The SARS-CoV-2 vaccination program campaign has been underway in Indonesia for people aged ≥18 years. The program’s success can be hampered by vaccine hesitancy in communities. This study aims to elucidate the determinants of SARS-CoV-2 vaccine hesitancy in a rural area of the Indonesia–Philippines border island Sangihe.
MethodsA mixed-methods study was conducted; a quantitative part involving a cross-sectional survey was carried out among participantes aged ≥18 years to determine the prevalence and determinants of SARS-CoV-2 vaccine hesitancy. The qualitative part involved in-depth interviews to explore the perceptions towards the SARS-CoV-2 vaccine.
ResultAmong 557 participantes, the prevalence of vaccine hesitancy was 63.9% (95% CI: 59.8–67.9). In the adjusted analysis, three factors affected vaccine hesitancy: education (aOR: 0.40; 95% CI: 0.22−0.70), knowledge of the SARS-CoV-2 vaccine (aOR: 2.17; 95% CI: 1.41–3.34) and willingness to pay (aOR: 0.12; 95% CI: 0.07–0.20). The majority of reasons for refusing the vaccine included doubt regarding its safety and effectiveness, the fear of side effects, lack of information regarding the vaccine and local Christians’ religious beliefs.
ConclusionThis study found that most adults in the area were hesitant about the SARS-CoV-2 vaccine. Lack of knowledge, a low level of education and misinformation were factors that greatly affected vaccination hesitancy. The government, by involving religious leaders, is expected to pay serious attention to the dissemination of accurate and convincing information to the public regarding the safety and importance of the SARS-CoV-2 vaccine.
La campaña de vacunación contra la infección por SARS-CoV-2 se viene desarrollando en Indonesia para personas ≥ 18 años. El éxito de este programa puede verse obstaculizado por la presencia de dudas sobre las vacunas en las comunidades. Este estudio tiene como objetivo identificar los determinantes de la indecisión en relación a la vacunación por la infección por coronavirus en una zona rural de la isla fronteriza entre Indonesia y Filipinas.
MétodosEstudio de métodos mixtos realizado con una parte cuantitativa que incluye una encuesta transversal realizada entre participantes de ≥ 18 años para determinar la prevalencia y los determinantes de la indecisión en relación a la vacunación contra la infección por SARS-CoV-2. La parte cualitativa consistió en entrevistas en profundidad para explorar la percepción hacia la vacuna contra la infección por SARS-CoV-2.
ResultadoEntre 557 participantes, la prevalencia de indecisión ante la vacuna fue del 63,9% (IC del 95%: 59,8–67,9%). En el análisis ajustado, hay 3 factores que inciden en la indecisión ante la vacuna, a saber, educación (ORa: 0,40; IC 95%: 0,22–0,70), conocimiento de la vacuna, infección por coronavirus (ORa: 2,17; IC 95%: 1,41–3,34) y disposición a pagar (ORa: 0,12; IC del 95%: 0,07–0,20). La mayoría de las razones para rechazar la vacuna incluyen la duda de su seguridad y eficacia, el temor a sus efectos secundarios, la falta de información sobre la vacuna y el factor de la creencia religiosa cristiana.
ConclusiónEste estudio encuentra que la mayoría de los adultos en zonas rurales dudan sobre la vacuna. La infección por coronavirus, la falta de conocimiento, el nivel de educación y la desinformación son factores que afectan en gran medida a la aceptación de la vacunación por parte de una persona. Se espera que el gobierno, al involucrar a los líderes religiosos, preste mucha atención a la difusión de información precisa y convincente para el público sobre la seguridad e importancia de la vacuna contra la infección por coronavirus.
The existence of vaccine hesitancy has been known in several urban areas. In India was 14.1% and in Indonesia was 33%.
What does it contribute?The majority the previous studies used cross-sectional study design. The design of this study produces more comprehensive data because it explores the reasons for doubt/refusal to vaccination so that it can provide recommendations for targeted interventions as a way to increase the coverage of COVID-19 vaccination.
The COVID-19 pandemic, caused by the SARS-CoV-2 virus, is still a Public Health Emergency of International Concern (PHEIC). The Indonesian government has been attempting to control the spread of infection by providing vaccines.1 The data as of July 5th 2021 showed 3197 M doses of COVID-19 vaccines have been administered across 215 countries (including Indonesia), areas, territories and economies.2
In Indonesia, the goal is to vaccinate 181 million Indonesians to achieve herd immunity in populations 18 years and over.3 The targeted immunization rate can be hampered by the presence of vaccine hesitancy among communities. Vaccine hesitancy is the delay in vaccine acceptance or refusal of vaccination despite the availability of vaccination services.4
Vaccine hesitancy is a worldwide phenomenon. A cross-sectional study on COVID-19 vaccine hesitancy among caregivers from the USA, Canada, Israel, Spain, Japan and Switzerland showed its prevalence to be 35% (95% CI = 32–37).5 In concordance, the prevalence of Measles Rubella (MR) vaccine hesitancy varied from 14.1% in India to 33% in Indonesia.6,7 A recent study in urban area of Indonesia, also found a 35,2% of vaccine hesitancy.8 However, the results of these studies cannot represent rural areas in Indonesia.
There has been limited research on the determinants and prevalence of vaccine hesitancy in rural areas using a mixed method. Sangihe Island is one of the outer islands of Indonesia, which is directly adjacent to the Philippines. As an island that constitutes mostly rural areas, it must be prioritised in handling the pandemic due to various limitations, including limited access to health services, limited information and a middle-average income (IDR 2.69 million per person per month).9 Meanwhile, the number of COVID cases in North Sulawesi reached 15,670, of which 313 were in the Sangihe Island.10 Therefore, this study aims to comprehensively determine the prevalence and determinants of the SARS-CoV-2 vaccine hesitancy. The results of this study can inform governments’ and decision makers’ policies regarding the SARS-CoV-2 infection vaccination program in Indonesia, which is an archipelagic country, and other countries in Southeast Asia that have the same characteristics.
MethodsDesignThis study uses a sequential explanatory mixed-method approach, which is a method that combines quantitative and qualitative data where the qualitative data aims to expand and deepen the results of the quantitative data.11,12 Quantitative data were collected using cross-sectional data collection. Meanwhile, qualitative data were collected through in-depth interviews to explore information about people’s perceptions of the SARS-CoV-2 vaccine.
Population and study settingThe study was conducted on an Indonesian-Philippines border island called the Sangihe Island of North Sulawesi. Residents mostly live in rural areas. This island is a district with 15 sub-districts that has a population of approximately 130,000 people. There are two public hospitals, and the referral hospital is a provincial-level hospital 10 h away by motorboat. At the time of the study, a vaccination program for health workers followed by educators and the general population was in progress.
Quantitative data collection targets were adult residents (aged ≥18 years) of Sangihe Island, and the samples were recruited from across the 15 sub-districts. Those who worked in health sectors were excluded from this study. Quantitative data collection was conducted from 16 February 2021 to 28 February 2021. The study was conducted after the Sinovac vaccine was available in Indonesia, which showed an efficacy of 65.3%.13
The sample calculation used a sample size formula for estimating proportion, namely n = Z1-α/2 P(1-P)/d,2,14 where the P-value is the proportion of vaccine acceptance from previous studies in Indonesia, namely 64.8% (P = 0.65). The value of d (acceptable standard deviation) was 5% (d = 0.05), and a 95% confidence degree (Zα = 1.96) showed the total value of N = 350 samples. To adjust for the sampling method, a design effect of 1.5 was used, and the final sample size was 525. Snowball sampling was used for quantitative sampling. Priority for participation was given to the population in sub-districts geographically spread out and easy to reach.
In the qualitative phase, we interviewed at least 30 adult citizens from five sub-districts. The samples (participants) were selected using a purposive sampling technique. The research instrument was the researcher himself who used an interview guide. The questions in the interview guide aimed to find out the public’s perceptions regarding the SARS-CoV-2 vaccine and the reasons why they accepted/rejected the vaccination. Qualitative data collection was conducted from 1 March 2021 to 14 March 2021.
VariablesTo assess respondents’ perceptions of the SARS-CoV-2 vaccine, respondents were asked questions about their willingness to be vaccinated. The answers ‘hesitate/refuse’ or ‘accept’ and the reason if the answer was ‘hesitate/refuse’ were gathered. Several explanatory variables were also collected through questionnaires. Specifically, these were socio-demographic variables, such as age, gender, education, occupation, religion, marital status, source of information on the vaccine, income, willingness to pay and economic status. Economic status was categorised as ‘poor’ for those living below the national poverty line, or around IDR 354,000 per person per month; as ‘vulnerable’ for those living above the poverty line but with a non-negligible risk of falling into poverty, or between IDR 354,000 and IDR 532,000 per person per month; as ‘aspiring middle class’ for those no longer living in poverty or vulnerability but who are not yet economically secure, or between IDR 532,000 and IDR 1.2 million per person per month and ‘middle/upper class’ for economically secure Indonesians with little chance of falling into poverty or vulnerability, or more than IDR 1.2 million per person per month.
Another variable is the knowledge variable related to the SARS-CoV-2 vaccine, which was assessed using 15 questions. Participants with 60% or more correct answers were categorised as having ‘good knowledge’, and participants with fewer than 60% correct answers were categorised as having ‘poor knowledge’.
Data collectionThe quantitative research instrument used was a questionnaire taken from previous research and validated.8 The enumerator distributed questionnaires to the first group of participants via social media, a WhatsApp group and email. Next, the first group was asked to distribute the link of questionnaires to the second group and so on. Once a participant opened the questionnaire link, they filled in the informed consent or willingness to become a participant. For people who did not have internet access, questionnaires were distributed in hardcopy, and the enumerator asked for the willingness of participants to continue to carry out their health protocols due to the pandemic.
Internal validity was maintained by enforcing good data management practices. Each participant had a unique ID to prevent double counting. It was unlikely that one participant filled out the questionnaire two times (offline and online) because the offline questionnaire was only for those who did not have internet access. Data collection was carried out using non-probability sampling so that it could not guarantee the representation of the entire population on one island (district). However, the sample came from all existing sub-districts.
The qualitative research instrument was an interview guide for in-depth interviews. The questions in the guide aimed to find out people’s perceptions regarding the SARS-CoV-2 vaccination. The research instrument was the researcher using interview guidelines.
The interviewer had a postgraduate degree with experience conducting qualitative research in the health sector. The interviewer was also a resident in the research community who understood the local language and customs. The interview began after obtaining approval by explaining the purpose and motive of the study. Each interview took at least 45 min–30 min for exploring the participants’ perceptions of vaccination and 15 min for the introduction. The privacy of informants was maintained by conducting interviews in a special room without the presence of non-participants. All information provided by the informant was kept strictly confidential. All interview processes were recorded with the participants’ consent. Field notes were taken during interviews. At the end of the interviews, a summary was presented to the participants for the validation of the data collected. Transcription was carried out using a verbatim format within 2 days of data collection to prevent information loss. The interviewer's relationship with the participants was equal.
Data analysisData analysis for the quantitative phase was conducted using a logistic regression model to clarify the determinants of SARS-CoV-2 vaccine hesitancy. The first step was to perform a bivariate (chi-squared) analysis to select a candidate as the independent variable. Associations between explanatory variables and vaccine hesitancy were analysed separately. In the second step, all variables with a P-value ≤0.25 (age group, education, occupation and marital status) in the first step were included in the adjusted analysis. The crude odds ratio (OR) and adjusted odds ratio (aOR) in the multivariate analysis were assessed at α = 0.05 with a 95% confidence interval (95% CI). All statistical analyses used SPSS software (25th version, International Business Machines Corp., New York).
Data analysis for the qualitative phase was carried out using the Colaizzi method. We conducted triangulation to maintain the validity of the data. Triangulation was carried out by more than one researcher in analysing and collecting data to avoid researcher subjectivity. In addition, the researchers did member checking by validating the data from participants.
Ethical considerationsThe protocol of this study was approved by the Health Research Ethics Committee of Manado Health Polytechnic, Ministry of Health (KEPK.01/02/008/2021). All participants were informed of the purpose of this study and were asked to provide their informed consent. All personal information was kept confidential and not reported in this paper.
ResultsQuantitative partA total of 584 people aged 18–89 years participated in this study; 19 respondents worked as health workers, and 8 respondents who did not complete the questionnaire were completely excluded from the research data. The total number of respondents included was 557 (95.3% response rate).
The prevalence of SARS-CoV-2 vaccine hesitancy was found to be 63.9% (95% CI: 59.8%–67.9%). Table 1 shows the association between socio-demographic characteristics and vaccine hesitancy. In the first step (before the adjustment), there were three variables that were significantly related to vaccine hesitancy: education, knowledge towards the SARS-CoV-2 infection vaccination and willingness to pay. After the adjustment, the results showed that respondents with a diploma/university education were less likely to hesitate to get vaccinated compared to those with a primary/junior high school education (aOR: 0.40; 95% CI: 0.22–0.70). Those who were senior high school graduates were less likely to be hesitant about the vaccine compared to those who were primary/junior school graduates (aOR: 0.32; 95% CI: 0.14–0.73). Respondents who had poor knowledge of the SARS-CoV-2 vaccine were 2.17 times more hesitant to get the vaccine compared to those who had good knowledge of the vaccination (aOR: 2.17; 95% CI: 1.41–3.34). Those who had a willingness to pay were likely less hesitant to get the vaccine compared to those who were not willing to pay (aOR: 0.12; 95% CI: 0.07–0.20). Other variables were not significantly associated with vaccine hesitancy (Table 1).
Factors associated with COVID-19 vaccine hesitancy in a rural area of Indonesia–Philippines Border (Sangihe Island).
| Variable | n (%) | Hesitancy n (%) | Unadjusted | Adjusted | ||
|---|---|---|---|---|---|---|
| OR (95% CI) | P-value | aOR (95% CI) | P-value | |||
| Age group (year) | ||||||
| 18–25 | 239 (42.9) | 174 (72.8) | 1 | 1 | ||
| 26–35 | 126 (22.6) | 74 (58.7) | 0.67 (0.28–1.59) | 0.366 | 0.601 (0.26–1.35) | 0.217 |
| 36–45 | 55 (9.9) | 23 (41.8) | 0.895 (0.44–1.78) | 0.751 | 0.765 (0.39–1.47) | 0.424 |
| >45 | 137 (24.6) | 85 (62.0) | 1.692 (0.74–3.82) | 0.206 | 1.438 (0.65–3.16) | 0.367 |
| Education | ||||||
| Primary/junior school | 99 (17.8) | 79 (79.8) | 1 | 1 | ||
| Senior high school | 276 (49.6) | 202 (73.2) | 0.282 (0.12–0.65) | 0.003 | 0.32 (0.14–0.73) | 0.007 |
| Diploma/university | 182 (32.7) | 75 (41.2) | 0.406 (0.22–0.73) | 0.003 | 0.40 (0.22–0.70) | 0.001 |
| Occupation | ||||||
| Civil servant | 96 (17.2) | 32 (33.3) | 1 | 1 | ||
| Student | 144 (25.9) | 108 (75.0) | 2.034 (0.89–4.61) | 0.089 | 1.70 (0.80–3.61) | 0.167 |
| Farmer/laborer | 105 (18.9) | 76 (72.4) | 0.973 (0.46–2.02) | 0.942 | 0.99 (0.48–2.01) | 0.984 |
| Private sector employee | 87 (15.6) | 51 (58.6) | 1.09 (0.49–2.40) | 0.830 | 1.14 (0.53–2.43) | 0.723 |
| Others | 125 (22.4) | 89 (71.2) | 1.161 (0.54–2.45) | 0.697 | 1.14 (0.55–2.34) | 0.721 |
| Religion | ||||||
| Christian | 477 (85.6) | 299 (62.7) | 1 | |||
| Islam | 75 (13.5) | 55 (73.3) | 2.083 (0.14–29.64) | 0.588 | ||
| Catholic | 5 (0.9) | 2 (40.0) | 1.247 (0.08–18.59) | 0.873 | ||
| Marital status | ||||||
| Single | 299 (53.7) | 203 (67.9) | 1 | 1 | ||
| Married | 258 (46.3) | 153 (59.3) | 1.442 (0.77–2.67) | 0.245 | 1.349 (0.73–2.46) | 0.329 |
| Economic status | ||||||
| Poor | 306 (54.9) | 213 (69.6) | 1 | |||
| Vulnerable | 142 (25.5) | 88 (62.0) | 0.956 (0.29–3.11) | 0.941 | ||
| Aspiring middle class | 85 (15.3) | 45 (52.9) | 0.645 (0.19–2.15) | 0.472 | ||
| Middle/upper class | 24 (4.3) | 10 (41.7) | 0.64 (0.19–2.15) | 0.471 | ||
| Knowledge towards COVID-19 vaccine | ||||||
| Good | 212 (38.1) | 99 (46.7) | 1 | 1 | ||
| Poor | 345 (61.9) | 257 (74.5) | 1.978 (1.26–3.08) | 0.003 | 2.171 (1.41–3.34) | 0.000 |
| Willingness to pay | ||||||
| No | 445 (79.9) | 332 (74.6) | 1 | 1 | ||
| Yes | 112 (20.1) | 24 (21.4) | 0.107 (0.061–0.19) | 0.000 | 0.118 (0.07–0.20) | 0.000 |
| Source of information | ||||||
| Social media | 271 (48.7) | 187 (69.0) | 1 | |||
| TV and newspaper | 230 (41.3) | 139 (60.4) | 0.372 (0.04–2.90) | 0.345 | ||
| Friends | 18 (3.2) | 15 (83.3) | 0.359 (0.04–2.78) | 0.327 | ||
| Health worker | 33 (5.9) | 12 (36.4) | 0.244 (0.02–2.81) | 0.258 | ||
| None | 5 (0.9) | 3 (60.0) | 1.003 (0.11–8.67) | 0.998 | ||
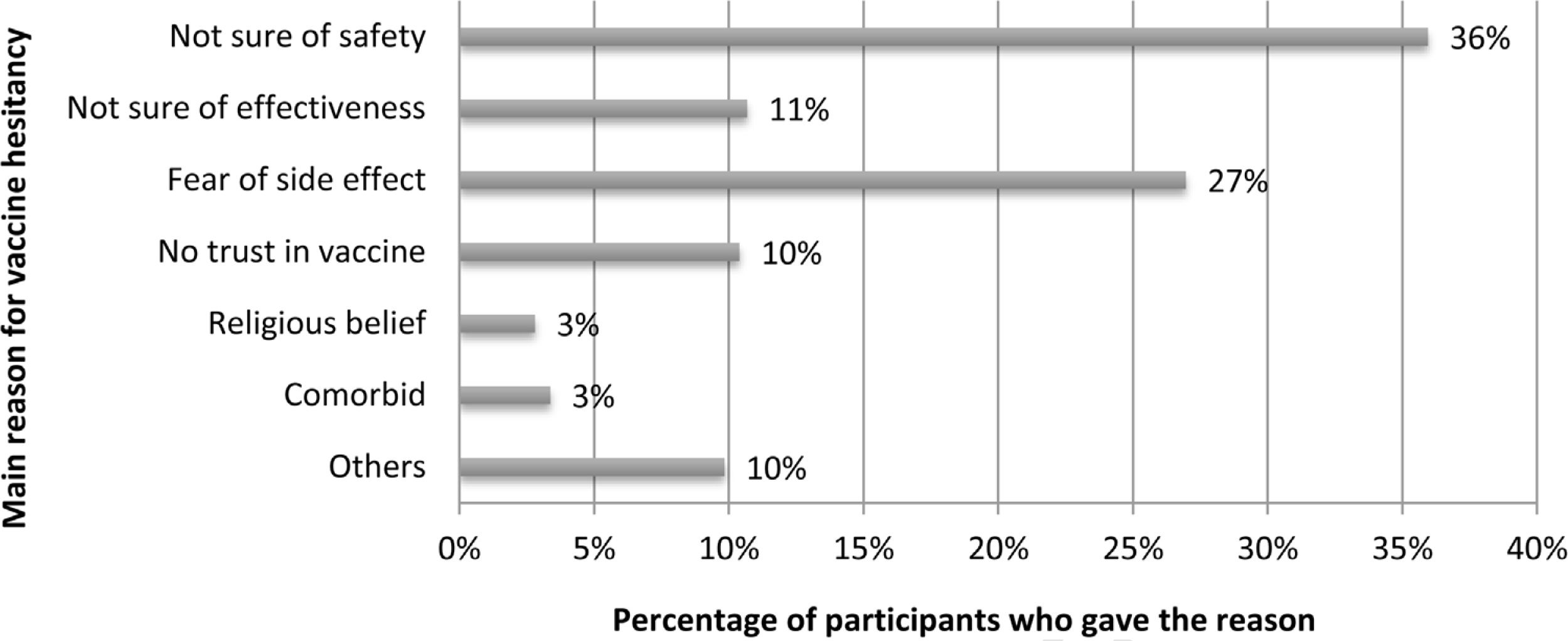
Of the total respondents who stated their hesitancy/refusal towards the SARS-CoV-2 vaccine (n = 356), the majority of the reasons given were ‘not sure of safety’ (36%) and ‘fear of side effects’ (27%; Fig. 1).
Qualitative partIn this study, 30 participants were interviewed, and data saturation occurred in all participants. All participants were domiciled in Sangihe Island District, with ages 22–64 years, with the highest level of education being high school education, and the majority of respondents worked as housewives. Participants consisted of 17 women (13 men), and all participants were Sangihe people. Of all participants interviewed, 22 refused to get vaccinated/were doubtful about vaccination, and 8 participants had received the vaccination (Table 2).
Basic descriptive statistics of interviewee characteristics.
| Characteristics | n | % |
|---|---|---|
| Mean age (SDa) | 45.37 (10.8) | |
| Age | ||
| 22–35 | 5 | 16.7 |
| 36–45 | 12 | 40.0 |
| >45 | 13 | 43.3 |
| Education | ||
| Primary/junior school | 5 | 16.7 |
| Senior high school | 17 | 56.7 |
| Diploma/university | 8 | 26.7 |
| Gender | ||
| Male | 12 | 40.0 |
| Female | 18 | 60.0 |
| Occupation | ||
| Civil servant | 2 | 6.7 |
| Housewife | 16 | 53.3 |
| Farmer/laborer | 6 | 20.0 |
| Private sector employee | 4 | 13.3 |
| Others | 2 | 6.7 |
| Acceptance towards COVID-19 vaccine | ||
| Yes | 8 | 26.7 |
| No | 18 | 60.0 |
| Undecided | 4 | 13.3 |
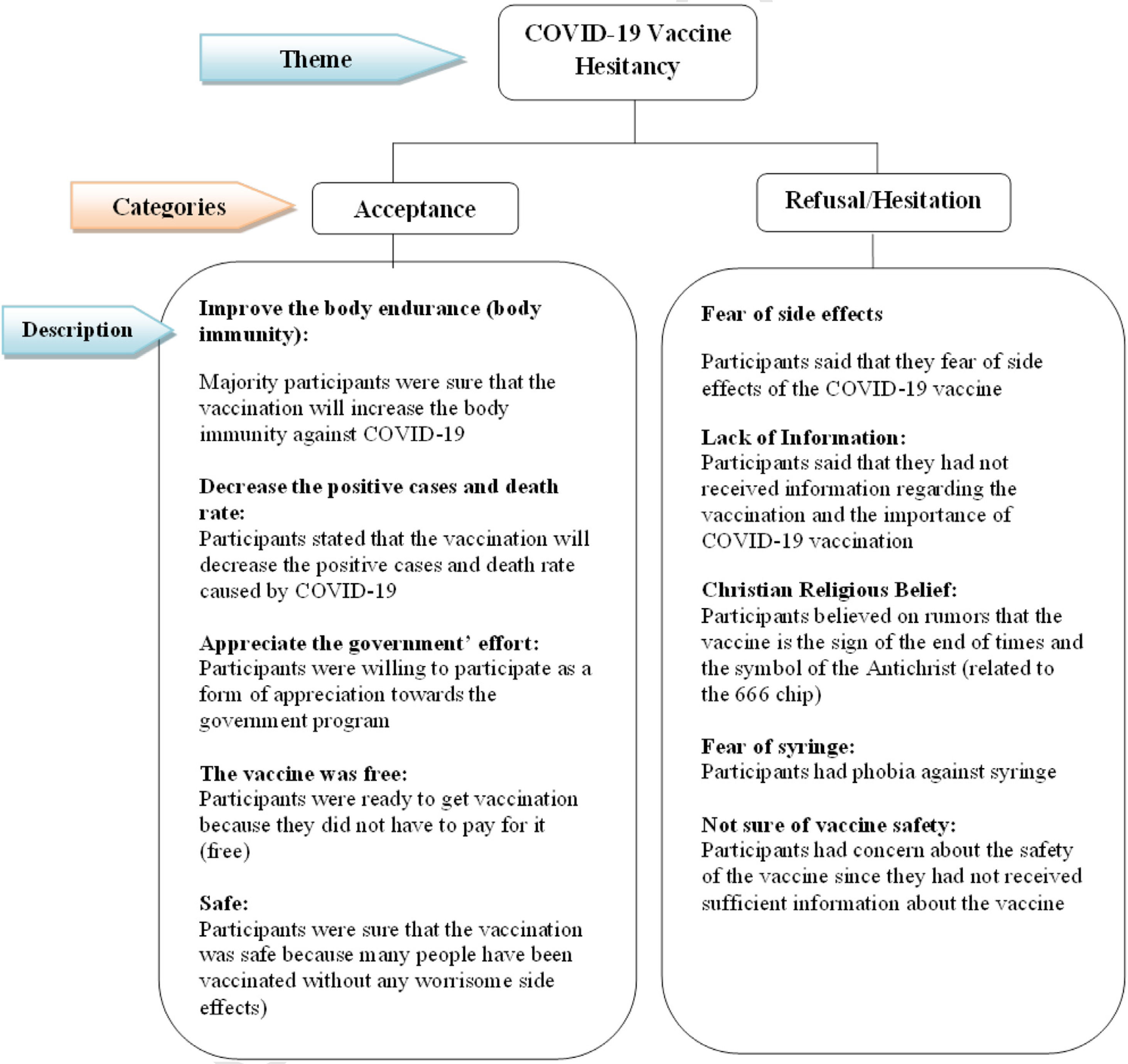
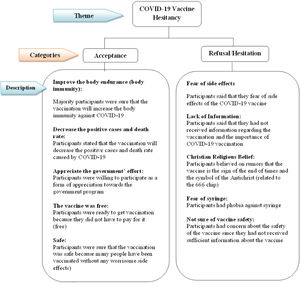
Fig. 2 shows the respondents’ perceptions of the SARS-CoV-2 vaccination. From the results of in-depth interviews, people’s perceptions of vaccination were divided into two categories, namely accepting and rejecting/doubting the vaccination. Both categories can be a supporting and an inhibiting factor in the vaccination process. Based on quotations from respondents who were willing to get vaccinated, the majority thought that vaccines would increase immunity, be safe, be free and reduce cases, and they appreciated the government’s efforts. ‘I am willing (to get the vaccination)… that’s a good (effort) anyway, if there is a vaccine, it means we are already protected from the virus…. It’s safe to go anywhere if there is a vaccine; you just have to follow the protocol, although you have already been vaccinated’. (P2) ‘The important thing is that (as long as the vaccination) is free and safe, I am willing to be vaccinated’. (P19) ‘If you have to (get the vaccine), you have to be willing to for your safety…. Instead of living like this—living with a mask (at all times) and the pandemic won’t go away (if you don’t get vaccinated). So for our safety, let’s get vaccinated. Besides, if there is a free vaccination, why not’? (P3)
Fig. 2 also shows respondents’ reasons for hesitating/refusing vaccination. The majority of responses from almost all respondents who refused the vaccination complained about the lack of information regarding the SARS-CoV-2 vaccination. Other reasons were related to side effects, religious beliefs, safety and fear of syringes. ‘I am not yet ready to be vaccinated; I don’t know how this vaccination will be conducted, about its safety and the side effects…even though it’s free, but if it’s not ready, I still don’t want to. I will just keep wearing my mask (to prevent the virus spreading)’. ‘I’m not ready to be vaccinated because I don’t know what the vaccine is. If I am asked for vaccination, I will not be fully ready….Well, maybe there should be socialisation or education from health workers about the vaccination first to the public so that people will know what this vaccination is all about’. (P13) ‘(I am) not willing to be vaccinated because some people say that there is a microchip in the vaccine, maybe (this is the program from) the antichrist…(the respondent smiles). I read in the Book of Revelation about the antichrist that the sign of the antichrist is the presence of a chip. Then, I heard the news on TV that the vaccine also has a chip…(the respondent chuckles)’. (P16) ‘…because the information concerning this vaccine circulating in the community is still lacking (I am not willing to be vaccinated), only when there is more information about the vaccine, then (I will consider that) it’s safe to be vaccinated, and I will be willing (to get one; The respondent showed his confused facial expression) but I still have doubt (about the vaccination)….’ ‘The health workers said that the vaccination is good (for your health), but I don’t want to be vaccinated because I’m still afraid of the syringe’ (P17).
The prevalence of vaccine hesitancy against the SARS-CoV-2 vaccine was found to be 63.9% (95% CI: 59.8%–67.9%). Previous studies demonstrated that vaccine hesitancy in urban areas in Indonesia was 35.2%8 and was almost the same as other studies in Indonesia that used the 50% vaccine effectiveness scenario with a vaccine hesitancy of 33.0%.7 Both studies were conducted at a time when the SARS-CoV-2 vaccine was still in the development stage. Vaccine hesitancy in general studies across various countries has been in the range of 12%–18%.15,16,17 Apart from the general population, SARS-CoV-2 vaccine hesitancy has also been found in health workers.18,19 The much higher prevalence of SARS-CoV-2 vaccine hesitancy in this study compared to previous studies is somewhat surprising. This is because this study was conducted at a time when the vaccination campaign was being carried out by the government, and the president, and other influencers subsequently, had already received the first injection of the vaccine, an event broadcast live on national TV. The differences are mainly due to the study population and a social context where participants’ access to information was very limited. These findings are of serious concern, as the government is trying to ensure widespread SARS-CoV-2 vaccination in all regions of Indonesia. Another possibility is the efficacy of the SINOVAC vaccine (63%). Previous research found that if the vaccine is 95% effective, 93.3% of participants would like to be vaccinated when the vaccine is provided for free by the government. However, this percentage decreases to 67.0% if vaccine efficacy is 50%.
A multivariate analysis (adjusted analysis) was performed to determine factors related to vaccine hesitancy. There are three factors associated with vaccine hesitancy, including the level of education, knowledge of the SARS-CoV-2 infection vaccination and willingness to pay. The higher the education, the less likely it is for vaccine refusal. These results are supported by the findings of other studies where education level is one of the factors related to vaccine hesitancy.16,20
This study proves that participants who do not have sufficient knowledge of the SARS-CoV-2 vaccination are twice as likely to refuse the vaccination compared to participants who have good knowledge, which is similar to the findings of other studies.15,21,22 There is no study regarding knowledge of COVID-19 vaccination in the first month of vaccination for the general population (January to February 2021) in Indonesia. However, from a study in Malaysia conducted at the end of 2020, it was found that 62% of respondents had poor knowledge of the COVID-19 vaccine.23 Access to information is very limited in rural areas, which causes people to not get comprehensive information regarding the SARS-CoV-2 vaccination. Therefore, the role of the local government in socialisation and education related to vaccination is very much needed. The increased knowledge is effective in increasing immunization coverage.24
A previous study found that 21.6% of rural residents were willing to pay for the vaccination. The willingness to pay for the vaccination in that study was related to income.25 This figure is not significantly different from the findings of this study, in which the proportion of rural residents willing to pay for the vaccination was 20.1% (Table 1). In this study, the willingness to pay was one of the factors that influenced a person to accept or refuse the vaccination. This means that people who are not willing to pay for vaccines will tend to refuse vaccination. This may be related to the fact that the majority of participants in this study fell into the category of poor economic status. This is also supported by research that found that families with lower incomes are more likely to refuse vaccination.14,26 Therefore, the Indonesian government’s decision to provide the COVID-19 vaccination for free to all populations in Indonesia is very appropriate and should encourage a higher vaccination rate.27
In this study, information on the reasons for receiving or refusing vaccination was extracted both qualitatively and quantitatively. Based on the quantitative results, the reasons for rejecting the vaccination from the largest to the smallest proportions included doubt of its safety, fear of side effects, doubt of its effectiveness, no trust in the vaccination, religious beliefs and comorbidities.
Meanwhile, based on the results of in-depth interviews (qualitative data), two categories of vaccine acceptance were found, namely acceptance and refusal/hesitation. The majority of respondents refused the vaccination. Lack of information related to the vaccination and the importance of vaccination were the reasons most participants cited for rejecting the vaccination. These results are in line with the quantitative results where vaccine-related knowledge is one of the factors associated with hesitancy towards vaccination. Meanwhile, the most cited reason for receiving the vaccine was that the vaccination can increase the body's immunity against SARS-CoV-2.
The reason for vaccine refusal that cannot be revealed from the quantitative results is the factor of Christian religious belief. Some participants believed circulated rumours that there is a microchip in the vaccine that is a symbol of the Antichrist. In a previous study in Indonesia, measles vaccination was also associated with Muslim religious beliefs where the vaccination coverage for the Muslim population was lower due to the presence of haram in the vaccine.28 However, the SARS-CoV-2 vaccine has been declared halal by the Indonesian Ulama Council, so it is not one of the reasons for vaccine rejection in this study. Rejection based on unfounded rumours about a microchip in the SARS-CoV-2 vaccine is not surprising. A theologian from Indonesia even conducted a study to refute this rumour.29 In a previous study in Jordan, it was found that high vaccine hesitancy was associated with the belief of the conspiracy that the SARS-CoV-2 vaccination would implant a microchip into a person’s body to control the person’s movements.30 Of course, further studies are needed to determine the relationship between local Christian religious beliefs and the hesitancy towards SARS-CoV-2 vaccination. However, the findings of this study can become a serious concern for religious leaders, especially in Christian-majority areas such as the study area. Local governments can support Christian religious leaders to straighten out information related to rumours of microchips in the SARS-CoV-2 vaccination.
The adopted sequential explanatory mixed methods are the strength of this study. This study provides more comprehensive data, as it explored reasons for doubt/refusal against vaccination to facilitate recommendations for targeted interventions to increase the rate of COVID-19 vaccination. The limitation of this study lies in the sampling method that used non-probability sampling, so there is the potential of sampling bias.
ConclusionMost residents in rural areas refused/were doubtful towards the SARS-CoV-2 vaccination (63.9%). Education level, vaccine-related knowledge and willingness to pay were found to be predictive factors towards vaccine hesitancy. The reasons for refusing/hesitating are doubt regarding the safety and effectiveness of the vaccine, fear of the side effects, lack of trust in the vaccination and Christian religious beliefs. Health workers and local religious leaders can be trained to provide education to reach the public directly regarding the safety and importance of the SARS-CoV-2 vaccination. Local government regulation on the obligation to vaccinate can be another solution to vaccination problems. Thus, the hope of achieving vaccination coverage for 181 million Indonesians can be realised.
Conflicts of interestThe authors have declared that no competing interest exists.
The authors thank all the participants involved in this study for their cooperation and support.