The goal of this study was to assess the survival to hospital discharge in patients after the implementation of venoarterial-extracorporeal membrane oxygenation (VA-ECMO) during cardiopulmonary arrest (simultaneously or during the first six hours after the event) in a Spanish tertiary hospital.
MethodThis is a descriptive and retrospective study conducted with patients subjected to VA-ECMO therapy during or after cardiopulmonary resuscitation (CPR) in the last 10 years. The variables were extracted from the electronic medical record of each patient.
Results175 ECMO therapies were implemented, 84% (147) were VA-ECMO, and the indication for 17% (25) was CPR. In 40% (10), ECMO therapy was initiated simultaneously during CPR, and the rest (15) during the first six hours after the event. Survival rates reached 44%.
ConclusionsThe use of CPR in well-selected patients can improve their survival.
El objetivo del estudio fue analizar la supervivencia al alta hospitalaria de los pacientes tras la instauración de una membrana de oxigenación extracorpórea veno-arterial (ECMO-VA) en contexto de Paro Cardiorrespiratorio (simultáneamente o durante las 6 horas posteriores a ésta) en un hospital de tercer nivel español.
MetodologíaEstudio descriptivo y retrospectivo de los pacientes sometidos a una terapia ECMO-VA durante o tras maniobras de Reanimación Cardiopulmonar (RCP) en los últimos 10 años. Las variables fueron extraídas de la Historia Clínica electrónica de cada paciente.
ResultadosSe implantaron 175 ECMO, el 84% (147) fueron ECMO-VA y el 17% (25) su indicación fue durante o después de la RCP. De éstos últimos, el 40% (10) la terapia ECMO se inició simultáneamente durante las maniobras de RCP y el resto (15) en las 6 horas posteriores. Se obtuvieron tasas de supervivencia del 44%.
ConclusionesEl uso de la ECMO durante la RCP a pacientes bien seleccionados puede mejorar su supervivencia.
What is known/what does this paper contribute?
After more than 40 years of the systematic and standardised practice of cardiopulmonary resuscitation following cardiac arrest, results in terms of survival are still disappointing. The implementation of the ECMO system during or after cardiac arrest shows better survival results.
This study could contribute to the knowledge and dissemination of this technique in tertiary hospitals and ultimately improve the prognosis of patients during or after cardiac arrest.
Implications of the study?
There are currently few documents in Spain that reflect these advances and nurses have broad competences and are very much involved, not only in life support but also in establishing and managing ECMO systems. Therefore, we believe it is important to disseminate this study and its results.
IntroductionThe deployment of venoarterial-extracorporeal membrane oxygenation (VA-ECMO) therapy as salvage therapy in cardiopulmonary resuscitation (CPR) during in-hospital cardiopulmonary arrest (CPA) of cardiac origin, has been shown in observational studies to provide an up to 29% increase in survival when used simultaneously with CPR, in cases where a stable spontaneous rhythm is not achieved versus 12% if conventional CPR (without ECMO) is performed.1,2 According to the meta-analysis by Ouweneel et al.3 survival can be increased by up to 13% compared to conventional CPR.
Some studies also demonstrate the benefit of VA-ECMO therapy in patients in refractory cardiogenic shock post CPA with survival rates of up to 47% (VA-ECMO post CPR). These are patients who have recovered from a CPA who present a systemic picture of vasoplegia due to the post-reperfusion inflammatory response.4,5
In both clinical settings, the use of VA-ECMO provides complete circulatory and respiratory support and has the advantage that it can be deployed rapidly and percutaneously and at the bedside.1,6
VA-ECMO therapy in our setting is in full development and although there is extensive experience in the treatment of cardiogenic shock in Spain,5 there is little experience in the context of CPA.7
The aim of the present study was to analyse the survival to hospital discharge of patients after VA-ECMO in the context of CPA (immediate or in the 6 h following CPA) in a Spanish tertiary care hospital.
MethodDescriptive and retrospective study. The population comprised patients undergoing VA-ECMO therapy during (simultaneously) or after CPR manoeuvres (post CPR) in a tertiary level hospital in the last 10 years (2009–2018).
Patients who received extracorporeal mechanical ventilation therapy without membrane oxygenation were excluded.
In addition to their sociodemographic variables, we analysed patient origin, cannulation site, initial pre-ECMO diagnosis, time to implementation of the device, days of therapy and survival to hospital discharge. We also differentiated between patients who received ECMO during CPR and those who, after recovery from CPA, were in refractory cardiogenic shock within 6 h.
The variables were extracted from each patient’s electronic medical records, after the project had been approved by the hospital ethics committee.
The qualitative variables are presented as absolute frequencies (n) and percentages (%) and the quantitative variables as mean and standard deviation (SD). For statistical comparison between groups, the Student’s t-test was used for quantitative variables and the chi-squared test for qualitative variables. P-values equal to or less than .05 were considered statistically significant differences. SPSS for Windows version 21 was used for the statistical analysis.
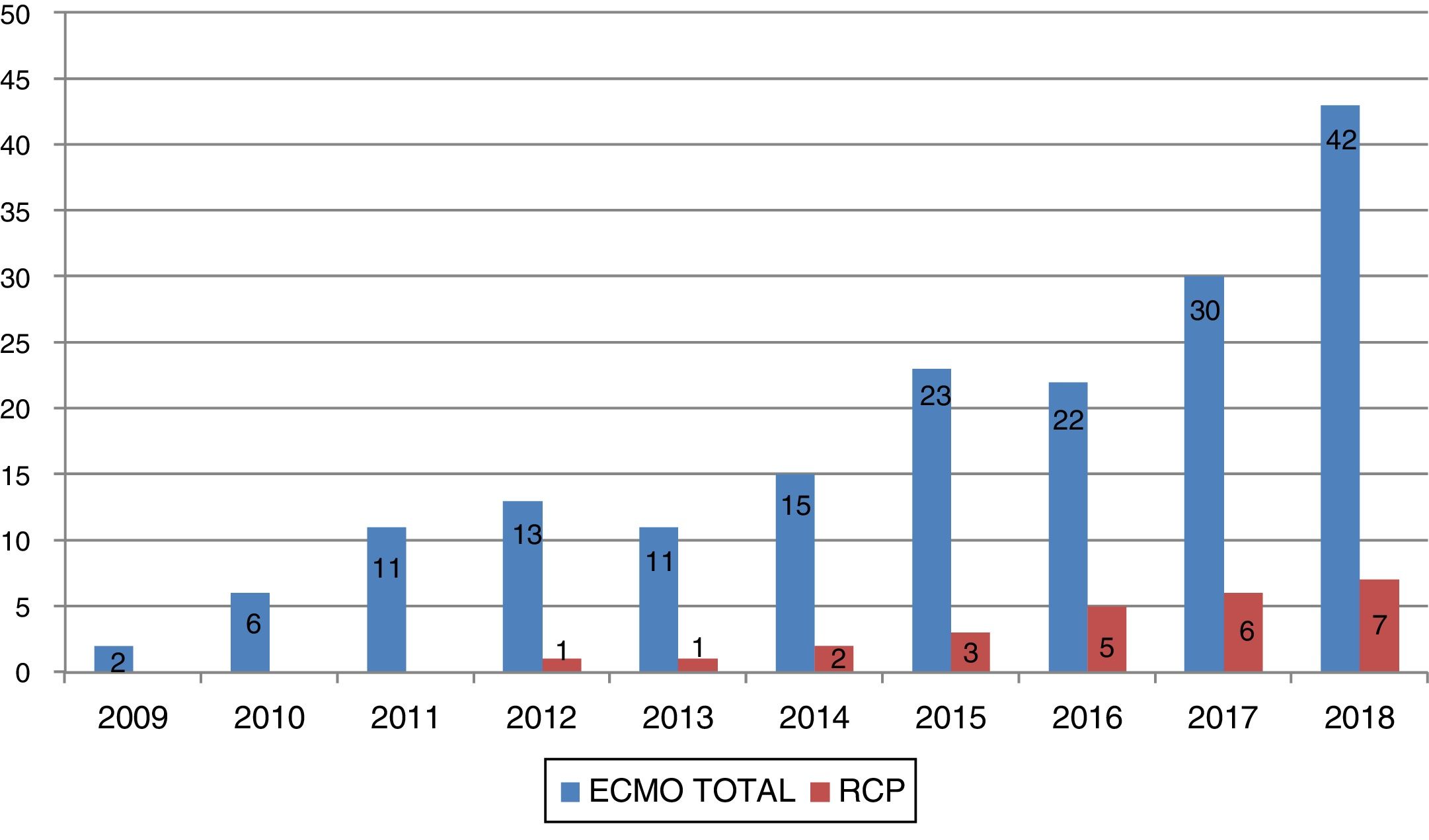
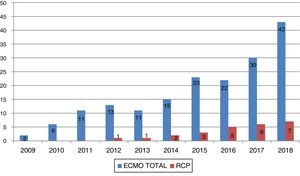
ResultsBetween January 2009 and December 2018, 175 ECMOs were implemented in the hospital, 84% (147) were VA-ECMO and of these, 17% (25) were indicated in the context of CPR (Fig. 1). In this paper we shall only analyse the data extracted from patients who underwent VA-ECMO during or after CPR.
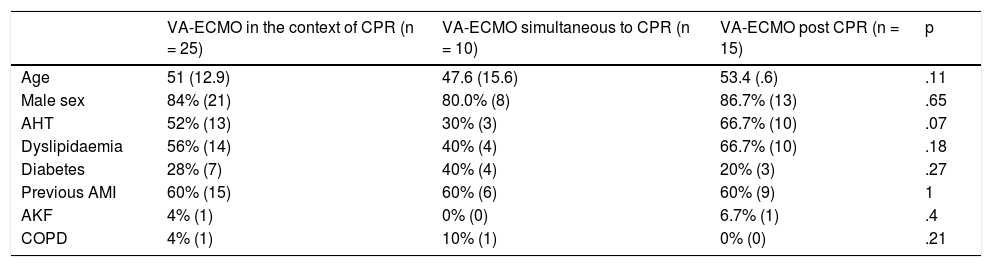
The mean age of these patients was 51 (12.9) years, 84% (21) were male and more than 50% were hypertensive and dyslipidaemic (Table 1 and Fig. 1).
Baseline data of the patients and their differentiation between groups.
| VA-ECMO in the context of CPR (n = 25) | VA-ECMO simultaneous to CPR (n = 10) | VA-ECMO post CPR (n = 15) | p | |
|---|---|---|---|---|
| Age | 51 (12.9) | 47.6 (15.6) | 53.4 (.6) | .11 |
| Male sex | 84% (21) | 80.0% (8) | 86.7% (13) | .65 |
| AHT | 52% (13) | 30% (3) | 66.7% (10) | .07 |
| Dyslipidaemia | 56% (14) | 40% (4) | 66.7% (10) | .18 |
| Diabetes | 28% (7) | 40% (4) | 20% (3) | .27 |
| Previous AMI | 60% (15) | 60% (6) | 60% (9) | 1 |
| AKF | 4% (1) | 0% (0) | 6.7% (1) | .4 |
| COPD | 4% (1) | 10% (1) | 0% (0) | .21 |
Values expressed in means (standard deviation-SD) and % (absolute frequencies).
AHT: arterial hypertension; AKF: acute kidney failure; AMI: acute myocardial infarction; COPD: chronic obstructive pulmonary disease.
The causes of CPA were acute myocardial infarction (AMI) in 60% (15), decompensation of previous cardiomyopathy in 20% (5), 4% (1) post-cardiotomy, 4% (1) after cardiac transplantation, and 12% (3) various aetiologies.
ECMO therapy was started simultaneously with CPR manoeuvres in 40% (10) and within 6 h in the rest (15). Table 1 shows the homogeneity of the groups in terms of sociodemographic variables and disease history, no statistically significant differences were found between them.
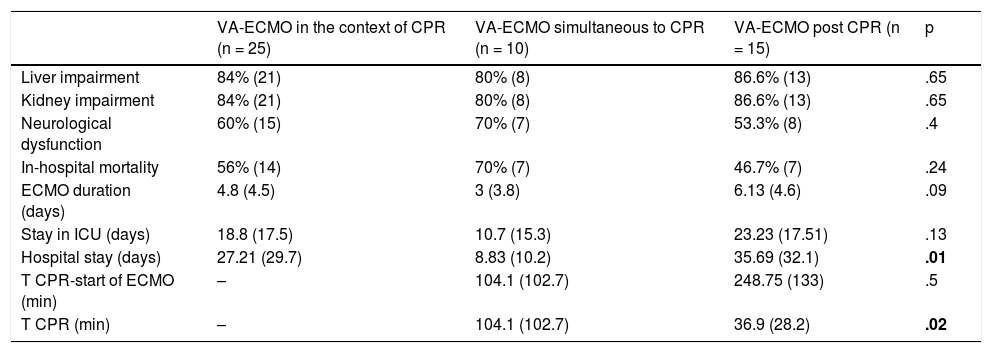
The total in-hospital mortality of the group was 56% (14) with a mean duration of VA-ECMO therapy of 4.88 (4.5) days, an intensive care stay of 18.85 (17.5) days and hospital stay of 27.21 (29.7) days (Table 2).
Clinical characteristics of patients undergoing ECMO during or after CPA, mortality, and results.
| VA-ECMO in the context of CPR (n = 25) | VA-ECMO simultaneous to CPR (n = 10) | VA-ECMO post CPR (n = 15) | p | |
|---|---|---|---|---|
| Liver impairment | 84% (21) | 80% (8) | 86.6% (13) | .65 |
| Kidney impairment | 84% (21) | 80% (8) | 86.6% (13) | .65 |
| Neurological dysfunction | 60% (15) | 70% (7) | 53.3% (8) | .4 |
| In-hospital mortality | 56% (14) | 70% (7) | 46.7% (7) | .24 |
| ECMO duration (days) | 4.8 (4.5) | 3 (3.8) | 6.13 (4.6) | .09 |
| Stay in ICU (days) | 18.8 (17.5) | 10.7 (15.3) | 23.23 (17.51) | .13 |
| Hospital stay (days) | 27.21 (29.7) | 8.83 (10.2) | 35.69 (32.1) | .01 |
| T CPR-start of ECMO (min) | – | 104.1 (102.7) | 248.75 (133) | .5 |
| T CPR (min) | – | 104.1 (102.7) | 36.9 (28.2) | .02 |
Values expressed in means (standard deviation-SD) and % (absolute frequencies). P values < .05 in bold.
T: time.
The in-hospital mortality rate of the 10 patients who received VA-ECMO during CPR was 70% (7), with a mean CPR time of 104 min until the device was deployed (Table 2). Of these, 40% died from post-anoxic encephalopathy, 30% from multi-organ failure and the rest from various causes.
The 15 patients who received VA-ECMO after recovery of stable cardiac rhythm (post CPR) had an in-hospital mortality rate of 46.7% (5), with a mean CPR time of 37 min and a time from start of CPR to start of VA-ECMO of 248 min (Table 2). Twenty percent of the patients died due to infection, 60% due to multi-organ failure and the rest due to various causes. No patient had severe post-anoxic encephalopathy.
All the patients had similar VA-ECMO duration (4.79 days for the deceased patients vs. 5.0 days for the survivors). However, the survivors had a shorter ICU stay (in days) than the deceased (10.6 vs. 27.1) and a shorter hospital stay (10 vs. 45.6).
DiscussionWe present the experience of a tertiary centre with a heart transplantation programme and extensive experience of more than 10 years in mechanical support therapies, including VA-ECMO, for the treatment of refractory cardiogenic shock. However, there is as yet no specific protocol for treatment with VA-ECMO as part of advanced CPR.
It is a technique that is increasingly implemented at hospital level,1,2,8 because it can be deployed at the bedside and the system’s technology has progressed to lighter and safer devices.9
As detailed below, survival in patients with simultaneous use of VA-ECMO during CPR is 30%, while the overall survival of patients on VA-ECMO in the context of CPR (simultaneous to CPR plus 6 h after CPR) is 44%; these are among the great variability of values included in published studies (between 7% and 57%)10,11 and comparable to the 29% survival rate reported by the ELSO.12 These are optimistic values if we compare them with conventional in-hospital cardiac arrest survival (without ECMO) which ranges from 15% to 22%.13 Therefore, we can cautiously recommend, like the international guidelines on CPR,14 that the use of VA-ECMO simultaneously with CPR (as a rescue alternative to advanced life support) in very well-selected patients may improve survival.
Our mean age was 51 years (22–68). These mean ages are lower than the 62 years reported by Mendiratta et al.,8 and nearer to the 54 years reported by Chonde et al.15
Our results show that the CPR times until implementing the ECMO system in the simultaneous CPR group are longer (104 min) than those recommended by Chen et al.1 (less than 30 min). Nevertheless, we obtained survival results similar to theirs (30%), in implementation times of between 30 and 60 min. These are acceptable results and show the potential of the therapy when a protocol that reduces reaction and action times is implemented. In the same group, the two predominant causes of death (post-anoxic encephalopathy and multi-organ failure) are to be expected in this scenario.15 Both could clearly benefit from a reduction in the time from CPA to starting VA-ECMO.
A survival rate of 53.5% was observed in relation to the results of the second group (post CPR), which is comparable to the 47% reported by Chonde et al.15 VA-ECMO therapy negates the detrimental effect of associated vasoplegia post CPA, reducing mortality due to the reversibility of the multi-organ failure established in these patients. The latter have significantly shorter CPR times than the simultaneous CPR group due to reversal of CPA, a longer time on ECMO-VA therapy, a longer stay in intensive care and a longer hospital stay, probably because these are patients with greater multi-organ involvement and a longer time in shock who require longer ECMO-VA times to reverse the damage.
The limitations of the study include its retrospective nature without a control group, the small sample size, and the fact that the cases recruited were obtained outside a specific protocol for this clinical situation. Nevertheless, we believe it very important to highlight this as a feasible and effective technique for the treatment of these two groups of patients who, if the therapy were not deployed, would have very high mortality.
In our opinion, these data provide us with a good starting point for structuring a VA-ECMO protocol for the treatment of refractory in-hospital CPA and the resulting refractory shock immediately post CPA. The protocol should be based on several premises according to the recommendations of societies and experts.15,16 It should be clear and help in the appropriate selection of the type of patient who can benefit from the therapy, it should provide a response in terms of the immediacy of activating the circuit as an integral part of advanced CPR. It should also have a specialist, trained team. All these aspects must result in the circuit being implemented within the 60 min following CPA.
We conclude that the thorough organisation of a structured VA-ECMO circuit for patients in cardiac arrest or once recovered and in cardiogenic shock can help to improve the survival of these patients.
Authorship/collaboratorsAll the authors of the manuscript participated in the research work and in drafting the article.
Each of the authors contributed substantially to the following aspects: in the conception and design of the study; in the acquisition, analysis, or interpretation of the data; in drafting the article or critical review of the intellectual content; and in the definitive approval of the final version.
The authors are developing a protocol for in-hospital ECMO during CPR based on the results obtained.
This was based on a thorough search and reading of the literature by all the authors.
The individual databases as collected by the different groups (nurses, perfusionists, cardiologists and cardiac surgeons) on patients undergoing ECMO therapy during CPR were combined. The candidate patients were selected (equally distributed among the authors), a data collection sheet was drawn up and data not previously collected were entered individually with the help of electronic medical records after authorisation from the hospital’s ethics committee.
Conflict of interestsThe authors have no conflict of interests to declare.
We would like to thank all the healthcare staff of the Hospital Universitario de Bellvitge involved in the care of critical patients undergoing ECMO therapy.
Please cite this article as: Castillo García J, Sánchez Salado JC, Gual Santandreu M, Molina Mazón CS, Blasco Lucas A, Sbraga F, et al. Supervivencia al alta hospitalaria de los pacientes sometidos a terapia ECMO tras PCR en un hospital de tercer nivel. Enferm Intensiva. 2021;32:73–78.