements, and it found that EF is one of the factors associated with increased raising of the head of the bed. The study by Lyerla et al.17 was carried out in an intensive care unit with a sample of 315 observations. It found that patients with some type of intubation for feeding had higher degrees of elevation. The recent study published by Llaurado-Serra et al.24 may also corroborate this. After distributing a specifically designed questionnaire among 67 nurses in 6 Spanish ICUs, it was found that EF is associated with compliance with the recommendation.
On the contrary, other studies found no significant relationships with EF, such as those by Grap et al.18 and Vinagre Gaspar et al.22 With samples of 502 and 553 measurements respectively, they both studied three areas of intensive care without finding any significant differences in the degree of compliance with the standard between patients with and without EF. Nevertheless, in both of these studies the patients receiving EF to elevated to higher degrees, although as Vinagre Gaspar et al.22 point out, this was hardly relevant in clinical terms.
Elevation of the head of the bed and the main medical diagnosisPatients with diagnoses associated with cardiac and neurocritical pathologies spent more time with the head of their bed at ≥30°, and there were no significant differences between these two groups. The recently published multicentre study of neurocritical patients by Llaurado-Serra et al.25 confirms that patients with an intracranial pressure monitoring catheter showed a significant increase in degrees of elevation of the head of the bed.
On the other hand, diagnoses associated with abdominal pathologies showed significantly fewer hours per day with the correct elevation of the head of the bed, so that this factor was found to hinder compliance with the recommended standard.
It is important to explain that patients with abdominal pathologies spent less time with the head of their bed raised, and that this finding is significantly associated with whether or not they were receiving EF. I.e., 67.2%(45) of the patients in the abdominal diagnosis category did not receive EF. On the contrary, 76.8% (149) patients in other categories did receive EF. These data agree with those of previous studies such as the one by Lyerla et al.,17 which found that patients with gastrointestinal diagnoses all had significantly lower elevations of the head of their bed.
Elevation of the head of the bed and level of sedationDeeper sedation, i.e., an SAS of 1–2 (unable to be woken, heavily sedated), has been shown to be a factor associated with spending longer with correct elevations of the head of the bed. The opposite is the case for an SAS of 5–6 (agitated; very agitated), which is a factor that significantly reduces head elevation. Levels of SAS 5–6 also differ significantly from SAS 3–4 (sedated, able to wake; relaxed, collaborative). However, no significant differences were found between SAS 1–2 and 3–4.
Few studies were found that connect level of sedation with the raising of the head of the bed. The recently published study by Llaurado-Serra et al.24 showed that agitation hindered compliance with the semirecumbent position. In this study the nurses also stated that other hindrances in attaining this position were patients being awake and describing the position as uncomfortable, or that some do not want the head of their bed to be at 30–45°. Qualitative studies such as the one by Cook et al.26 also describe how nurses identify several barriers against use of the semirecumbent position. One of these relates to patient safety when they are or may become agitated. This would give rise to the possibility of loss of access to the central venous catheter or sliding out of bed. In the study by Helman et al.23 the nurses express a series of concerns about the semirecumbent position, such as the possibility of patients sliding down to the bottom of the bed, patient comfort, their being unable to sleep and that turning patients may harm them, among others.
Due to all of the above considerations, it is logical for patients with an SAS 1–2 to have more possibilities of having a higher elevation of the head of their bed and for a longer time, as they are neither able to express discomfort and nor is there any danger of their exiting the bed. On the contrary, with an agitated patient or one who become so their safety is the priority for nurses, so they will keep them at a lower elevation of the head of the bed, while ensuring that they neither leave the bed nor lose their central venous catheter. It does not seem difficult for patients in SAS 3–4 who are awake and collaborative to remain in the correct position, unless they find it uncomfortable or it hinders them from sleeping.
Elevation of the head of the bed and ventilation modeThis study found that ventilation mode is not a factor that is significantly associated with raising the head of the bed. Nevertheless, the patients in spontaneous mode (PS or CPAP) spent a slightly longer average time elevated that did not in assisted or controlled mode (volume control, pressure control or pressure regulated volume control).
The findings of Vinagre Gaspar et al.22 are similar to ours. They compared patients connected to MV with T-intubed patients and found no statistically significant differences. Nevertheless, Rose et al.15 found that the weaning process is associated with greater elevation of the head of the bed, although they do not describe this process. The study by Cook et al.,26 which was based on interviews and focus groups, also found that higher elevations are more probable for patients in the process of weaning. Nurses may therefore place patients at a higher angle if they are in spontaneous mode or in the process of weaning, to favour lung expansion and breathing. In fact, the recent study published by Llaurado-Sera et al.25 confirms that in spontaneous ventilation modes or with T-tube there is significantly more compliance with the semirecumbent position.
The results of this study therefore show that compliance with the recommended standard of “elevation of the head of the bed to from 30° to 45°” for patients with MV is at a low level, and, as was pointed out, specific factors exist in the clinical state of patients which encourage or hinder this practice.
This study gives rise to new questions that should be investigated in the future. For example, which method for auditing bed head elevations best detects the actual situation in clinical practice with the instruments we now have? Are the results of intermittent checks comparable with those of the continuous method? On the other hand, a qualitative study is also required to examine nurses’ opinions on raising the head of the bed for patients with MV. Raising the head or not may be due to knowledge acquired with experience that is hard to express. It would be of interest to discover what underlies the said practice.
Study limitationsOne of the limitations of this study is that the data obtained cannot be extrapolated. They are taken from a single hospital and used a non-probabilistic sample. Nevertheless, these data do pertain to a multipurpose unit in a tertiary hospital that cares for multiple pathologies. Moreover, measurement of the elevation of heads of beds was continuous, and this is not possible in all hospitals.
ConclusionsRaising the head of a bed is simple to do, low cost and feasible in all critical care units. It is a preventative measure in PAMV that is nationally and internationally recognised and agreed. The nurses are mainly in charge of patient positioning and fulfilling the standard measure.
This study uses new measurement methodology that takes into account the length of time the head of a bed is raised, making it more accurate in describing actual practice with our patients. It would be positive for national and international bodies to establish an optimum rate for compliance with bed head elevation to ≥30° for 24h periods. It is important to work on this not only because electronic devices are becoming increasingly available, but also because they offer us better and more precise methods for evaluating the quality of care, implementing actions for improvement and for such actions to benefit patients.
We are sure that the innovations in hospital beds have only just commenced. Their design will improve as an instrument that helps to improve our clinical practice by offering better performance for patients as well as being research tools. Their use in this study is a good example of the latter.
As a final reflection, nursing care is crucial in preventing adverse effects for our patients while also offering them the maximum benefit, quality and safety during their hospitalisation. Together with training, research and the publication of results are strategies to continue improving patient care as well as the nursing profession. Nurses have to watch out for the innovations and opportunities which modern technology offers now, although it is even more important to form a part of this and becoming involved in it, knowing how to respond to the new needs of society.
Ethical disclosuresProtection of human and animal subjectsThe authors declare that no experiments in human beings or animals took place for this study.
Confidentiality of dataThe authors declare that they followed the protocols of their centre of work regarding the publication of patient data.
Right to privacy and informed consentThe authors declare that no patient data appear in this paper.
Conflict of interestThe authors have no conflict of interests to declare.
Please cite this article as: Martí-Hereu L, Arreciado Marañón A. Tiempo de elevación del cabezal de la cama del paciente con ventilación mecánica y factores relacionados. Enferm Intensiva. 2017;28:169–177.